Study on Sperm Suppression Using Norethisterone Enanthate and Testosterone Undecanoate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pp375-430-Annex 1.Qxd
ANNEX 1 CHEMICAL AND PHYSICAL DATA ON COMPOUNDS USED IN COMBINED ESTROGEN–PROGESTOGEN CONTRACEPTIVES AND HORMONAL MENOPAUSAL THERAPY Annex 1 describes the chemical and physical data, technical products, trends in produc- tion by region and uses of estrogens and progestogens in combined estrogen–progestogen contraceptives and hormonal menopausal therapy. Estrogens and progestogens are listed separately in alphabetical order. Trade names for these compounds alone and in combination are given in Annexes 2–4. Sales are listed according to the regions designated by WHO. These are: Africa: Algeria, Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Cape Verde, Central African Republic, Chad, Comoros, Congo, Côte d'Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Eritrea, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Sao Tome and Principe, Senegal, Seychelles, Sierra Leone, South Africa, Swaziland, Togo, Uganda, United Republic of Tanzania, Zambia and Zimbabwe America (North): Canada, Central America (Antigua and Barbuda, Bahamas, Barbados, Belize, Costa Rica, Cuba, Dominica, El Salvador, Grenada, Guatemala, Haiti, Honduras, Jamaica, Mexico, Nicaragua, Panama, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago), United States of America America (South): Argentina, Bolivia, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Guyana, Paraguay, -

Gender-Affirming Hormone Therapy
GENDER-AFFIRMING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health, Fenway Health March 2020 fenwayhealth.org GOALS AND OBJECTIVES 1. Review process of initiating hormone therapy through the informed consent model 2. Provide an overview of masculinizing and feminizing hormone therapy 3. Review realistic expectations and benefits of hormone therapy vs their associated risks 4. Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience and patient’s goals ▪ Document prior hormone use ▪ Assess appropriateness for gender affirming medical -
Guidelines for the Management of Heavy Menstrual Bleeding
i GUIDELINES FOR THE MANAGEMENT OF HEAVY MENSTRUAL BLEEDING Prepared by a Working Party on behalf of the National Health Committee ii MAY 1998 Women reporting with heavy menstrual bleeding 50% of women have menstrual blood loss Full menstrual history ● Examination ● Full blood count note1 Yes Prolonged irregular cycles No Refer Yes Abnormal exam specialist uterine size >12wks note 2 No mild or severe anaemic moderate treat < 80 g/l (80-115g/l) anaemia No Assess risk of endometrial hyperplasia low Offer medical therapy ● risk Unexplaine bodyweight 90kg heavy menstrual ● note5 note 6 age 45 years <2% bleeding ● other risk factors have 90% of women note 3 ● levonorgestrel endometrial >8% have hyperplasia intrauterine system ● tranexamic acid ● Assess endometrium nonsteroidal ● transvaginal ultrasound antiinflammatory agents ● (TVS) norethisterone long course or normal ● oc pill endometrium ● ● endometrial biopsy if danazol if one medical therapyfails endometrium 12mm others can be used note 7 or if TVS not available note 4 Treatment Hyperplastic endometrium success? or carcinoma No Yes Refer to specialist for hysteroscopic evaluation Continue Refer specialist me d i c a l for surgery therapy note8 note9 iii note 1 O In women <20 years old pelvic examination is unlikely to contribute to management of heavy bleeding (C) and the likelihood of pathology is small (C) O Increased likelihood (70%) of heavy menstrual blood loss >80mls/cycle if Hb <120g/l (A) O Consider pictorial blood loss assessment charts (appendix 6.5) for women with normal -

Gender-Affirming Hormone Therapy
GENDER-AFFIRMING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health Fenway Health November 2019 fenwayhealth.org GOALS AND OBJECTIVES 1.Review process of initiating hormone therapy through the informed consent model 2.Provide an overview of masculinizing and feminizing hormone therapy 3.Review realistic expectations and benefits of hormone therapy vs their associated risks 4.Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience ▪ Document prior hormone use ▪ Review patient goals ▪ Assess appropriateness for gender affirming medical -

Toiminta Unita on Ulla La Mungukurti |
TOIMINTAUNITA USON 20180071390A1ULLA LA MUNGUKURTI | ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2018/ 0071390 A1 PATEL et al. (43 ) Pub . Date : Mar . 15 , 2018 ( 54 ) COMPOSITIONS OF PHARMACEUTICAL A61K 9 / 06 (2006 .01 ) ACTIVES CONTAINING DIETHYLENE A61K 9 /00 (2006 .01 ) GLYCOL MONOETHYL ETHER OR OTHER A61K 31 /573 ( 2006 .01 ) ALKYL DERIVATIVES A61K 31/ 565 ( 2006 .01 ) A61K 31/ 4439 ( 2006 . 01 ) ( 71 ) Applicant : THEMIS MEDICARE LIMITED , A61K 31 / 167 ( 2006 . 01 ) Mumbai (IN ) A61K 31 / 57 (2006 . 01) (52 ) U . S . CI. (72 ) Inventors : Dinesh Shantilal PATEL , Mumbai CPC .. .. .. A61K 47 / 10 ( 2013 . 01 ) ; A61K 9 /4858 ( IN ) ; Sachin Dinesh PATEL , Mumbai ( 2013 .01 ) ; A61K 9 /08 ( 2013 .01 ) ; A61K 9 / 06 ( IN ) ; Shashikant Prabhudas ( 2013 .01 ) ; A61K 9 / 0014 ( 2013 .01 ) ; A61K KURANI, Mumbai ( IN ) ; Madhavlal 31/ 573 ( 2013 .01 ) ; A61K 31 /57 ( 2013 .01 ) ; Govindlal PATEL , Mumbai ( IN ) A61K 31/ 565 ( 2013 .01 ) ; A61K 31 /4439 (73 ) Assignee : THEMIS MEDICARE LIMITED , ( 2013 .01 ) ; A61K 31/ 167 ( 2013 .01 ) ; A61K Mumbai (IN ) 9 /0048 ( 2013 .01 ) ; A61K 9 /0019 (2013 .01 ) ( 57 ) ABSTRACT (21 ) Appl. No .: 15 / 801, 390 The present invention relates to pharmaceutical composi tions of various pharmaceutical actives, especially lyophilic ( 22 ) Filed : Nov . 2 , 2017 and hydrophilic actives containing Diethylene glycol mono ethyl ether or other alkyl derivatives thereof as a primary Related U . S . Application Data vehicle and /or to pharmaceutical compositions utilizing (62 ) Division of application No. 14 /242 , 973 , filed on Apr. Diethylene glycol monoethyl ether or other alkyl derivatives 2 , 2014 , now Pat. No. 9 , 827 ,315 . -

Combined Estrogen–Progestogen Menopausal Therapy
COMBINED ESTROGEN–PROGESTOGEN MENOPAUSAL THERAPY Combined estrogen–progestogen menopausal therapy was considered by previous IARC Working Groups in 1998 and 2005 (IARC, 1999, 2007). Since that time, new data have become available, these have been incorporated into the Monograph, and taken into consideration in the present evaluation. 1. Exposure Data 1.1.2 Progestogens (a) Chlormadinone acetate Combined estrogen–progestogen meno- Chem. Abstr. Serv. Reg. No.: 302-22-7 pausal therapy involves the co-administration Chem. Abstr. Name: 17-(Acetyloxy)-6-chlo- of an estrogen and a progestogen to peri- or ropregna-4,6-diene-3,20-dione menopausal women. The use of estrogens with IUPAC Systematic Name: 6-Chloro-17-hy- progestogens has been recommended to prevent droxypregna-4,6-diene-3,20-dione, acetate the estrogen-associated risk of endometrial Synonyms: 17α-Acetoxy-6-chloro-4,6- cancer. Evidence from the Women’s Health pregnadiene-3,20-dione; 6-chloro-Δ6-17- Initiative (WHI) of adverse effects from the use acetoxyprogesterone; 6-chloro-Δ6-[17α] of a continuous combined estrogen–progestogen acetoxyprogesterone has affected prescribing. Patterns of exposure Structural and molecular formulae, and relative are also changing rapidly as the use of hormonal molecular mass therapy declines, the indications are restricted, O CH and the duration of the therapy is reduced (IARC, 3 C 2007). CH3 CH3 O C 1.1 Identification of the agents CH3 H O 1.1.1 Estrogens HH For Estrogens, see the Monograph on O Estrogen-only Menopausal Therapy in this Cl volume. C23H29ClO4 Relative molecular mass: 404.9 249 IARC MONOGRAPHS – 100A (b) Cyproterone acetate Structural and molecular formulae, and relative Chem. -
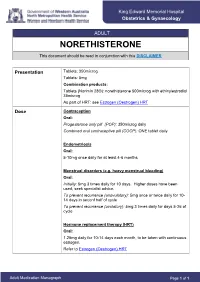
NORETHISTERONE This Document Should Be Read in Conjunction with This DISCLAIMER
King Edward Memorial Hospital Obstetrics & Gynaecology ADULT NORETHISTERONE This document should be read in conjunction with this DISCLAIMER Presentation Tablets: 350microg Tablets: 5mg Combination products: Tablets (Norimin 28®): norethisterone 500microg with ethinylestradiol 35microg As part of HRT: see Estrogen (Oestrogen) HRT Dose Contraception Oral: Progesterone only pill (POP): 350microg daily Combined oral contraceptive pill (COCP): ONE tablet daily Endometriosis Oral: 5-10mg once daily for at least 4-6 months Menstrual disorders (e.g. heavy menstrual bleeding) Oral: Initially: 5mg 3 times daily for 10 days. Higher doses have been used; seek specialist advice. To prevent recurrence (anovulatory): 5mg once or twice daily for 10- 14 days in seconf half of cycle To prevent recurrence (ovulatory): 5mg 3 times daily for days 5-26 of cycle Hormone replacement therapy (HRT) Oral: 1.25mg daily for 10-14 days each month, to be taken with continuous estrogen. Refer to Estrogen (Oestrogen) HRT Adult Medication Monograph Page 1 of 1 Norethisterone – Adult Administration Oral To be taken at the same time each day (or within 3 hours of the usual dose time). For Contraception: Start 4 weeks after the birth of baby (increased risk of abnormal vaginal bleeding if started earlier) Pregnancy 1st Trimester: Contraindicated 2nd Trimester: Contraindicated 3rd Trimester: Contraindicated Breastfeeding Considered safe to use. Progestogens are the preferred hormonal contraceptives as they do not inhibit lactation. Clinical Guidelines Estrogen (Oestrogen) HRT and Policies Progesterone Only Pill Contraception: Post Partum Gynaecology (Non-Oncological) Australian Medicines Handbook. Norethisterone. In: Australian References Medicines Handbook [Internet]. Adelaide (South Australia): Australian Medicines Handbook; 2017 [cited 2017 Apr 12]. -

Nur-Isterate Injection
SELECT THE REQUIRED INFORMATION PROFESSIONAL INFORMATION PATIENT INFORMATION LEAFLET SCHEDULING STATUS: S4 PROPRIETARY NAME AND DOSAGE FORM: NUR-ISTERATE Oily solution for intramuscular injection COMPOSITION: 1 ml contains norethisterone enantate (17-ethinyl-17-heptanoyloxy-4-estrene-3-one) 200 mg. Other ingredients are: benzyl benzoate, castor oil for injection. PHARMACOLOGICAL CLASSIFICATION: A. 21.8.2 Progesterones without estrogens. PHARMACOLOGICAL ACTION: Pharmacodynamic properties: Protection against conception is based primarily upon an alteration of the cervical mucous. This alteration is present for the whole of the duration of action and prevents the ascent of the sperm into the uterine cavity. Radioimmunological studies have shown that, during the first 5 to 7 weeks after injection, ovulation is suppressed as a result of the high plasma level of norethisterone. In addition, NUR- ISTERATE causes morphological changes in the endometrium which have the effect of rendering nidation of a fertilised egg difficult. Pharmacokinetic properties: Norethisterone enantate was completely absorbed after intramuscular injection. The ester was eventually completely hydrolysed to its pharmacologically active compound norethisterone once it was released from the depot. Maximum levels of norethisterone were measured at about 3 to 10 days after IM administration. They amounted on average to 13.4 5.4 ng/ml and 12.2 2.7 ng/ml about 7 days (median) after IM administration of 200 mg norethisterone enantate in 2 ml and 1 ml oily solution, respectively. Plasma levels of norethisterone declined in two disposition phases with half-lives of 4 to 5 days and 15 to 20 days, respectively, which were due to a biphasic release of norethisterone enantate from the depot. -

FDA Briefing Document NDA 206089 Testosterone Undecanoate
FDA Briefing Document NDA 206089 Testosterone Undecanoate (proposed trade name Jatenzo) For replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone. Bone, Reproductive, and Urologic Drugs Advisory Committee (BRUDAC) Meeting January 9, 2018 Division of Bone, Reproductive, and Urologic Products Office of New Drugs Division of Clinical Pharmacology 3 Office of Clinical Pharmacology Center for Drug Evaluation and Research 1 DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought a new drug application (NDA 206089) for testosterone undecanoate oral capsules (proposed trade name, JATENZO), intended for replacement therapy in adult males for conditions associated with a deficiency or absence of endogenous testosterone sponsored by Clarus Therapeutics, Inc, to this Advisory Committee in order to gain the Committee’s insights and opinions. The background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered and all reviews have been finalized. The final determination may be affected by issues not discussed at the advisory committee meeting. -

A Rare Case of Cerebral Venous Sinus Thrombosis (CVST) Induced by Norethisterone Enanthate: Report from a Medical University Hospital in Bangladesh
Case Report Annals of Clinical Case Reports Published: 25 Jan, 2019 A Rare Case of Cerebral Venous Sinus Thrombosis (CVST) Induced by Norethisterone Enanthate: Report from a Medical University Hospital in Bangladesh Raknuzzaman1, Anis Ahmed1*, Masud Rana1, Kazi Jannat Ara1 and Dewan Md Emdadul Hoque1 1Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Bangladesh 2Department of Epidemiology and Preventive Medicine, International Centre for Diarrhoeal Disease Research, Bangladesh Abstract Cerebral Venous Sinus Thrombosis (CVST) is a rare condition and the association between norethisterone enanthate and CVST in the literature has very seldom been reported. In this case report, a 22-year-old unmarried woman of Bangladesh presented with acute onset of headache and vomiting with history of oral intake of 5 mg norethisterone thrice daily during past 2 years for menstrual disorder. She had no history of seizure, visual disturbances, and neck stiffness, imbalance of gait and weakness of any limbs, any sensory complaints or any episode of unconsciousness during the course of illness. Bilateral papilloedema was present with more marked on left eye and serum homocysteine level was high. A brain CT scan, MRI and Magnetic Resonance Venogram (MRV) revealed thrombosed anterosuperior segment of superior sagittal sinus. She was diagnosed to have CVST due to norethisterone and was treated with low molecular weight heparin, followed by Rivaroxaban, Vitamin B12, Vitamin B6 and Folic acid. She made a complete recovery after one month of intake of rivaroxaban and withdrawn of norethisterone. Keywords: Cerebral venous sinus thrombosis; Norethisterone enanthate; Hyperhomocysteinemia; OPEN ACCESS Rivaroxaban *Correspondence: Introduction Anis Ahmed, Department of Neurology, Cerebral Venous Sinuses Thrombosis (CVST) is rare type of stroke with the annual incidence Bangabandhu Sheikh Mujib Medical ranging from 0.22 to 1.57 per 100,000 populations, affecting young individuals and mostly women University, Bangladesh, Tel: [1-3]. -

Combined Estrogen–Progestogen Menopausal Therapy
PHARMACEUTICALS volume 100 A A review of humAn cArcinogens This publication represents the views and expert opinions of an IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, which met in Lyon, 14-21 October 2008 LYON, FRANCE - 2012 iArc monogrAphs on the evAluAtion of cArcinogenic risks to humAns COMBINED ESTROGEN–PROGESTOGEN MENOPAUSAL THERAPY Combined estrogen–progestogen menopausal therapy was considered by previous IARC Working Groups in 1998 and 2005 (IARC, 1999, 2007). Since that time, new data have become available, these have been incorporated into the Monograph, and taken into consideration in the present evaluation. 1. Exposure Data 1.1.2 Progestogens (a) Chlormadinone acetate Combined estrogen–progestogen meno- Chem. Abstr. Serv. Reg. No.: 302-22-7 pausal therapy involves the co-administration Chem. Abstr. Name: 17-(Acetyloxy)-6-chlo- of an estrogen and a progestogen to peri- or ropregna-4,6-diene-3,20-dione menopausal women. The use of estrogens with IUPAC Systematic Name: 6-Chloro-17-hy- progestogens has been recommended to prevent droxypregna-4,6-diene-3,20-dione, acetate the estrogen-associated risk of endometrial Synonyms: 17α-Acetoxy-6-chloro-4,6- cancer. Evidence from the Women’s Health pregnadiene-3,20-dione; 6-chloro-Δ6-17- Initiative (WHI) of adverse effects from the use acetoxyprogesterone; 6-chloro-Δ6-[17α] of a continuous combined estrogen–progestogen acetoxyprogesterone has affected prescribing. Patterns of exposure Structural and molecular formulae, and relative are also changing rapidly as the use of hormonal molecular mass therapy declines, the indications are restricted, O CH and the duration of the therapy is reduced (IARC, 3 C 2007). -

Steroids and Other Appearance and Performance Enhancing Drugs (Apeds) Research Report
Research Report Revised Febrero 2018 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Table of Contents Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Introduction What are the different types of APEDs? What is the history of anabolic steroid use? Who uses anabolic steroids? Why are anabolic steroids misused? How are anabolic steroids used? What are the side effects of anabolic steroid misuse? How does anabolic steroid misuse affect behavior? What are the risks of anabolic steroid use in teens? How do anabolic steroids work in the brain? Are anabolic steroids addictive? How are anabolic steroids tested in athletes? What can be done to prevent steroid misuse? What treatments are effective for anabolic steroid misuse? Where can I get further information about steroids? References Page 1 Steroids and Other Appearance and Performance Enhancing Drugs (APEDs) Research Report Esta publicación está disponible para su uso y puede ser reproducida, en su totalidad, sin pedir autorización al NIDA. Se agradece la citación de la fuente, de la siguiente manera: Fuente: Instituto Nacional sobre el Abuso de Drogas; Institutos Nacionales de la Salud; Departamento de Salud y Servicios Humanos de los Estados Unidos. Introduction Appearance and performance enhancing drugs (APEDs) are most often used by males to improve appearance by building muscle mass or to enhance athletic performance. Although they may directly and indirectly have effects on a user’s mood, they do not produce a euphoric high, which makes APEDs distinct from other drugs such as cocaine, heroin, and marijuana. However, users may develop a substance use disorder, defined as continued use despite adverse consequences.