Capillarys Hemoglobin(E) Using the Capillarys 2 Flex-Piercing Instrument
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoglobin Variants: Biochemical Properties and Clinical Correlates
Downloaded from http://perspectivesinmedicine.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Hemoglobin Variants: Biochemical Properties and Clinical Correlates Christopher S. Thom1,2, Claire F. Dickson3, David A. Gell3, and Mitchell J. Weiss2 1Cell and Molecular Biology Graduate Group, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 2Hematology Department, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania 19104 3Menzies Research Institute, University of Tasmania, Hobart, Australia Correspondence: [email protected] Diseases affecting hemoglobin synthesis and function are extremely common worldwide. More than 1000 naturally occurring human hemoglobin variants with single amino acid substitutions throughout the molecule have been discovered, mainly through their clinical and/or laboratory manifestations. These variants alter hemoglobin structure and biochem- ical properties with physiological effects ranging from insignificant to severe. Studies of these mutations in patients and in the laboratory have produced a wealth of information on he- moglobin biochemistry and biology with significant implications for hematology practice. More generally, landmark studies of hemoglobin performed over the past 60 years have established important paradigms for the disciplines of structural biology, genetics, biochem- istry, and medicine. Here we review the major classes of hemoglobin variants, emphasizing general concepts and illustrative examples. lobin gene mutations affecting hemoglobin stitutions, antitermination mutations, and al- G(Hb), the major blood oxygen (O2) carrier, tered posttranslational processing (Table 1). are common, affecting an estimated 7% of the Naturally occurring Hb mutations cause a world’s population (Weatherall and Clegg 2001; range of biochemical abnormalities, some of Kohne 2011). These mutations are broadly sub- which produce clinically significant symptoms. -

Hemoglobinopathies: Clinical & Hematologic Features And
Hemoglobinopathies: Clinical & Hematologic Features and Molecular Basis Abdullah Kutlar, MD Professor of Medicine Director, Sickle Cell Center Georgia Health Sciences University Types of Normal Human Hemoglobins ADULT FETAL Hb A ( 2 2) 96-98% 15-20% Hb A2 ( 2 2) 2.5-3.5% undetectable Hb F ( 2 2) < 1.0% 80-85% Embryonic Hbs: Hb Gower-1 ( 2 2) Hb Gower-2 ( 2 2) Hb Portland-1( 2 2) Hemoglobinopathies . Qualitative – Hb Variants (missense mutations) Hb S, C, E, others . Quantitative – Thalassemias Decrease or absence of production of one or more globin chains Functional Properties of Hemoglobin Variants . Increased O2 affinity . Decreased O2 affinity . Unstable variants . Methemoglobinemia Clinical Outcomes of Substitutions at Particular Sites on the Hb Molecule . On the surface: Sickle Hb . Near the Heme Pocket: Hemolytic anemia (Heinz bodies) Methemoglobinemia (cyanosis) . Interchain contacts: 1 1 contact: unstable Hbs 1 2 contact: High O2 affinity: erythrocytosis Low O2 affinity: anemia Clinically Significant Hb Variants . Altered physical/chemical properties: Hb S (deoxyhemoglobin S polymerization): sickle syndromes Hb C (crystallization): hemolytic anemia; microcytosis . Unstable Hb Variants: Congenital Heinz body hemolytic anemia (N=141) . Variants with altered Oxygen affinity High affinity variants: erythrocytosis (N=93) Low affinity variants: anemia, cyanosis (N=65) . M-Hemoglobins Methemoglobinemia, cyanosis (N=9) . Variants causing a thalassemic phenotype (N=51) -thalassemia Hb Lepore ( ) fusion Aberrant RNA processing (Hb E, Hb Knossos, Hb Malay) Hyperunstable globins (Hb Geneva, Hb Westdale, etc.) -thalassemia Chain termination mutants (Hb Constant Spring) Hyperunstable variants (Hb Quong Sze) Modified and updated from Bunn & Forget: Hemoglobin: Molecular, Genetic, and Clinical Aspects. WB Saunders, 1986. -

The Developmental Genetics of Hemoglobin Synthesis in Chironomus Darrel Starr English Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1968 The developmental genetics of hemoglobin synthesis in Chironomus Darrel Starr English Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Genetics Commons Recommended Citation English, Darrel Starr, "The developmental genetics of hemoglobin synthesis in Chironomus " (1968). Retrospective Theses and Dissertations. 3660. https://lib.dr.iastate.edu/rtd/3660 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. This dissertation has been microfilmed exactly as received 6 8-14,785 ENGLISH, Barrel Starr, 1936- THE DEVELOPMENTAL GENETICS OF HEMOGLOBIN SYNTHESIS IN CHIRONOMUS. Iowa State University, Ph.D., 1968 Biology- Genetics University Microfilms, Inc., Ann Arbor, Michigan THE DEVELOPMENTAL GENETICS OF HEMOGLOBIN SYNTHESIS IN CHIRONOMUS by Darrel Starr English A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of The Requirements for the Degree of DOCTOR OF PHILOSOPHY Major Subject: Genetics Approved: Signature was redacted for privacy. In Charge of MajdA Work Signature was redacted for privacy. Head ^ Major Department Signature was redacted for privacy. -
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
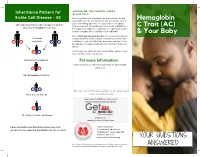
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Phd Thesis Tjaard Pijning
University of Groningen Divergent or just different Rozeboom, Henriette IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2014 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Rozeboom, H. (2014). Divergent or just different: Structural studies on six different enzymes. [S.n.]. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 29-09-2021 Divergent or just different Structural studies on six different enzymes Henriëtte Rozeboom Printed by Ipskamp Drukkers, Enschede The research presented in this thesis was carried out in the Protein Crystallography group at the Groningen Biomolecular Sciences and Biotechnology Institute. -

Impact of Heterozygous Hemoglobin E on Six Commercial Methods for Hemoglobin A1c Measurement
Impact of heterozygous hemoglobin E on six commercial methods for hemoglobin A1c measurement Sharon Yong1, Hong Liu1, Cindy Lye Teng Lum2, Qian Liu2, Sin Ye Sim3, Felicia Fu Mun Chay3, Wan Ling Cheng4, Siew Fong Neo4, Suru Chew4, Lizhen Ong4, Tze Ping Loh4, Qinde Liu1, Tang Lin Teo1 and Sunil Kumar Sethi4 1 Chemical Metrology Division, Health Sciences Authority, Singapore, Singapore 2 Department of Pathology, Sengkang General Hospital, Singapore, Singapore 3 Department of Laboratory Medicine, Alexandra Hospital, Singapore, Singapore 4 Department of Laboratory Medicine, National University Hospital, Singapore, Singapore ABSTRACT Background: This study examined the impact of heterozygous HbE on HbA1c measurements by six commonly used commercial methods. The results were compared with those from a modified isotope-dilution mass spectrometry (IDMS) reference laboratory method on a liquid chromatograph coupled with tandem mass spectrometer (LC-MS/MS). Methods: Twenty-three leftover samples of patients with heterozygous HbE (HbA1c range: 5.4–11.6%), and nineteen samples with normal hemoglobin (HbA1c range: 5.0–13.7%) were included. The selected commercial methods included the Tina-quant HbA1c Gen. 3 (Roche Diagnostics, Basel, Switzerland), Cobas B 101 (Roche Diagnostics, Basel, Switzerland), D100 (Bio-Rad Laboratories, Hercules, CA, USA), Variant II Turbo HbA1c 2.0 (Bio-Rad Laboratories, Hercules, CA, USA), DCA Vantage (Siemens Healthcare, Erlangen, Germany) and HbA1c Advanced (Beckman Coulter Inc., Brea, CA, USA). Results: With the exception of Cobas B 101 and the Variant II Turbo 2.0, the 95% confidence intervals of the Passing–Bablok regression lines between the results Submitted 25 September 2020 from the six commercial methods and the IDMS method overlapped. -

A Distant Gene Deletion Affects Beta-Globin Gene Function in an Atypical Gamma Delta Beta-Thalassemia
A distant gene deletion affects beta-globin gene function in an atypical gamma delta beta-thalassemia. P Curtin, … , A D Stephens, H Lehmann J Clin Invest. 1985;76(4):1554-1558. https://doi.org/10.1172/JCI112136. Research Article We describe an English family with an atypical gamma delta beta-thalassemia syndrome. Heterozygosity results in a beta-thalassemia phenotype with normal hemoglobin A2. However, unlike previously described cases, no history of neonatal hemolytic anemia requiring blood transfusion was obtained. Gene mapping showed a deletion that extended from the third exon of the G gamma-globin gene upstream for approximately 100 kilobases (kb). The A gamma-globin, psi beta-, delta-, and beta-globin genes in cis remained intact. The malfunction of the beta-globin gene on a chromosome in which the deletion is located 25 kb away suggests that chromatin structure and conformation are important for globin gene expression. Find the latest version: https://jci.me/112136/pdf A Distant Gene Deletion Affects ,8-Globin Gene Function in an Atypical '6y5-Thalassemia Peter Curtin, Mario Pirastu, and Yuet Wai Kan Howard Hughes Medical Institute and Department ofMedicine, University of California, San Francisco, California 94143 John Anderson Gobert-Jones Department ofPathology, West Suffolk County Hospital, Bury St. Edmunds IP33-2QZ, Suffolk, England Adrian David Stephens Department ofHaematology, St. Bartholomew's Hospital, London ECIA-7BE, England Herman Lehmann Department ofBiochemistry, University ofCambridge, Cambridge CB2-lQW, England Abstract tologic picture of f3-thalassemia minor in adult life. Globin syn- thetic studies reveal a ,3 to a ratio of -0.5, but unlike the usual We describe an English family with an atypical 'yS6-thalassemia fl-thalassemia heterozygote, the levels of HbA2 (and HbF) are syndrome. -

Physiology & Biophysics
DEPARTMENTAL RESOURCES The Department of Physiology & Biophysics plays a unique role in biological research. It is in effect a conduit through which the powerful techniques and tools of the physical sciences are brought to bear on significant problems of biological importance. The range of problems being addressed in the Department runs the gamut from understanding functionally important atomic scale motions of proteins to characterizing complex behavior on the cellular through organelle level. The tools being used to pursue these cutting edge problems include state of the art instrumentation for magnetic resonance, laser and synchrotron radiation spectroscopies as well as extensive computer modeling. The strength of the Department stems not only from the significant problems that are being aggressively addressed by the departmental faculty, but also from the resources and the collaborative spirit with the department. The Department houses several world class spectroscopy facilities: Biomolecular Laser Research Center (BLRC) The BLRC is composed of three interrelated laser oriented facilities. The laser spectroscopy facility (LSF) contains an extensive array of state-of-the-art laser spectroscopic tools devoted to studying structure, function and dynamics in isolated biomolecules. The laser imaging and microscopy facility (L1MF) focuses on interfacing laser spectroscopy with microscopy to study complex systems at the molecular level. The third facility, devoted to laser based diagnostic tools for clinical applications, is still in the development stage. Pulsed EPR Facility The EPR facility consists of a number of state-of-the-art spectrometers that have been constructed at Einstein. Both theoretical work and experiments are being carried out to define the structure of metal binding sites in metalloproteins and to determine the orientation and distance of substrates to metal centers at active sites of metalloenzymes. -

8.5 X12.5 Doublelines.P65
Cambridge University Press 978-0-521-87519-6 - Disorders of Hemoglobin: Genetics, Pathophysiology, and Clinical Management, Second Edition Edited by Martin H. Steinberg, Bernard G. Forget, Douglas R. Higgs and David J. Weatherall Index More information anti-inflammatory therapy, 762–763 thalassemia-related complications, 779 sulfasalazine, nuclear factor (NF)-kB, 762 transplant-related complications, 778–779 targeting ET-1, 762–763 S-linked haplotypes, African/Indo-European, anti-oxidant therapy targeting erythrocyte, 638–640 765–766 burst forming unit-erythroid (BFU-E), 10, 29 deferiprone, 765 oral glutamine, 765 calcium-activated potassium channel (Gardos oral N-acetyl-cysteine, 765–766 pathway), 167–168 anti-oxidant therapy targeting vascular, 763–765 capillary electrophoresis, 660 Index Apo A-I mimetics, 764 capillary IEF, 660 NO, 763–764 carbon monoxide poisoning, 613–616 statins, 764 clinical features, 615 xanthine oxidase inhibitors, 764–765 diagnosis, treatment, 615–616 anti-thrombotic therapy epidemiology, 613–614 -thalassemia, 761–762 cardiac, arterial abnormalities, 151 sickle cell disease, 761–762 cardiac abnormalities, ATRX syndrome, 305 aortagonad-mesonephros (AGM), 6 cardiovascular disease, 652 Apo A-I mimetics, 764 cation content, cellular hydration, 164–172 apoptosis, vasculature permeability, 193–194 calcium-activated potassium channel, 167–168 assays, assay systems, 7, 142 cation permeability alterations, 166–167 ATMDS. See ␣ thalassemia-myelodysplastic cell calcium, calcium pump activity, 167 syndromes cell sodium, -

Your Baby Has Hemoglobin E Or Hemoglobin O Trait for Parents
NEW HAMPSHIRE NEWBORN SCREENING PROGRAM Your Baby Has Hemoglobin E or Hemoglobin O Trait For Parents All infants born in New Hampshire are screened for a panel of conditions at birth. A small amount of blood was collected from your baby’s heel and sent to the laboratory for testing. One of the tests looked at the hemoglobin in your baby’s blood. Your baby’s test found that your baby has either hemoglobin E trait or hemoglobin O trait. The newborn screen- ing test cannot tell the difference between hemoglobin E and hemoglobin O so we do not know which one your baby has. Both hemoglobin E trait and hemoglobin O trait are common and do not cause health problems. Hemoglobin E trait and hemoglobin O trait will never develop to disease. What is hemoglobin? Hemoglobin is the part of the blood that carries oxygen to all parts of the body. There are different types of hemoglobin. The type of hemoglobin we have is determined from genes that we inherit from our parents. Genes are the instructions for how our body develops and functions. We have two copies of each gene; one copy is inherited from our mother in the egg and one copy is inherited from our father in the sperm. What are hemoglobin E trait and hemoglobin O trait? The normal, and most common, type of hemoglobin is called hemoglobin A. Hemoglobin E trait is when a baby inherited one gene for hemoglobin A from one parent and one gene for hemoglobin E from the other parent. -

Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies
Journal of Clinical Medicine Article Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies Coralea Stephanou, Stella Tamana , Anna Minaidou, Panayiota Papasavva, , , Marina Kleanthous * y and Petros Kountouris * y Molecular Genetics Thalassaemia Department, The Cyprus Institute of Neurology and Genetics, Nicosia 2371, Cyprus; [email protected] (C.S.); [email protected] (S.T.); [email protected] (A.M.); [email protected] (P.P.) * Correspondence: [email protected] (M.K.); [email protected] (P.K.); Tel.:+357-2239-2652 (M.K.); +357-2239-2623 (P.K.) Equal contribution; Joint last authorship. y Received: 20 September 2019; Accepted: 5 November 2019; Published: 9 November 2019 Abstract: Haemoglobinopathies are common monogenic disorders with diverse clinical manifestations, partly attributed to the influence of modifier genes. Recent years have seen enormous growth in the amount of genetic data, instigating the need for ranking methods to identify candidate genes with strong modifying effects. Here, we present the first evidence-based gene ranking metric (IthaScore) for haemoglobinopathy-specific phenotypes by utilising curated data in the IthaGenes database. IthaScore successfully reflects current knowledge for well-established disease modifiers, while it can be dynamically updated with emerging evidence. Protein–protein interaction (PPI) network analysis and functional enrichment analysis were employed to identify new potential disease modifiers and to evaluate the biological profiles of selected phenotypes. The most relevant gene ontology (GO) and pathway gene annotations for (a) haemoglobin (Hb) F levels/Hb F response to hydroxyurea included urea cycle, arginine metabolism and vascular endothelial growth factor receptor (VEGFR) signalling, (b) response to iron chelators included xenobiotic metabolism and glucuronidation, and (c) stroke included cytokine signalling and inflammatory reactions. -

Hemoglobin C Harlem Or Hemoglobin O Arab Trait- for Physicians
New Hampshire Newborn Screening Program Hemoglobin C harlem or hemoglobin O arab Trait- For Physicians As part of routine newborn screening all babies are tested for sickle cell disease and other hemoglobinopathies. Screening of all specimens is done by isoelectric focusing (IEF). Results are then confirmed by IEF and citrate agar electrophoresis. Your patient has tested positive for hemoglobin C harlem trait or hemoglobin O arab trait. Our testing methods are unable to distinguish between hemoglobin C harlem, hemoglobin O arab and other variants that migrate in the same region. Although there is no immediate clinical significance, this information is important for future reproductive decisions of the child and other family members. Possible Newborn Screening Results: Hemoglobin F Fetal hemoglobin, present in declining amounts until 6 months after birth A Normal adult hemoglobin B Hemoglobin Bart’s H Hemoglobin C Harlem or Hemoglobin O arab FA: Normal newborn hemoglobin pattern FAH: Hemoglobin C Harlem trait OR hemoglobin O arab trait FACB: Hemoglobin C trait with Hemoglobin Bart’s (see separate Hemoglobin Bart’s information sheet) Follow Up Recommendations: Newborn screening cannot make a distinction between Hemoglobin C Harlem and O arab. The baby should have a CBC and hemoglobin electrophoresis to verify the NBS results and to help distinguish between hemoglobin C harlem trait and hemoglobin O arab trait. The testing can be performed anytime after fetal hemoglobin levels normalize, which occurs at approximately 6 months of age. The family should be offered genetic counseling for parental testing to assess the risk to future pregnancies and to discuss the inheritance of Hemoglobin C.