PRIMOLUT N Tablet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Guidelines for the Management of Heavy Menstrual Bleeding
i GUIDELINES FOR THE MANAGEMENT OF HEAVY MENSTRUAL BLEEDING Prepared by a Working Party on behalf of the National Health Committee ii MAY 1998 Women reporting with heavy menstrual bleeding 50% of women have menstrual blood loss Full menstrual history ● Examination ● Full blood count note1 Yes Prolonged irregular cycles No Refer Yes Abnormal exam specialist uterine size >12wks note 2 No mild or severe anaemic moderate treat < 80 g/l (80-115g/l) anaemia No Assess risk of endometrial hyperplasia low Offer medical therapy ● risk Unexplaine bodyweight 90kg heavy menstrual ● note5 note 6 age 45 years <2% bleeding ● other risk factors have 90% of women note 3 ● levonorgestrel endometrial >8% have hyperplasia intrauterine system ● tranexamic acid ● Assess endometrium nonsteroidal ● transvaginal ultrasound antiinflammatory agents ● (TVS) norethisterone long course or normal ● oc pill endometrium ● ● endometrial biopsy if danazol if one medical therapyfails endometrium 12mm others can be used note 7 or if TVS not available note 4 Treatment Hyperplastic endometrium success? or carcinoma No Yes Refer to specialist for hysteroscopic evaluation Continue Refer specialist me d i c a l for surgery therapy note8 note9 iii note 1 O In women <20 years old pelvic examination is unlikely to contribute to management of heavy bleeding (C) and the likelihood of pathology is small (C) O Increased likelihood (70%) of heavy menstrual blood loss >80mls/cycle if Hb <120g/l (A) O Consider pictorial blood loss assessment charts (appendix 6.5) for women with normal -
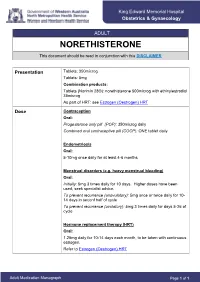
NORETHISTERONE This Document Should Be Read in Conjunction with This DISCLAIMER
King Edward Memorial Hospital Obstetrics & Gynaecology ADULT NORETHISTERONE This document should be read in conjunction with this DISCLAIMER Presentation Tablets: 350microg Tablets: 5mg Combination products: Tablets (Norimin 28®): norethisterone 500microg with ethinylestradiol 35microg As part of HRT: see Estrogen (Oestrogen) HRT Dose Contraception Oral: Progesterone only pill (POP): 350microg daily Combined oral contraceptive pill (COCP): ONE tablet daily Endometriosis Oral: 5-10mg once daily for at least 4-6 months Menstrual disorders (e.g. heavy menstrual bleeding) Oral: Initially: 5mg 3 times daily for 10 days. Higher doses have been used; seek specialist advice. To prevent recurrence (anovulatory): 5mg once or twice daily for 10- 14 days in seconf half of cycle To prevent recurrence (ovulatory): 5mg 3 times daily for days 5-26 of cycle Hormone replacement therapy (HRT) Oral: 1.25mg daily for 10-14 days each month, to be taken with continuous estrogen. Refer to Estrogen (Oestrogen) HRT Adult Medication Monograph Page 1 of 1 Norethisterone – Adult Administration Oral To be taken at the same time each day (or within 3 hours of the usual dose time). For Contraception: Start 4 weeks after the birth of baby (increased risk of abnormal vaginal bleeding if started earlier) Pregnancy 1st Trimester: Contraindicated 2nd Trimester: Contraindicated 3rd Trimester: Contraindicated Breastfeeding Considered safe to use. Progestogens are the preferred hormonal contraceptives as they do not inhibit lactation. Clinical Guidelines Estrogen (Oestrogen) HRT and Policies Progesterone Only Pill Contraception: Post Partum Gynaecology (Non-Oncological) Australian Medicines Handbook. Norethisterone. In: Australian References Medicines Handbook [Internet]. Adelaide (South Australia): Australian Medicines Handbook; 2017 [cited 2017 Apr 12]. -

Nur-Isterate Injection
SELECT THE REQUIRED INFORMATION PROFESSIONAL INFORMATION PATIENT INFORMATION LEAFLET SCHEDULING STATUS: S4 PROPRIETARY NAME AND DOSAGE FORM: NUR-ISTERATE Oily solution for intramuscular injection COMPOSITION: 1 ml contains norethisterone enantate (17-ethinyl-17-heptanoyloxy-4-estrene-3-one) 200 mg. Other ingredients are: benzyl benzoate, castor oil for injection. PHARMACOLOGICAL CLASSIFICATION: A. 21.8.2 Progesterones without estrogens. PHARMACOLOGICAL ACTION: Pharmacodynamic properties: Protection against conception is based primarily upon an alteration of the cervical mucous. This alteration is present for the whole of the duration of action and prevents the ascent of the sperm into the uterine cavity. Radioimmunological studies have shown that, during the first 5 to 7 weeks after injection, ovulation is suppressed as a result of the high plasma level of norethisterone. In addition, NUR- ISTERATE causes morphological changes in the endometrium which have the effect of rendering nidation of a fertilised egg difficult. Pharmacokinetic properties: Norethisterone enantate was completely absorbed after intramuscular injection. The ester was eventually completely hydrolysed to its pharmacologically active compound norethisterone once it was released from the depot. Maximum levels of norethisterone were measured at about 3 to 10 days after IM administration. They amounted on average to 13.4 5.4 ng/ml and 12.2 2.7 ng/ml about 7 days (median) after IM administration of 200 mg norethisterone enantate in 2 ml and 1 ml oily solution, respectively. Plasma levels of norethisterone declined in two disposition phases with half-lives of 4 to 5 days and 15 to 20 days, respectively, which were due to a biphasic release of norethisterone enantate from the depot. -

Polycystic Ovarian Syndrome
Polycystic Ovarian Syndrome What we understand and how we can help October 2017 Presentation Title | 27 January 2014 History Stein and Leventhal 1935 Stein IF, Leventhal ML. Amenorrhoea associated with bilateral polycystic ovaries. Am J Obstet Gynaecol 1935; 29:181-191 Presentation Title | 7 January, 2019 Presentation Title | 7 January, 2019 Diagnosis Rotterdam criteria – Two of the three criteria 1. PCOS on USS 2. Oligo or anovulation (less than 6 periods each year) 3. Hyperandrogenism Presentation Title | 7 January, 2019 Presentation Title | 7 January, 2019 Diagnosis – ovarian morphology PCO ultrasound appearance in 22% of normal population PCOS is present in • 7% of women • 32% of women with amenorrhoea • 87% of women with hirsuitism/ acne • 73% of women with anovulatory infertility Presentation Title | 7 January, 2019 Diagnostic tests The biochemical tests are to identify hyperandrogenism… Testosterone Can be measured at any time during the cycle. Consider testosterone secreting tumour if rapid virilisation. Consider High total testosterone or normal total testosterone with low SHBG and high bio-testosterone (measure the free androgen index) GTT All PCOS women who are obese and all women PCOS women over the age of 40. LH and FSH AMH Ovarian reserve and number of antral follicles. – may be raised in PCOS, however not currently used in diagnsois. Presentation Title | 7 January, 2019 Presentation Title | 7 January, 2019 Managing Symptoms Presentation Title | 7 January, 2019 Obesity Supportive strategies for weight loss and diet. Consider Metformin Bariatric surgery Presentation Title | 7 January, 2019 Hirsuitism and Acne Weight loss Cosmetic methods Oral contraceptive pill consider Yasmin as it has an antiandrogenic action. -

Study on Sperm Suppression Using Norethisterone Enanthate and Testosterone Undecanoate
Study on sperm suppression using Norethisterone enanthate and testosterone undecanoate Objectives Overall goal: and The study was designed to address the following primary objectives: Background 1. The rate of suppression of spermatogenesis induced by a regimen of NET-EN and TU administered every 8 weeks for up to 4 injection visits; and 2. The level of contraceptive protection provided by the continued administration of NET-EN and TU every 8 weeks for an efficacy period of up to 56 weeks. Background: The study was designed to evaluate whether the combination of a progestin, norethisterone enantate (NET-EN), and an androgen, testosterone undecanoate (TU), represents a safe and effective method of male fertility regulation. The study had 3 phases. The suppression phase was to initiate a status of decreased sperm count and activity to a level which would be considered as contraceptive. When this was reached it was sustained with subsequent injections in the efficacy phase, which would end after 56 weeks, or if a pregnancy occurs. After these, the participant was then placed in the recovery phase, and was observed until normal sperm counts and activity returns to normal. 487 participants were screened for eligibility, of which 167 were excluded. The remaining 320 were enrolled into the study, into the suppression phase. A total of 274 completed the suppression phase. Of these 8 discontinued before transitioning to the Efficacy phase, and were moved to recovery phase. A total of 266 transitioned to the efficacy phase, among which 111 completed 56 weeks follow up or until a pregnancy occurred. The remaining 155 were discontinued, either because of the stopping of the study by the sponsor (96), death (1, unrelated to the study), or for other reasons (58). -

Other Data Relevant to an Evaluation of Carcinogenicity and Its Mechanisms
COMBINED ESTROGEN−PROGESTOGEN CONTRACEPTIVES 143 4. Other Data Relevant to an Evaluation of Carcinogenicity and its Mechanisms 4.1 Absorption, distribution, metabolism and excretion in humans The metabolism and disposition of various formulations of oral contraceptives used in humans differ. After entering the small intestine, estrogenic and progestogenic compounds in combined oral contraceptives undergo metabolism by bacterial enzymes and enzymes in the intestinal mucosa to varying extents. The mixture of metabolized and unmetabolized compounds then undergoes intestinal absorption, and thus enters the portal vein blood, which perfuses the liver. In the liver, the compounds can be metabolized extensively, which leads to variations in the amount of active drug. A fraction of the absorbed dose of ethinyl- estradiol and some progestogens is also excreted in the bile during its first transit through the liver. Although some of these compounds are partially reabsorbed via the enterohepatic circulation, a fraction may also be excreted in this ‘first pass’, which reduces overall bio- availability. Since steroids penetrate normal skin easily, various systems have also been developed that deliver estrogens and progestogens parenterally, e.g. transdermal patches, nasal sprays, subcutaneous implants, vaginal rings and intrauterine devices (Fanchin et al., 1997; Dezarnaulds & Fraser, 2002; Meirik et al., 2003; Sarkar, 2003; Wildemeersch et al., 2003; Sturdee et al., 2004). These different modes of administration have been described previously (IARC, 1999). In general, all parenteral routes avoid loss of the drug by hepatic first-pass metabolism and minimally affect hepatic protein metabolism. The absorption rates of orally administered estrogens and progestogens are usually rapid; peak serum values are observed between 0.5 and 4 h after intake. -
Steroidal Estrogens
FINAL Report on Carcinogens Background Document for Steroidal Estrogens December 13 - 14, 2000 Meeting of the NTP Board of Scientific Counselors Report on Carcinogens Subcommittee Prepared for the: U.S. Department of Health and Human Services Public Health Service National Toxicology Program Research Triangle Park, NC 27709 Prepared by: Technology Planning and Management Corporation Canterbury Hall, Suite 310 4815 Emperor Blvd Durham, NC 27703 Contract Number N01-ES-85421 Dec. 2000 RoC Background Document for Steroidal Estrogens Do not quote or cite Criteria for Listing Agents, Substances or Mixtures in the Report on Carcinogens U.S. Department of Health and Human Services National Toxicology Program Known to be Human Carcinogens: There is sufficient evidence of carcinogenicity from studies in humans, which indicates a causal relationship between exposure to the agent, substance or mixture and human cancer. Reasonably Anticipated to be Human Carcinogens: There is limited evidence of carcinogenicity from studies in humans which indicates that causal interpretation is credible but that alternative explanations such as chance, bias or confounding factors could not adequately be excluded; or There is sufficient evidence of carcinogenicity from studies in experimental animals which indicates there is an increased incidence of malignant and/or a combination of malignant and benign tumors: (1) in multiple species, or at multiple tissue sites, or (2) by multiple routes of exposure, or (3) to an unusual degree with regard to incidence, site or type of tumor or age at onset; or There is less than sufficient evidence of carcinogenicity in humans or laboratory animals, however; the agent, substance or mixture belongs to a well defined, structurally-related class of substances whose members are listed in a previous Report on Carcinogens as either a known to be human carcinogen, or reasonably anticipated to be human carcinogen or there is convincing relevant information that the agent acts through mechanisms indicating it would likely cause cancer in humans. -

Norethisterone 5Mg Tablets
Norethisterone 5mg tablets • an inherited disorder of the red blood pigment haemoglobin (porphyria) • severe itching coding area • had cancer of the breast or genital tract (unless Norethisterone tablets are given as part of a cancer treatment programme). Check with your doctor or pharmacist before taking Norethisterone tablets if you have: • not had a period before starting a new course of norethisterone (it must be confirmed you are not pregnant) • diabetes Read all of this leaflet carefully before you start taking • epilepsy, migraine, asthma, kidney or heart problems this medicine. (norethisterone may cause fluid retention which can • Keep this leaflet. You may need to read it again. aggravate these conditions). • If you have any further questions, ask your doctor Taking other medicines or pharmacist. Please tell your doctor or pharmacist if you are taking or • This medicine has been prescribed for you. have recently taken any other medicines, including medicines Do not pass it on to others. It may harm them, obtained without a prescription. Especially: even if their symptoms are the same as yours. • other hormonal products (oestrogens or progestogens) • medicines used to treat epilepsy (e.g. phenobarbital, Index phenytoin, carbamazepine) 1 What Norethisterone tablets are • medicines used to treat infections (e.g. rifampicin, and what they are used for nevirapine, tetracyclines, ampicillin, oxacillin, co- 2 Before you take trimoxazole, ritonavir, nelfinavir) 3 How to take • St John’s Wort (hypericum perforatum-a herbal remedy) • aminoglutethimide 4 Possible side effects • ciclosporin (to prevent transplant rejection) 5 How to store • other medicines which can also cause fluid retention 6 Further information such as anti-inflammatory medicines (e.g. -

PRAC Recommendations on Signals October 2018
29 October 20181 EMA/PRAC/689235/2018 Pharmacovigilance Risk Assessment Committee (PRAC) PRAC recommendations on signals Adopted at the 1-4 October 2018 PRAC meeting This document provides an overview of the recommendations adopted by the Pharmacovigilance Risk Assessment Committee (PRAC) on the signals discussed during the meeting of 1-4 October 2018 (including the signal European Pharmacovigilance Issues Tracking Tool [EPITT]2 reference numbers). PRAC recommendations to provide supplementary information are directly actionable by the concerned marketing authorisation holders (MAHs). PRAC recommendations for regulatory action (e.g. amendment of the product information) are submitted to the Committee for Medicinal Products for Human Use (CHMP) for endorsement when the signal concerns Centrally Authorised Products (CAPs), and to the Co-ordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh) for information in the case of Nationally Authorised Products (NAPs). Thereafter, MAHs are expected to take action according to the PRAC recommendations. When appropriate, the PRAC may also recommend the conduct of additional analyses by the Agency or Member States. MAHs are reminded that in line with Article 16(3) of Regulation No (EU) 726/2004 and Article 23(3) of Directive 2001/83/EC, they shall ensure that their product information is kept up to date with the current scientific knowledge including the conclusions of the assessment and recommendations published on the European Medicines Agency (EMA) website (currently acting as the EU medicines webportal). For CAPs, at the time of publication, PRAC recommendations for update of product information have been agreed by the CHMP at their plenary meeting (17-20 October 2018) and corresponding variations will be assessed by the CHMP. -

Biological Efficacy and Plasma Norethisterone Levels of Orally Administered Norethisterone Enanthate in Rat and Hamster
Indian J Physiol Pharmacol 1998; 42 (4) : 485-490 BIOLOGICAL EFFICACY AND PLASMA NORETHISTERONE LEVELS OF ORALLY ADMINISTERED NORETHISTERONE ENANTHATE IN RAT AND HAMSTER P. RAVINDER, K. MADHAVAN NAIR AND B. SIVAKUMAR* Division of Biophysics. National Institute of Nutrition. (Indian Council of Medical Research) Jamai-Osmania, Hyderabad - 500 007 (Received on September 11, 1997) Abstract: Norethisterone enanthate (NET-En) is a well known intramuscular contraceptive drug. The long acting nature of this prep~ration when administered orally was evalu~ted in female rats and hamsters using fertility inhibition test and from the plasma levels of norethisterone (NET). An oral dose of 20-60 mg NET-En was administered to random groups of six female rats and hamsters and were mated after five and ten days with males of proven fertility. The fertility inhibition rate was determined from vaginal delivery. A dose-dependent reduction in fertility was seen in rats 5 days after oral administration of NET-En. This effect was found to be less pronounced and not significant 10 days after administration of similar doses of NET-En. In hamsters, a similar but less pronounced effect was noted. The decrease in fertility was significant only at the 60 mg dose. The plasma levels of NET estimated by RIA over a period of 15 days, in a different set of treated rats, suggested rapid absorption of NET-En within a day, and drug concentration decreased slowly, the levels on the 4th day ranged from 0.9-2.3 with the 10 mg and 1.0-4.0 ng/ml with the 20 mg dose. -

Norethisterone(BAN, Pinn)
Nandrolone/Norethisterone 2119 fluid retention or adverse effect on renal function or serum-lipids. Pharmacopoeias. In Eur. (see p.vii). Mex.: Evra; Neth.: Evra; Norw.: Evra; Philipp.: Evra; Pol.: Evra; Port.: In these reports, intramuscular doses of nandrolone decanoate Ph. Eur. 6.2 (Nomegestrol Acetate). A white or almost white Evra; Rus.: Evra (Евра); S.Afr.: Evra; Singapore: Evra; Spain: Evra; Swed.: have ranged from 100 mg once every 2 weeks4 up to 600 mg crystalline powder. Practically insoluble in water; soluble in al- Evra; Switz.: Evra; Thai.: Evra; UK: Evra; USA: Ortho Evra; Venez.: Evra. weekly,2 and treatment has generally been given for 12 to 24 cohol; freely soluble in acetone. Protect from light. weeks. Profile Norethandrolone (BAN, rINN) ⊗ 1. Gold J, et al. Safety and efficacy of nandrolone decanoate for Nomegestrol acetate is a progestogen structurally related to pro- treatment of wasting in patients with HIV infection. AIDS 1996 17α-Ethyl-17β-hydroxyestr-4-en-3-one; 17β-Hydroxy-19-nor- 10: 745–52. gesterone (p.2125) that has been used in the treatment of men- 2. Sattler FR, et al. Effects of pharmacological doses of nandrolone strual disorders and as the progestogen component of menopau- 17α-pregn-4-en-3-one; Noretandrolona; Noréthandrolone; decanoate and progressive resistance training in immunodefi- sal HRT (p.2071). Typical oral doses are 5 mg daily for 10 to 14 Norethandrolonum. cient patients infected with human immunodeficiency virus. J days of a 28-day cycle. A subdermal implant is under investiga- Норэтандролон Clin Endocrinol Metab 1999; 84: 1268–76. tion as a long-acting progestogen-only contraceptive. -

Terms Moving from Scrs 2018 Mesh to Descriptors in 2019
Terms moving from SCRs 2018 MeSH to Descriptors in 2019 Term EntryTerm Moved Current UI Current Heading Moved To New MeSH New Heading Type From UI PrefTerm histone methyltransferase SCR C021362 histone methyltransferase Descriptor D000076983 Histone Methyltransferases EntryTerm Sugammadex sodium SCR C453980 Sugammadex Descriptor D000077122 Sugammadex EntryTerm Esmeron SCR C061870 rocuronium Descriptor D000077123 Rocuronium EntryTerm NSC 628503 SCR C067311 docetaxel Descriptor D000077143 Docetaxel EntryTerm RP-56976 SCR C067311 docetaxel Descriptor D000077143 Docetaxel EntryTerm Taxotere SCR C067311 docetaxel Descriptor D000077143 Docetaxel EntryTerm clopidogrel, (+)(S)-isomer SCR C055162 clopidogrel Descriptor D000077144 Clopidogrel EntryTerm Plavix SCR C055162 clopidogrel Descriptor D000077144 Clopidogrel EntryTerm sulfanilamide strontium salt SCR C036944 sulfanilamide Descriptor D000077145 Sulfanilamide EntryTerm sulfanilamide zinc salt SCR C036944 sulfanilamide Descriptor D000077145 Sulfanilamide EntryTerm Irrinotecan SCR C051890 irinotecan Descriptor D000077146 Irinotecan EntryTerm SN-38-11 SCR C051890 irinotecan Descriptor D000077146 Irinotecan EntryTerm cis-oxalato-(trans-l)-1,2-diaminocyclohexane-platinum(II) SCR C030110 oxaliplatin Descriptor D000077150 Oxaliplatin PrefTerm oxaliplatin SCR C030110 oxaliplatin Descriptor D000077150 Oxaliplatin EntryTerm oxaliplatin, (SP-4-2-(1S-trans))-isomer SCR C030110 oxaliplatin Descriptor D000077150 Oxaliplatin EntryTerm LY 170053 SCR C076029 olanzapine Descriptor D000077152 Olanzapine EntryTerm