Summary of Data Reported and Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Compositions Comprising Drospirenone Molecularly
(19) & (11) EP 1 748 756 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/00 (2006.01) A61K 9/107 (2006.01) 29.04.2009 Bulletin 2009/18 A61K 9/48 (2006.01) A61K 9/16 (2006.01) A61K 9/20 (2006.01) A61K 9/14 (2006.01) (2006.01) (2006.01) (21) Application number: 05708751.2 A61K 9/70 A61K 31/565 (22) Date of filing: 10.03.2005 (86) International application number: PCT/IB2005/000665 (87) International publication number: WO 2005/087194 (22.09.2005 Gazette 2005/38) (54) COMPOSITIONS COMPRISING DROSPIRENONE MOLECULARLY DISPERSED ZUSAMMENSETZUNGEN AUS DROSPIRENON IN MOLEKULARER DISPERSION DES COMPOSITIONS CONTENANT DROSPIRENONE A DISPERSION MOLECULAIRE (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • FUNKE, Adrian HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR D-14055 Berlin (DE) Designated Extension States: • WAGNER, Torsten AL BA HR MK YU 13127 Berlin (DE) (30) Priority: 10.03.2004 EP 04075713 (74) Representative: Wagner, Kim 10.03.2004 US 551355 P Plougmann & Vingtoft a/s Sundkrogsgade 9 (43) Date of publication of application: P.O. Box 831 07.02.2007 Bulletin 2007/06 2100 Copenhagen Ø (DK) (60) Divisional application: (56) References cited: 08011577.7 / 1 980 242 EP-A- 1 260 225 EP-A- 1 380 301 WO-A-01/52857 WO-A-20/04022065 (73) Proprietor: Bayer Schering Pharma WO-A-20/04041289 US-A- 5 569 652 Aktiengesellschaft US-A- 5 656 622 US-A- 5 789 442 13353 Berlin (DE) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Drospirenone-Containing Birth Control Pills (Yaz, Yasmin, Ocella, Gianvi and Their Generics)
Drospirenone-Containing Birth Control Pills (Yaz, Yasmin, Ocella, Gianvi and their generics) Drospirenone is a progestin component of some birth control pills that does some blocking of testosterone (the "male hormone" that women have, too, and the hormone that can be a part of making acne worse). This is why drospirenone-containing birth control pills are especially good at helping acne (and why they can theoretically help hirsutism and female-pattern scalp hair loss as well). Drospirenone is also a mild diuretic and is why these birth control pills do not cause the water weight gain that some birth control pills can. Any birth control pill can theoretically help acne just by evening out hormonal fluctuations, but for many birth control pills, the effects on acne is very minimal. Which birth control pills are most likely to help acne? Some birth control pills are more like testosterone and some are less like testosterone. The ones that are less like testosterone can theoretically help acne more. The drospirenone-containing birth control pills go one step further by blocking testosterone, and may show the most benefit on clearing acne. Drospirenone is a progestin that is derived from 17-alpha-spironolactone and is chemically related to the diuretic spironolactone. Spironolactone is a diuretic (used for high blood pressure) that is sometimes used off-label for the treatment of acne, hirsutism or female-pattern hair loss. Often people say that a drospirenone-containing birth control pill may be equivalent to 25mg of spironolactone. Risks : Any estrogen-containing birth control pill increases the risk of a high blood pressure, stroke, or other life-threatening blood clot, and one study showed possibly a slightly higher risk with a drospirenone-containing birth control pill. -

Index Vol. 12-15
353 INDEX VOL. 12-15 Die Stichworte des Sachregisters sind in der jeweiligen Sprache der einzelnen Beitrage aufgefiihrt. Les termes repris dans la Table des matieres sont donnes selon la langue dans laquelle l'ouvrage est ecrit. The references of the Subject Index are given in the language of the respective contribution. 14 AAG (Alpha-acid glycoprotein) 120 14 Adenosine 108 12 Abortion 151 12 Adenosine-phosphate 311 13 Abscisin 12, 46, 66 13 Adenosine-5'-phosphosulfate 148 14 Absorbierbarkeit 317 13 Adenosine triphosphate 358 14 Absorption 309, 350 15 S-Adenosylmethionine 261 13 Absorption of drugs 139 13 Adipaenin (Spasmolytin) 318 14 - 15 12 Adrenal atrophy 96 14 Absorptionsgeschwindigkeit 300, 306 14 - 163, 164 14 Absorptionsquote 324 13 Adrenal gland 362 14 ACAI (Anticorticocatabolic activity in 12 Adrenalin(e) 319 dex) 145 14 - 209, 210 12 Acalo 197 15 - 161 13 Aceclidine (3-Acetoxyquinuclidine) 307, 13 {i-Adrenergic blockers 119 308, 310, 311, 330, 332 13 Adrenergic-blocking activity 56 13 Acedapsone 193,195,197 14 O(-Adrenergic blocking drugs 36, 37, 43 13 Aceperone (Acetabutone) 121 14 {i-Adrenergic blocking drugs 38 12 Acepromazin (Plegizil) 200 14 Adrenergic drugs 90 15 Acetanilid 156 12 Adrenocorticosteroids 14, 30 15 Acetazolamide 219 12 Adrenocorticotropic hormone (ACTH) 13 Acetoacetyl-coenzyme A 258 16,30,155 12 Acetohexamide 16 14 - 149,153,163,165,167,171 15 1-Acetoxy-8-aminooctahydroindolizin 15 Adrenocorticotropin (ACTH) 216 (Slaframin) 168 14 Adrenosterone 153 13 4-Acetoxy-1-azabicyclo(3, 2, 2)-nonane 12 Adreson 252 -

Download PDF File
Ginekologia Polska 2019, vol. 90, no. 9, 520–526 Copyright © 2019 Via Medica ORIGINAL PAPER / GYNECologY ISSN 0017–0011 DOI: 10.5603/GP.2019.0091 Anti-androgenic therapy in young patients and its impact on intensity of hirsutism, acne, menstrual pain intensity and sexuality — a preliminary study Anna Fuchs, Aleksandra Matonog, Paulina Sieradzka, Joanna Pilarska, Aleksandra Hauzer, Iwona Czech, Agnieszka Drosdzol-Cop Department of Pregnancy Pathology, Department of Woman’s Health, School of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland ABSTRACT Objectives: Using anti-androgenic contraception is one of the methods of birth control. It also has a significant, non-con- traceptive impact on women’s body. These drugs can be used in various endocrinological disorders, because of their ability to reduce the level of male hormones. The aim of our study is to establish a correlation between taking different types of anti-androgenic drugs and intensity of hirsutism, acne, menstrual pain intensity and sexuality . Material and methods: 570 women in childbearing age that had been using oral contraception for at least three months took part in our research. We examined women and asked them about quality of life, health, direct causes and effects of that treatment, intensity of acne and menstrual pain before and after. Our research group has been divided according to the type of gestagen contained in the contraceptive pill: dienogest, cyproterone, chlormadynone and drospirenone. Ad- ditionally, the control group consisted of women taking oral contraceptives without antiandrogenic component. Results: The mean age of the studied group was 23 years ± 3.23. 225 of 570 women complained of hirsutism. -

Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis In
JMIR RESEARCH PROTOCOLS Amiri et al Review Comparing the Effects of Combined Oral Contraceptives Containing Progestins With Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis in Patients With Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis Mina Amiri1,2, PhD, Postdoc; Fahimeh Ramezani Tehrani2, MD; Fatemeh Nahidi3, PhD; Ali Kabir4, MD, MPH, PhD; Fereidoun Azizi5, MD 1Students Research Committee, School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 2Reproductive Endocrinology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 3School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 4Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Islamic Republic Of Iran 5Endocrine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran Corresponding Author: Fahimeh Ramezani Tehrani, MD Reproductive Endocrinology Research Center Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences 24 Parvaneh Yaman Street, Velenjak, PO Box 19395-4763 Tehran, 1985717413 Islamic Republic Of Iran Phone: 98 21 22432500 Email: [email protected] Abstract Background: Different products of combined oral contraceptives (COCs) can improve clinical and biochemical findings in patients with polycystic ovary syndrome (PCOS) through suppression of the hypothalamic-pituitary-gonadal (HPG) axis. Objective: This systematic review and meta-analysis aimed to compare the effects of COCs containing progestins with low androgenic and antiandrogenic activities on the HPG axis in patients with PCOS. -

Pp375-430-Annex 1.Qxd
ANNEX 1 CHEMICAL AND PHYSICAL DATA ON COMPOUNDS USED IN COMBINED ESTROGEN–PROGESTOGEN CONTRACEPTIVES AND HORMONAL MENOPAUSAL THERAPY Annex 1 describes the chemical and physical data, technical products, trends in produc- tion by region and uses of estrogens and progestogens in combined estrogen–progestogen contraceptives and hormonal menopausal therapy. Estrogens and progestogens are listed separately in alphabetical order. Trade names for these compounds alone and in combination are given in Annexes 2–4. Sales are listed according to the regions designated by WHO. These are: Africa: Algeria, Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Cape Verde, Central African Republic, Chad, Comoros, Congo, Côte d'Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Eritrea, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Sao Tome and Principe, Senegal, Seychelles, Sierra Leone, South Africa, Swaziland, Togo, Uganda, United Republic of Tanzania, Zambia and Zimbabwe America (North): Canada, Central America (Antigua and Barbuda, Bahamas, Barbados, Belize, Costa Rica, Cuba, Dominica, El Salvador, Grenada, Guatemala, Haiti, Honduras, Jamaica, Mexico, Nicaragua, Panama, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago), United States of America America (South): Argentina, Bolivia, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Guyana, Paraguay, -
Guidelines for the Management of Heavy Menstrual Bleeding
i GUIDELINES FOR THE MANAGEMENT OF HEAVY MENSTRUAL BLEEDING Prepared by a Working Party on behalf of the National Health Committee ii MAY 1998 Women reporting with heavy menstrual bleeding 50% of women have menstrual blood loss Full menstrual history ● Examination ● Full blood count note1 Yes Prolonged irregular cycles No Refer Yes Abnormal exam specialist uterine size >12wks note 2 No mild or severe anaemic moderate treat < 80 g/l (80-115g/l) anaemia No Assess risk of endometrial hyperplasia low Offer medical therapy ● risk Unexplaine bodyweight 90kg heavy menstrual ● note5 note 6 age 45 years <2% bleeding ● other risk factors have 90% of women note 3 ● levonorgestrel endometrial >8% have hyperplasia intrauterine system ● tranexamic acid ● Assess endometrium nonsteroidal ● transvaginal ultrasound antiinflammatory agents ● (TVS) norethisterone long course or normal ● oc pill endometrium ● ● endometrial biopsy if danazol if one medical therapyfails endometrium 12mm others can be used note 7 or if TVS not available note 4 Treatment Hyperplastic endometrium success? or carcinoma No Yes Refer to specialist for hysteroscopic evaluation Continue Refer specialist me d i c a l for surgery therapy note8 note9 iii note 1 O In women <20 years old pelvic examination is unlikely to contribute to management of heavy bleeding (C) and the likelihood of pathology is small (C) O Increased likelihood (70%) of heavy menstrual blood loss >80mls/cycle if Hb <120g/l (A) O Consider pictorial blood loss assessment charts (appendix 6.5) for women with normal -

Drugs Contraindicated in Pregnancy
DRUGS CONTRAINDICATED IN PREGNANCY (Part 1 of 2) This chart represents information on select drugs that are contraindicated (Pregnancy category X) for women who are pregnant. This is not an inclusive list of products that carry that pregnancy category. Those drugs that are contraindicated at a certain phase of the pregnancy are listed next to the product name. For more information on specific drug monographs, see product entries or consult the manufacturer. ALLERGIC DISORDERS Tazorac (tazarotene) METABOLIC DISORDERS Tilia Fe (norethindrone acetate/ethinyl Vistaril (hydroxyzine) Early pregnancy estradiol) Zavesca (miglustat) CARDIOVASCULAR SYSTEM Tri-Legest Fe (norethindrone acetate/ MUSCULOSKELETAL DISORDERS ethinyl estradiol) Advicor (niacin ext-rel/lovastatin) Tri-previfem (norgestimate/ethinyl Advil (ibuprofen) 3rd trimester Aggrenox (dipyridamole/aspirin) 3rd estradiol) Aleve (naproxen sodium) 3rd trimester trimester Tri-sprintec (norgestimate/ethinyl estradiol) Ansaid (flurbiprofen) Late pregnancy Altoprev (lovastatin) Yaz (drospirenone/ethinyl estradiol) Arava (leflunomide) Bayer (aspirin) 3rd trimester Arthrotec (diclofenac sodium/ Caduet (amlodipine/atorvastatin) ENDOCRINE SYSTEM misoprostol) Coumadin (warfarin sodium) 3rd trimester Androderm (testosterone) Bayer (aspirin) Crestor (rosuvastatin) Androgel (testosterone) BC Arthritis Strength (aspirin/ Ecotrin (aspirin) 3rd trimester 3rd trimester Android (methyltestosterone) caffeine/salicylamide) Lescol (fluvastatin) 3rd Axiron (testosterone) Carisoprodol/aspirin/codeine Lescol -
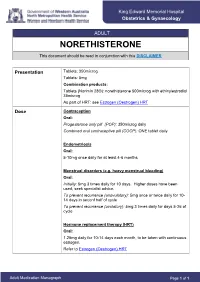
NORETHISTERONE This Document Should Be Read in Conjunction with This DISCLAIMER
King Edward Memorial Hospital Obstetrics & Gynaecology ADULT NORETHISTERONE This document should be read in conjunction with this DISCLAIMER Presentation Tablets: 350microg Tablets: 5mg Combination products: Tablets (Norimin 28®): norethisterone 500microg with ethinylestradiol 35microg As part of HRT: see Estrogen (Oestrogen) HRT Dose Contraception Oral: Progesterone only pill (POP): 350microg daily Combined oral contraceptive pill (COCP): ONE tablet daily Endometriosis Oral: 5-10mg once daily for at least 4-6 months Menstrual disorders (e.g. heavy menstrual bleeding) Oral: Initially: 5mg 3 times daily for 10 days. Higher doses have been used; seek specialist advice. To prevent recurrence (anovulatory): 5mg once or twice daily for 10- 14 days in seconf half of cycle To prevent recurrence (ovulatory): 5mg 3 times daily for days 5-26 of cycle Hormone replacement therapy (HRT) Oral: 1.25mg daily for 10-14 days each month, to be taken with continuous estrogen. Refer to Estrogen (Oestrogen) HRT Adult Medication Monograph Page 1 of 1 Norethisterone – Adult Administration Oral To be taken at the same time each day (or within 3 hours of the usual dose time). For Contraception: Start 4 weeks after the birth of baby (increased risk of abnormal vaginal bleeding if started earlier) Pregnancy 1st Trimester: Contraindicated 2nd Trimester: Contraindicated 3rd Trimester: Contraindicated Breastfeeding Considered safe to use. Progestogens are the preferred hormonal contraceptives as they do not inhibit lactation. Clinical Guidelines Estrogen (Oestrogen) HRT and Policies Progesterone Only Pill Contraception: Post Partum Gynaecology (Non-Oncological) Australian Medicines Handbook. Norethisterone. In: Australian References Medicines Handbook [Internet]. Adelaide (South Australia): Australian Medicines Handbook; 2017 [cited 2017 Apr 12]. -

Nur-Isterate Injection
SELECT THE REQUIRED INFORMATION PROFESSIONAL INFORMATION PATIENT INFORMATION LEAFLET SCHEDULING STATUS: S4 PROPRIETARY NAME AND DOSAGE FORM: NUR-ISTERATE Oily solution for intramuscular injection COMPOSITION: 1 ml contains norethisterone enantate (17-ethinyl-17-heptanoyloxy-4-estrene-3-one) 200 mg. Other ingredients are: benzyl benzoate, castor oil for injection. PHARMACOLOGICAL CLASSIFICATION: A. 21.8.2 Progesterones without estrogens. PHARMACOLOGICAL ACTION: Pharmacodynamic properties: Protection against conception is based primarily upon an alteration of the cervical mucous. This alteration is present for the whole of the duration of action and prevents the ascent of the sperm into the uterine cavity. Radioimmunological studies have shown that, during the first 5 to 7 weeks after injection, ovulation is suppressed as a result of the high plasma level of norethisterone. In addition, NUR- ISTERATE causes morphological changes in the endometrium which have the effect of rendering nidation of a fertilised egg difficult. Pharmacokinetic properties: Norethisterone enantate was completely absorbed after intramuscular injection. The ester was eventually completely hydrolysed to its pharmacologically active compound norethisterone once it was released from the depot. Maximum levels of norethisterone were measured at about 3 to 10 days after IM administration. They amounted on average to 13.4 5.4 ng/ml and 12.2 2.7 ng/ml about 7 days (median) after IM administration of 200 mg norethisterone enantate in 2 ml and 1 ml oily solution, respectively. Plasma levels of norethisterone declined in two disposition phases with half-lives of 4 to 5 days and 15 to 20 days, respectively, which were due to a biphasic release of norethisterone enantate from the depot. -

Use of Postmenopausal Hormone Therapy and Risk of Alzheimer’S BMJ: First Published As 10.1136/Bmj.L665 on 6 March 2019
RESEARCH Use of postmenopausal hormone therapy and risk of Alzheimer’s BMJ: first published as 10.1136/bmj.l665 on 6 March 2019. Downloaded from disease in Finland: nationwide case-control study Hanna Savolainen-Peltonen,1,2 Päivi Rahkola-Soisalo,1 Fabian Hoti,3 Pia Vattulainen,3 Mika Gissler,4,5,6 Olavi Ylikorkala,1 Tomi S Mikkola1,2 1University of Helsinki and ABSTRACT ratio 1.09, 95% confidence interval 1.05 to 1.14) and Helsinki University Hospital, OBJECTIVES those of oestrogen-progestogen (1.17, 1.13 to 1.21). Obstetrics and Gynecology, To compare the use of hormone therapy between The risk increases in users of oestrogen-progestogen Haartmaninkatu 2, PO Box 140, FIN-00029 HUS, 00029 Finnish postmenopausal women with and without a therapy were not related to different progestogens Helsinki, Finland diagnosis for Alzheimer’s disease. (noreth isterone acetate, medroxyprogesterone 2 Folkhälsan Research Center, DESIGN acetate, or other progestogens); but in women Biomedicum, Helsinki, Finland younger than 60 at hormone therapy initiation, 3 Nationwide case-control study. EPID Research Oy, Espoo, these risk increases were associated with hormone Finland SETTING therapy exposure over 10 years. Furthermore, the 4National Institute for Health Finnish national population and drug register, age at initiation of systemic hormone therapy was and Welfare, Helsinki, Finland between 1999 and 2013. 5Karolinska Institute, not a decisive determinant for the increase in risk Department of Neurobiology, PARTICIPANTS of Alzheimer’s disease. The exclusive use of vaginal Care Sciences and Society, All postmenopausal women (n=84 739) in Finland estradiol did not affect the risk of the disease (0.99, Division of Family Medicine, who, between 1999 and 2013, received a diagnosis of 0.96 to 1.01). -

Guidance on Bioequivalence Studies for Reproductive Health Medicines
Medicines Guidance Document 23 October 2019 Guidance on Bioequivalence Studies for Reproductive Health Medicines CONTENTS 1. Introduction........................................................................................................................................................... 2 2. Which products require a bioequivalence study? ................................................................................................ 3 3. Design and conduct of bioequivalence studies .................................................................................................... 4 3.1 Basic principles in the demonstration of bioequivalence ............................................................................... 4 3.2 Good clinical practice ..................................................................................................................................... 4 3.3 Contract research organizations .................................................................................................................... 5 3.4 Study design .................................................................................................................................................. 5 3.5 Comparator product ....................................................................................................................................... 6 3.6 Generic product .............................................................................................................................................. 6 3.7 Study subjects