Polycystic Ovarian Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download PDF File
Ginekologia Polska 2019, vol. 90, no. 9, 520–526 Copyright © 2019 Via Medica ORIGINAL PAPER / GYNECologY ISSN 0017–0011 DOI: 10.5603/GP.2019.0091 Anti-androgenic therapy in young patients and its impact on intensity of hirsutism, acne, menstrual pain intensity and sexuality — a preliminary study Anna Fuchs, Aleksandra Matonog, Paulina Sieradzka, Joanna Pilarska, Aleksandra Hauzer, Iwona Czech, Agnieszka Drosdzol-Cop Department of Pregnancy Pathology, Department of Woman’s Health, School of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland ABSTRACT Objectives: Using anti-androgenic contraception is one of the methods of birth control. It also has a significant, non-con- traceptive impact on women’s body. These drugs can be used in various endocrinological disorders, because of their ability to reduce the level of male hormones. The aim of our study is to establish a correlation between taking different types of anti-androgenic drugs and intensity of hirsutism, acne, menstrual pain intensity and sexuality . Material and methods: 570 women in childbearing age that had been using oral contraception for at least three months took part in our research. We examined women and asked them about quality of life, health, direct causes and effects of that treatment, intensity of acne and menstrual pain before and after. Our research group has been divided according to the type of gestagen contained in the contraceptive pill: dienogest, cyproterone, chlormadynone and drospirenone. Ad- ditionally, the control group consisted of women taking oral contraceptives without antiandrogenic component. Results: The mean age of the studied group was 23 years ± 3.23. 225 of 570 women complained of hirsutism. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -
Guidelines for the Management of Heavy Menstrual Bleeding
i GUIDELINES FOR THE MANAGEMENT OF HEAVY MENSTRUAL BLEEDING Prepared by a Working Party on behalf of the National Health Committee ii MAY 1998 Women reporting with heavy menstrual bleeding 50% of women have menstrual blood loss Full menstrual history ● Examination ● Full blood count note1 Yes Prolonged irregular cycles No Refer Yes Abnormal exam specialist uterine size >12wks note 2 No mild or severe anaemic moderate treat < 80 g/l (80-115g/l) anaemia No Assess risk of endometrial hyperplasia low Offer medical therapy ● risk Unexplaine bodyweight 90kg heavy menstrual ● note5 note 6 age 45 years <2% bleeding ● other risk factors have 90% of women note 3 ● levonorgestrel endometrial >8% have hyperplasia intrauterine system ● tranexamic acid ● Assess endometrium nonsteroidal ● transvaginal ultrasound antiinflammatory agents ● (TVS) norethisterone long course or normal ● oc pill endometrium ● ● endometrial biopsy if danazol if one medical therapyfails endometrium 12mm others can be used note 7 or if TVS not available note 4 Treatment Hyperplastic endometrium success? or carcinoma No Yes Refer to specialist for hysteroscopic evaluation Continue Refer specialist me d i c a l for surgery therapy note8 note9 iii note 1 O In women <20 years old pelvic examination is unlikely to contribute to management of heavy bleeding (C) and the likelihood of pathology is small (C) O Increased likelihood (70%) of heavy menstrual blood loss >80mls/cycle if Hb <120g/l (A) O Consider pictorial blood loss assessment charts (appendix 6.5) for women with normal -

The Mechanism of Androgen Actions in PCOS Etiology
medical sciences Review The Mechanism of Androgen Actions in PCOS Etiology Valentina Rodriguez Paris 1 and Michael J. Bertoldo 1,2,* 1 Fertility and Research Centre, School of Women’s and Children’s Health, University of New South Wales Sydney, NSW 2052, Australia 2 School of Medical Sciences, University of New South Wales Sydney, NSW 2052, Australia * Correspondence: [email protected] Received: 15 June 2019; Accepted: 20 August 2019; Published: 28 August 2019 Abstract: Polycystic ovary syndrome (PCOS) is the most common endocrine condition in reproductive-age women. By comprising reproductive, endocrine, metabolic and psychological features—the cause of PCOS is still unknown. Consequently, there is no cure, and management is persistently suboptimal as it depends on the ad hoc management of symptoms only. Recently it has been revealed that androgens have an important role in regulating female fertility. Androgen actions are facilitated via the androgen receptor (AR) and transgenic Ar knockout mouse models have established that AR-mediated androgen actions have a part in regulating female fertility and ovarian function. Considerable evidence from human and animal studies currently reinforces the hypothesis that androgens in excess, working via the AR, play a key role in the origins of polycystic ovary syndrome (PCOS). Identifying and confirming the locations of AR-mediated actions and the molecular mechanisms involved in the development of PCOS is critical to provide the knowledge required for the future development of innovative, mechanism-based interventions for the treatment of PCOS. This review summarises fundamental scientific discoveries that have improved our knowledge of androgen actions in PCOS etiology and how this may form the future development of effective methods to reduce symptoms in patients with PCOS. -
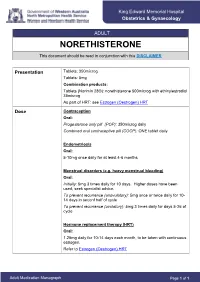
NORETHISTERONE This Document Should Be Read in Conjunction with This DISCLAIMER
King Edward Memorial Hospital Obstetrics & Gynaecology ADULT NORETHISTERONE This document should be read in conjunction with this DISCLAIMER Presentation Tablets: 350microg Tablets: 5mg Combination products: Tablets (Norimin 28®): norethisterone 500microg with ethinylestradiol 35microg As part of HRT: see Estrogen (Oestrogen) HRT Dose Contraception Oral: Progesterone only pill (POP): 350microg daily Combined oral contraceptive pill (COCP): ONE tablet daily Endometriosis Oral: 5-10mg once daily for at least 4-6 months Menstrual disorders (e.g. heavy menstrual bleeding) Oral: Initially: 5mg 3 times daily for 10 days. Higher doses have been used; seek specialist advice. To prevent recurrence (anovulatory): 5mg once or twice daily for 10- 14 days in seconf half of cycle To prevent recurrence (ovulatory): 5mg 3 times daily for days 5-26 of cycle Hormone replacement therapy (HRT) Oral: 1.25mg daily for 10-14 days each month, to be taken with continuous estrogen. Refer to Estrogen (Oestrogen) HRT Adult Medication Monograph Page 1 of 1 Norethisterone – Adult Administration Oral To be taken at the same time each day (or within 3 hours of the usual dose time). For Contraception: Start 4 weeks after the birth of baby (increased risk of abnormal vaginal bleeding if started earlier) Pregnancy 1st Trimester: Contraindicated 2nd Trimester: Contraindicated 3rd Trimester: Contraindicated Breastfeeding Considered safe to use. Progestogens are the preferred hormonal contraceptives as they do not inhibit lactation. Clinical Guidelines Estrogen (Oestrogen) HRT and Policies Progesterone Only Pill Contraception: Post Partum Gynaecology (Non-Oncological) Australian Medicines Handbook. Norethisterone. In: Australian References Medicines Handbook [Internet]. Adelaide (South Australia): Australian Medicines Handbook; 2017 [cited 2017 Apr 12]. -

Nur-Isterate Injection
SELECT THE REQUIRED INFORMATION PROFESSIONAL INFORMATION PATIENT INFORMATION LEAFLET SCHEDULING STATUS: S4 PROPRIETARY NAME AND DOSAGE FORM: NUR-ISTERATE Oily solution for intramuscular injection COMPOSITION: 1 ml contains norethisterone enantate (17-ethinyl-17-heptanoyloxy-4-estrene-3-one) 200 mg. Other ingredients are: benzyl benzoate, castor oil for injection. PHARMACOLOGICAL CLASSIFICATION: A. 21.8.2 Progesterones without estrogens. PHARMACOLOGICAL ACTION: Pharmacodynamic properties: Protection against conception is based primarily upon an alteration of the cervical mucous. This alteration is present for the whole of the duration of action and prevents the ascent of the sperm into the uterine cavity. Radioimmunological studies have shown that, during the first 5 to 7 weeks after injection, ovulation is suppressed as a result of the high plasma level of norethisterone. In addition, NUR- ISTERATE causes morphological changes in the endometrium which have the effect of rendering nidation of a fertilised egg difficult. Pharmacokinetic properties: Norethisterone enantate was completely absorbed after intramuscular injection. The ester was eventually completely hydrolysed to its pharmacologically active compound norethisterone once it was released from the depot. Maximum levels of norethisterone were measured at about 3 to 10 days after IM administration. They amounted on average to 13.4 5.4 ng/ml and 12.2 2.7 ng/ml about 7 days (median) after IM administration of 200 mg norethisterone enantate in 2 ml and 1 ml oily solution, respectively. Plasma levels of norethisterone declined in two disposition phases with half-lives of 4 to 5 days and 15 to 20 days, respectively, which were due to a biphasic release of norethisterone enantate from the depot. -

Receptor Af®Nity and Potency of Non-Steroidal Antiandrogens: Translation of Preclinical ®Ndings Into Clinical Activity
Prostate Cancer and Prostatic Diseases (1998) 1, 307±314 ß 1998 Stockton Press All rights reserved 1365±7852/98 $12.00 http://www.stockton-press.co.uk/pcan Review Receptor af®nity and potency of non-steroidal antiandrogens: translation of preclinical ®ndings into clinical activity GJCM Kolvenbag1, BJA Furr2 & GRP Blackledge3 1Medical Affairs, Zeneca Pharmaceuticals, Wilmington, DE, USA; 2Therapeutic Research Department, and 3Medical Research Department, Zeneca Pharmaceuticals, Alderley Park, Maccles®eld, Cheshire, UK The non-steroidal antiandrogens ¯utamide (Eulexin1), nilutamide (Anandron1) and bicalutamide (Casodex1) are widely used in the treatment of advanced prostate cancer, particularly in combination with castration. The naturally occurring ligand 5a-DHT has higher binding af®nity at the androgen receptor than the non-steroidal antiandrogens. Bicalutamide has an af®nity two to four times higher than 2-hydroxy¯utamide, the active metabolite of ¯utamide, and around two times higher than nilutamide for wild-type rat and human prostate androgen receptors. Animal studies have indicated that bicalutamide also exhi- bits greater potency in reducing seminal vesicle and ventral prostate weights and inhibiting prostate tumour growth than ¯utamide. Although preclinical data can give an indication of the likely clinical activity, clinical studies are required to determine effective, well-tolerated dosing regimens. As components of combined androgen blockade (CAB), controlled studies have shown survival bene®ts of ¯utamide plus a luteinising hormone-releasing hormone analogue (LHRH-A) over LHRH-A alone, and for nilutamide plus orchiectomy over orchiectomy alone. Other studies have failed to show such survival bene®ts, including those comparing ¯utamide plus orchiectomy with orchiectomy alone, and nilutamide plus LHRH-A with LHRH-A alone. -

Flutamide Capsules USP, 125 Mg
FLUTAMIDE- flutamide capsule Cipla USA Inc. ---------- Flutamide Capsules USP, 125 mg BOXED WARNING WARNINGS Hepatic Injury There have been postmarketing reports of hospitalization and rarely death due to liver failure in patients taking flutamide. Evidence of hepatic injury included elevated serum transaminase levels, jaundice, hepatic encephalopathy and death related to acute hepatic failure. The hepatic injury was reversible after discontinuation of therapy in some patients. Approximately half of the reported cases occurred within the initial 3 months of treatment with flutamide. Serum transaminase levels should be measured prior to starting treatment with flutamide. Flutamide is not recommended in patients whose ALT values exceed twice the upper limit of normal. Serum transaminase levels should then be measured monthly for the first 4 months of therapy, and periodically thereafter. Liver function tests also should be obtained at the first signs and symptoms suggestive of liver dysfunction, e.g., nausea, vomiting, abdominal pain, fatigue, anorexia, "flu-like" symptoms, hyperbilirubinuria, jaundice or right upper quadrant tenderness. If at any time, a patient has jaundice, or their ALT rises above 2 times the upper limit of normal, flutamide should be immediately discontinued with close follow-up of liver function tests until resolution. DESCRIPTION Flutamide capsules, USP contain flutamide, an acetanilid, nonsteroidal, orally active antiandrogen having the chemical name, α,α,α-Trifluoro-2-methyl-4'-nitro-m-propionotoluidide and has the following structural formula: C11H11F3N2O3 M.W. 276.21 Flutamide is a buff to yellow powder. Each capsule, for oral administration, contains 125 mg flutamide and has the following inactive ingredients: black iron oxide, corn starch, D&C yellow #10 aluminum lake, FD&C blue #1 aluminum lake, FD&C blue #2 aluminum lake, FD&C red #40 aluminum lake, gelatin, lactose monohydrate, magnesium stearate, red iron oxide, sodium lauryl sulfate, titanium dioxide and yellow iron oxide. -

Study on Sperm Suppression Using Norethisterone Enanthate and Testosterone Undecanoate
Study on sperm suppression using Norethisterone enanthate and testosterone undecanoate Objectives Overall goal: and The study was designed to address the following primary objectives: Background 1. The rate of suppression of spermatogenesis induced by a regimen of NET-EN and TU administered every 8 weeks for up to 4 injection visits; and 2. The level of contraceptive protection provided by the continued administration of NET-EN and TU every 8 weeks for an efficacy period of up to 56 weeks. Background: The study was designed to evaluate whether the combination of a progestin, norethisterone enantate (NET-EN), and an androgen, testosterone undecanoate (TU), represents a safe and effective method of male fertility regulation. The study had 3 phases. The suppression phase was to initiate a status of decreased sperm count and activity to a level which would be considered as contraceptive. When this was reached it was sustained with subsequent injections in the efficacy phase, which would end after 56 weeks, or if a pregnancy occurs. After these, the participant was then placed in the recovery phase, and was observed until normal sperm counts and activity returns to normal. 487 participants were screened for eligibility, of which 167 were excluded. The remaining 320 were enrolled into the study, into the suppression phase. A total of 274 completed the suppression phase. Of these 8 discontinued before transitioning to the Efficacy phase, and were moved to recovery phase. A total of 266 transitioned to the efficacy phase, among which 111 completed 56 weeks follow up or until a pregnancy occurred. The remaining 155 were discontinued, either because of the stopping of the study by the sponsor (96), death (1, unrelated to the study), or for other reasons (58). -

Other Data Relevant to an Evaluation of Carcinogenicity and Its Mechanisms
COMBINED ESTROGEN−PROGESTOGEN CONTRACEPTIVES 143 4. Other Data Relevant to an Evaluation of Carcinogenicity and its Mechanisms 4.1 Absorption, distribution, metabolism and excretion in humans The metabolism and disposition of various formulations of oral contraceptives used in humans differ. After entering the small intestine, estrogenic and progestogenic compounds in combined oral contraceptives undergo metabolism by bacterial enzymes and enzymes in the intestinal mucosa to varying extents. The mixture of metabolized and unmetabolized compounds then undergoes intestinal absorption, and thus enters the portal vein blood, which perfuses the liver. In the liver, the compounds can be metabolized extensively, which leads to variations in the amount of active drug. A fraction of the absorbed dose of ethinyl- estradiol and some progestogens is also excreted in the bile during its first transit through the liver. Although some of these compounds are partially reabsorbed via the enterohepatic circulation, a fraction may also be excreted in this ‘first pass’, which reduces overall bio- availability. Since steroids penetrate normal skin easily, various systems have also been developed that deliver estrogens and progestogens parenterally, e.g. transdermal patches, nasal sprays, subcutaneous implants, vaginal rings and intrauterine devices (Fanchin et al., 1997; Dezarnaulds & Fraser, 2002; Meirik et al., 2003; Sarkar, 2003; Wildemeersch et al., 2003; Sturdee et al., 2004). These different modes of administration have been described previously (IARC, 1999). In general, all parenteral routes avoid loss of the drug by hepatic first-pass metabolism and minimally affect hepatic protein metabolism. The absorption rates of orally administered estrogens and progestogens are usually rapid; peak serum values are observed between 0.5 and 4 h after intake. -

Medical Treatment of Hirsutism in Women F
2530 Current Medicinal Chemistry, 2010, 17, 2530-2538 Medical Treatment of Hirsutism in Women F. Lumachi*,1 and S.M.M. Basso2 1Department of Surgical and Gastroenterological Sciences; 21st School of General Surgery, University of Padua, School of Medicine, 35128 Padova, Italy Abstract: Hirsutism is the presence of excess hair growth in women in the typical male hair growth areas, thereby reflect- ing a deviation from the normal female hair pattern. It affects from 5% to 10% of women, depending on age, menopausal status and ethnic background. The presence of hirsutism is very distressing for women, and subsequently may have a negative impact on their psychosocial life. In the treatment of hirsutism several options are now available, including pharmacologic regimens and cosmetic measures. Both the hormonal profile of the patient and her expectations and prefer- ences should guide the therapeutic approach. The aims of the medical therapy are suppression of excessive androgen pro- duction, inhibition of peripheral action of androgens, and treatment of patients at risk for metabolic disorders or reproduc- tive cancers. For other diseases related to endocrine abnormalities, such as thyroid disorders or Cushing’s syndrome, spe- cific treatment is mandatory. After an ineffective local approach by direct hair removal, a pharmacological treatment should be suggested, using estrogen and progestin combinations, antiandrogens (i.e. cyproterone acetate, spironolactone) or both as a first line. Finasteride, gonadotropin-releasing hormone agonists, and glucocorticoids should be used in se- lected cases. Adequate contraception is also recommended if antiandrogens are used. Unfortunately, since systemic ther- apy reduces hair growth in less than 50% of cases, hirsute women frequently require cosmetic measures.