An Autoantigen-Ome from HS-Sultan B-Lymphoblasts Offers a Molecular Map for Investigating Autoimmune Sequelae of COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Histone Isoform H2A1H Promotes Attainment of Distinct Physiological
Bhattacharya et al. Epigenetics & Chromatin (2017) 10:48 DOI 10.1186/s13072-017-0155-z Epigenetics & Chromatin RESEARCH Open Access Histone isoform H2A1H promotes attainment of distinct physiological states by altering chromatin dynamics Saikat Bhattacharya1,4,6, Divya Reddy1,4, Vinod Jani5†, Nikhil Gadewal3†, Sanket Shah1,4, Raja Reddy2,4, Kakoli Bose2,4, Uddhavesh Sonavane5, Rajendra Joshi5 and Sanjay Gupta1,4* Abstract Background: The distinct functional efects of the replication-dependent histone H2A isoforms have been dem- onstrated; however, the mechanistic basis of the non-redundancy remains unclear. Here, we have investigated the specifc functional contribution of the histone H2A isoform H2A1H, which difers from another isoform H2A2A3 in the identity of only three amino acids. Results: H2A1H exhibits varied expression levels in diferent normal tissues and human cancer cell lines (H2A1C in humans). It also promotes cell proliferation in a context-dependent manner when exogenously overexpressed. To uncover the molecular basis of the non-redundancy, equilibrium unfolding of recombinant H2A1H-H2B dimer was performed. We found that the M51L alteration at the H2A–H2B dimer interface decreases the temperature of melting of H2A1H-H2B by ~ 3 °C as compared to the H2A2A3-H2B dimer. This diference in the dimer stability is also refected in the chromatin dynamics as H2A1H-containing nucleosomes are more stable owing to M51L and K99R substitu- tions. Molecular dynamic simulations suggest that these substitutions increase the number of hydrogen bonds and hydrophobic interactions of H2A1H, enabling it to form more stable nucleosomes. Conclusion: We show that the M51L and K99R substitutions, besides altering the stability of histone–histone and histone–DNA complexes, have the most prominent efect on cell proliferation, suggesting that the nucleosome sta- bility is intimately linked with the physiological efects observed. -

Molecular Genetic Delineation of 2Q37.3 Deletion in Autism and Osteodystrophy: Report of a Case and of New Markers for Deletion Screening by PCR
UC Irvine UC Irvine Previously Published Works Title Molecular genetic delineation of 2q37.3 deletion in autism and osteodystrophy: report of a case and of new markers for deletion screening by PCR. Permalink https://escholarship.org/uc/item/83f0x61r Journal Cytogenetics and cell genetics, 94(1-2) ISSN 0301-0171 Authors Smith, M Escamilla, JR Filipek, P et al. Publication Date 2001 DOI 10.1159/000048775 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Original Article Cytogenet Cell Genet 94:15–22 (2001) Molecular genetic delineation of 2q37.3 deletion in autism and osteodystrophy: report of a case and of new markers for deletion screening by PCR M. Smith, J.R. Escamilla, P. Filipek, M.E. Bocian, C. Modahl, P. Flodman, and M.A. Spence Department of Pediatrics, University of California, Irvine CA (USA) Abstract. We recently studied a patient who meets criteria us to determine the parental origin of the deletion in our for autistic disorder and has a 2q37 deletion. Molecular cyto- patient. DNA from 8–13 unrelated individuals was used to genetic studies were carried out using DNA isolated from 22 determine heterozygosity estimates for these markers. We re- different 2q37 mapped BACs to more precisely define the view four genes deleted in our patient – genes whose known extent of the chromosome deletion. We also analyzed 2q37 functions and sites of expression in the brain and/or bone make mapped polymorphic markers. In addition DNA sequences of them candidates for involvement in autism and/or the osteo- BACs in the deletion region were scanned to identify microsa- dystrophy observed in patients with 2q37.3 deletions. -

Genomic Correlates of Relationship QTL Involved in Fore- Versus Hind Limb Divergence in Mice
Loyola University Chicago Loyola eCommons Biology: Faculty Publications and Other Works Faculty Publications 2013 Genomic Correlates of Relationship QTL Involved in Fore- Versus Hind Limb Divergence in Mice Mihaela Palicev Gunter P. Wagner James P. Noonan Benedikt Hallgrimsson James M. Cheverud Loyola University Chicago, [email protected] Follow this and additional works at: https://ecommons.luc.edu/biology_facpubs Part of the Biology Commons Recommended Citation Palicev, M, GP Wagner, JP Noonan, B Hallgrimsson, and JM Cheverud. "Genomic Correlates of Relationship QTL Involved in Fore- Versus Hind Limb Divergence in Mice." Genome Biology and Evolution 5(10), 2013. This Article is brought to you for free and open access by the Faculty Publications at Loyola eCommons. It has been accepted for inclusion in Biology: Faculty Publications and Other Works by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. © Palicev et al., 2013. GBE Genomic Correlates of Relationship QTL Involved in Fore- versus Hind Limb Divergence in Mice Mihaela Pavlicev1,2,*, Gu¨ nter P. Wagner3, James P. Noonan4, Benedikt Hallgrı´msson5,and James M. Cheverud6 1Konrad Lorenz Institute for Evolution and Cognition Research, Altenberg, Austria 2Department of Pediatrics, Cincinnati Children‘s Hospital Medical Center, Cincinnati, Ohio 3Yale Systems Biology Institute and Department of Ecology and Evolutionary Biology, Yale University 4Department of Genetics, Yale University School of Medicine 5Department of Cell Biology and Anatomy, The McCaig Institute for Bone and Joint Health and the Alberta Children’s Hospital Research Institute for Child and Maternal Health, University of Calgary, Calgary, Canada 6Department of Anatomy and Neurobiology, Washington University *Corresponding author: E-mail: [email protected]. -

Design of a Bioactive Small Molecule That Targets R(AUUCU) Repeats in Spinocerebellar Ataxia 10
ARTICLE Received 24 Jun 2015 | Accepted 18 Apr 2016 | Published 1 Jun 2016 DOI: 10.1038/ncomms11647 OPEN Design of a bioactive small molecule that targets r(AUUCU) repeats in spinocerebellar ataxia 10 Wang-Yong Yang1, Rui Gao2, Mark Southern3, Partha S. Sarkar2 & Matthew D. Disney1 RNA is an important target for chemical probes of function and lead therapeutics; however, it is difficult to target with small molecules. One approach to tackle this problem is to identify compounds that target RNA structures and utilize them to multivalently target RNA. Here we show that small molecules can be identified to selectively bind RNA base pairs by probing a library of RNA-focused small molecules. A small molecule that selectively binds AU base pairs informed design of a dimeric compound (2AU-2) that targets the pathogenic RNA, expanded r(AUUCU) repeats, that causes spinocerebellar ataxia type 10 (SCA10) in patient- derived cells. Indeed, 2AU-2 (50 nM) ameliorates various aspects of SCA10 pathology including improvement of mitochondrial dysfunction, reduced activation of caspase 3, and reduction of nuclear foci. These studies provide a first-in-class chemical probe to study SCA10 RNA toxicity and potentially define broadly applicable compounds targeting RNA AU base pairs in cells. 1 Departments of Chemistry and Neuroscience, The Scripps Research Institute, Scripps Florida, Jupiter, Florida 33458, USA. 2 Mitchell Center for Neurodegenerative Disorders, Department of Neurology, Neuroscience and Cell Biology, University of Texas Medical Branch, Galveston, Texas 77555, USA. 3 Informatics Core, The Scripps Research Institute, Scripps Florida, Jupiter, Florida 33458, USA. Correspondence and requests for materials should be addressed to M.D.D. -

Environmental Influences on Endothelial Gene Expression
ENDOTHELIAL CELL GENE EXPRESSION John Matthew Jeff Herbert Supervisors: Prof. Roy Bicknell and Dr. Victoria Heath PhD thesis University of Birmingham August 2012 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. ABSTRACT Tumour angiogenesis is a vital process in the pathology of tumour development and metastasis. Targeting markers of tumour endothelium provide a means of targeted destruction of a tumours oxygen and nutrient supply via destruction of tumour vasculature, which in turn ultimately leads to beneficial consequences to patients. Although current anti -angiogenic and vascular targeting strategies help patients, more potently in combination with chemo therapy, there is still a need for more tumour endothelial marker discoveries as current treatments have cardiovascular and other side effects. For the first time, the analyses of in-vivo biotinylation of an embryonic system is performed to obtain putative vascular targets. Also for the first time, deep sequencing is applied to freshly isolated tumour and normal endothelial cells from lung, colon and bladder tissues for the identification of pan-vascular-targets. Integration of the proteomic, deep sequencing, public cDNA libraries and microarrays, delivers 5,892 putative vascular targets to the science community. -

Genome-Wide Analysis of Transcriptional Bursting-Induced Noise in Mammalian Cells
bioRxiv preprint doi: https://doi.org/10.1101/736207; this version posted August 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Title: Genome-wide analysis of transcriptional bursting-induced noise in mammalian cells Authors: Hiroshi Ochiai1*, Tetsutaro Hayashi2, Mana Umeda2, Mika Yoshimura2, Akihito Harada3, Yukiko Shimizu4, Kenta Nakano4, Noriko Saitoh5, Hiroshi Kimura6, Zhe Liu7, Takashi Yamamoto1, Tadashi Okamura4,8, Yasuyuki Ohkawa3, Itoshi Nikaido2,9* Affiliations: 1Graduate School of Integrated Sciences for Life, Hiroshima University, Higashi-Hiroshima, Hiroshima, 739-0046, Japan 2Laboratory for Bioinformatics Research, RIKEN BDR, Wako, Saitama, 351-0198, Japan 3Division of Transcriptomics, Medical Institute of Bioregulation, Kyushu University, Fukuoka, Fukuoka, 812-0054, Japan 4Department of Animal Medicine, National Center for Global Health and Medicine (NCGM), Tokyo, 812-0054, Japan 5Division of Cancer Biology, The Cancer Institute of JFCR, Tokyo, 135-8550, Japan 6Graduate School of Bioscience and Biotechnology, Tokyo Institute of Technology, Yokohama, Kanagawa, 226-8503, Japan 7Janelia Research Campus, Howard Hughes Medical Institute, Ashburn, VA, 20147, USA 8Section of Animal Models, Department of Infectious Diseases, National Center for Global Health and Medicine (NCGM), Tokyo, 812-0054, Japan 9Bioinformatics Course, Master’s/Doctoral Program in Life Science Innovation (T-LSI), School of Integrative and Global Majors (SIGMA), University of Tsukuba, Wako, 351-0198, Japan *Corresponding authors Corresponding authors e-mail addresses Hiroshi Ochiai, [email protected] Itoshi Nikaido, [email protected] bioRxiv preprint doi: https://doi.org/10.1101/736207; this version posted August 15, 2019. -

Identification of Phosphoproteins Involved in Sperm
IDENTIFICATION OF PHOSPHOPROTEINS INVOLVED IN SPERM MATURATION AND FERTILITY. A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Suranjana Goswami August 2018 © Copyright All rights reserved Except for previously published materials Dissertation written by Suranjana Goswami B.Sc., University of Calcutta, India, 2009 M.Sc., University of Calcutta, India 2011 Ph.D., Kent State University, USA, 2018 Approved by Dr. Srinivasan Vijayaraghavan , Chair, Doctoral Dissertation Committee Dr. Douglas W. Kline , Members, Doctoral Dissertation Committee Dr. Gary Koshi , Dr. Sanjaya Abeysirigunawardena , Dr. Andrew Jasnow , Accepted by Dr. Laura G. Leff , Chair, Department of Biological Sciences Dr. James L. Blank , Dean, College of Arts and Sciences TABLE OF CONTENTS ............................................................................................................... iii LIST OF FIGURES ..........................................................................................................................v LIST OF TABLES ....................................................................................................................... viii ABBREVIATIONS ....................................................................................................................... ix DEDICATION ............................................................................................................................... xi ACKNOWLEDGEMENTS ......................................................................................................... -
Somatic Mutational Landscape of AML with Inv(16) Or T(8;21) Identifies Patterns of Clonal Evolution in Relapse Leukemia
Somatic mutational landscape of AML with inv(16) or t(8;21) identifies patterns of clonal evolution in relapse leukemia The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Sood, R., N. F. Hansen, F. X. Donovan, B. Carrington, D. Bucci, B. Maskeri, A. Young, et al. 2015. “Somatic mutational landscape of AML with inv(16) or t(8;21) identifies patterns of clonal evolution in relapse leukemia.” Leukemia 30 (2): 501-504. doi:10.1038/ leu.2015.141. http://dx.doi.org/10.1038/leu.2015.141. Published Version doi:10.1038/leu.2015.141 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:27320188 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Leukemia Manuscript Author . Author manuscript; Manuscript Author available in PMC 2016 May 18. Published in final edited form as: Leukemia. 2016 February ; 30(2): 501–504. doi:10.1038/leu.2015.141. Somatic mutational landscape of AML with inv(16) or t(8;21) identifies patterns of clonal evolution in relapse leukemia Raman Sood1,4, Nancy F. Hansen2, Frank X. Donovan3, Blake Carrington4, Donna Bucci5, Baishali Maskeri6, Alice Young6, Niraj S. Trivedi7, Jessica Kohlschmidt5,8, Richard M. Stone9, Michael A. Caligiuri5, Settara C. Chandrasekharappa3,10, Guido Marcucci5,11, James C. -

An Evaluation of Host Factors As Novel Therapeutic Targets During Influenza Infection Using RNA Technologies
California State University, San Bernardino CSUSB ScholarWorks Electronic Theses, Projects, and Dissertations Office of aduateGr Studies 6-2018 An Evaluation of Host Factors as Novel Therapeutic Targets During Influenza Infection Using RNA Technologies Michael Ryan Haden Thompson California State University - San Bernardino Follow this and additional works at: https://scholarworks.lib.csusb.edu/etd Part of the Virology Commons Recommended Citation Thompson, Michael Ryan Haden, "An Evaluation of Host Factors as Novel Therapeutic Targets During Influenza Infection Using RNA Technologies" (2018). Electronic Theses, Projects, and Dissertations. 721. https://scholarworks.lib.csusb.edu/etd/721 This Thesis is brought to you for free and open access by the Office of aduateGr Studies at CSUSB ScholarWorks. It has been accepted for inclusion in Electronic Theses, Projects, and Dissertations by an authorized administrator of CSUSB ScholarWorks. For more information, please contact [email protected]. AN EVALUATION OF HOST FACTORS AS NOVEL THERAPEUTIC TARGETS DURING INFLUENZA INFECTION USING RNA TECHNOLOGIES _____________________ A Thesis Presented to the Faculty of California State University, San Bernardino _____________________ In Partial Fulfillment of the Requirements for the Degree Master of Science in Biology _____________________ by Michael Ryan Haden Thompson June 2018 AN EVALUATION OF HOST FACTORS AS NOVEL THERAPEUTIC TARGETS DURING INFLUENZA INFECTION USING RNA TECHNOLOGIES _____________________ A Thesis Presented to the Faculty of California State University, San Bernardino _____________________ By Michael Ryan Haden Thompson June 2018 Approved by: Dr. Laura L Newcomb, Committee Chair, Biology Dr. Nicole Bournias-Vardiabasis, Committee Member Dr. Daniel Nickerson, Committee Member © 2018 Michael Ryan Haden Thompson ABSTRACT Influenza A is a single-stranded, multi-segmented, negative sense RNA virus of the family Orthomyxoviridae and is the causative agent of seasonal Influenza. -
Differentially Expressed on Collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All Rights Reserved. Symbol Entrez
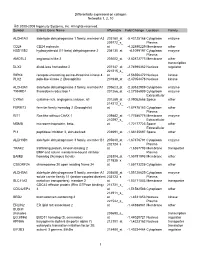
Differentially expressed on collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All rights reserved. Symbol Entrez Gene Name Affymetrix Fold Change Location Family ALDH1A3 aldehyde dehydrogenase 1 family, member A3 203180_at -5.43125168 Cytoplasm enzyme 209772_s_ Plasma CD24 CD24 molecule at -4.32890229 Membrane other HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 204130_at -4.1099197 Cytoplasm enzyme Plasma AMOTL2 angiomotin like 2 203002_at -2.82872773 Membrane other transcription DLX2 distal-less homeobox 2 207147_at -2.74996362 Nucleus regulator 221215_s_ RIPK4 receptor-interacting serine-threonine kinase 4 at -2.56556472 Nucleus kinase PLK2 polo-like kinase 2 (Drosophila) 201939_at -2.47054478 Nucleus kinase ALDH3A1 aldehyde dehydrogenase 3 family, memberA1 205623_at -2.30532989 Cytoplasm enzyme TXNRD1 thioredoxin reductase 1 201266_at -2.27936909 Cytoplasm enzyme Extracellular CYR61 cysteine-rich, angiogenic inducer, 61 201289_at -2.09052668 Space other 214212_x_ FERMT2 fermitin family homolog 2 (Drosophila) at -1.87478183 Cytoplasm other Plasma RIT1 Ras-like without CAAX 1 209882_at -1.77586775 Membrane enzyme 210297_s_ Extracellular MSMB microseminoprotein, beta- at -1.72177723 Space other Extracellular PI3 peptidase inhibitor 3, skin-derived 203691_at -1.68135697 Space other ALDH3B1 aldehyde dehydrogenase 3 family, member B1 205640_at -1.67376791 Cytoplasm enzyme 202124_s_ Plasma TRAK2 trafficking protein, kinesin binding 2 at -1.6367793 Membrane transporter BMP and activin membrane-bound inhibitor Plasma BAMBI -

Recent Advances in Drosophila Models of Charcot-Marie-Tooth Disease
International Journal of Molecular Sciences Review Recent Advances in Drosophila Models of Charcot-Marie-Tooth Disease Fukiko Kitani-Morii 1,2,* and Yu-ichi Noto 2 1 Department of Molecular Pathobiology of Brain Disease, Kyoto Prefectural University of Medicine, Kyoto 6028566, Japan 2 Department of Neurology, Kyoto Prefectural University of Medicine, Kyoto 6028566, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-75-251-5793 Received: 31 August 2020; Accepted: 6 October 2020; Published: 8 October 2020 Abstract: Charcot-Marie-Tooth disease (CMT) is one of the most common inherited peripheral neuropathies. CMT patients typically show slowly progressive muscle weakness and sensory loss in a distal dominant pattern in childhood. The diagnosis of CMT is based on clinical symptoms, electrophysiological examinations, and genetic testing. Advances in genetic testing technology have revealed the genetic heterogeneity of CMT; more than 100 genes containing the disease causative mutations have been identified. Because a single genetic alteration in CMT leads to progressive neurodegeneration, studies of CMT patients and their respective models revealed the genotype-phenotype relationships of targeted genes. Conventionally, rodents and cell lines have often been used to study the pathogenesis of CMT. Recently, Drosophila has also attracted attention as a CMT model. In this review, we outline the clinical characteristics of CMT, describe the advantages and disadvantages of using Drosophila in CMT studies, and introduce recent advances in CMT research that successfully applied the use of Drosophila, in areas such as molecules associated with mitochondria, endosomes/lysosomes, transfer RNA, axonal transport, and glucose metabolism. -

Mir-17-92 Fine-Tunes MYC Expression and Function to Ensure
ARTICLE Received 31 Mar 2015 | Accepted 22 Sep 2015 | Published 10 Nov 2015 DOI: 10.1038/ncomms9725 OPEN miR-17-92 fine-tunes MYC expression and function to ensure optimal B cell lymphoma growth Marija Mihailovich1, Michael Bremang1, Valeria Spadotto1, Daniele Musiani1, Elena Vitale1, Gabriele Varano2,w, Federico Zambelli3, Francesco M. Mancuso1,w, David A. Cairns1,w, Giulio Pavesi3, Stefano Casola2 & Tiziana Bonaldi1 The synergism between c-MYC and miR-17-19b, a truncated version of the miR-17-92 cluster, is well-documented during tumor initiation. However, little is known about miR-17-19b function in established cancers. Here we investigate the role of miR-17-19b in c-MYC-driven lymphomas by integrating SILAC-based quantitative proteomics, transcriptomics and 30 untranslated region (UTR) analysis upon miR-17-19b overexpression. We identify over one hundred miR-17-19b targets, of which 40% are co-regulated by c-MYC. Downregulation of a new miR-17/20 target, checkpoint kinase 2 (Chek2), increases the recruitment of HuR to c- MYC transcripts, resulting in the inhibition of c-MYC translation and thus interfering with in vivo tumor growth. Hence, in established lymphomas, miR-17-19b fine-tunes c-MYC activity through a tight control of its function and expression, ultimately ensuring cancer cell homeostasis. Our data highlight the plasticity of miRNA function, reflecting changes in the mRNA landscape and 30 UTR shortening at different stages of tumorigenesis. 1 Department of Experimental Oncology, European Institute of Oncology, Via Adamello 16, Milan 20139, Italy. 2 Units of Genetics of B cells and lymphomas, IFOM, FIRC Institute of Molecular Oncology Foundation, Milan 20139, Italy.