Autosomal Dominant Cerebellar Ataxia Type I: a Review of the Phenotypic and Genotypic Characteristics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Detrusor Sphincter Dyssynergia: a Review of Physiology, Diagnosis, and Treatment Strategies
Review Article Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies John T. Stoffel Department of Urology, University of Michigan, Ann Arbor, MI, USA Correspondence to: John T. Stoffel, MD. Department of Urology, University of Michigan, Ann Arbor, MI, USA. Email: [email protected]. Abstract: Detrusor sphincter dyssynergia (DSD) is the urodynamic description of bladder outlet obstruction from detrusor muscle contraction with concomitant involuntary urethral sphincter activation. DSD is associated with neurologic conditions such as spinal cord injury, multiple sclerosis, and spina bifida and some of these neurogenic bladder patients with DSD may be at risk for autonomic dysreflexia, recurrent urinary tract infections, or upper tract compromise if the condition is not followed and treated appropriately. It is diagnosed most commonly during the voiding phase of urodynamic studies using EMG recordings and voiding cystourethrograms, although urethral pressure monitoring could also potentially be used. DSD can be sub-classified as either continuous or intermittent, although adoption of this terminology is not widespread. There are few validated oral pharmacologic treatment options for this condition but transurethral botulinum toxin injection have shown temporary efficacy in reducing bladder outlet obstruction. Urinary sphincterotomy has also demonstrated reproducible long term benefits in several studies, but the morbidity associated with this procedure can be high. Keywords: Detrusor sphincter dyssynergia (DSD); neurogenic bladder; urodynamics; external urinary sphincter (EUS) Submitted Nov 30, 2015. Accepted for publication Jan 05, 2016. doi: 10.3978/j.issn.2223-4683.2016.01.08 View this article at: http://dx.doi.org/10.3978/j.issn.2223-4683.2016.01.08 Introduction Physiology The human bladder has two functions—to store and During storage of urine, afferent nerves carry information empty urine. -

Acute Cerebellar Ataxia Associated with Intermittent ECG Pattern Similar to Wellens Syndrome and Transient Prominent QRS Anterior Forces
Acute cerebellar ataxia associated with intermittent ECG pattern similar to Wellens syndrome and transient prominent QRS anterior forces Andrés Ricardo Pérez-Riera, MD, PhD. Post-Graduates Advisor at Design of Studies and Scientific Writing Laboratory in the ABC Faculty of Medicine - ABC Foundation - Santo André – São Paulo – Brazil Raimundo Barbosa-Barros, MD. Specialist in Cardiology by the Brazilian Society of Cardiology (SBC) Specialist in Intensive Care by the Sociedade Brasileira de Terapia Intensiva Chief of the Coronary Center of the Hospital de Messejana Dr. Carlos Alberto Studart Gomes. Fortaleza - Brazil Adrian Baranchuk, MD FACC FRCPC Associate Professor of Medicine and Physiology - Cardiac Electrophysiology and Pacing - Director, EP Training Program - Kingston General Hospital - FAPC 3, 76 Stuart Street K7L 2V7, Kingston ON Queen's University - Canada Male patient, 56 years old, white, uncontrolled hypertension, was admitted to our emergency department (ED) with reports of sudden dizziness, headache of abrupt onset, nausea, vomiting and weakness in the lower limbs. Physical examination drew attention to the presence of manifestations suggestive of cerebellar syndrome: impaired coordination in the trunk or arms and legs, inability to coordinate balance, gait, extremity, uncontrolled or repetitive eye movements, (nystagmus), dyssynergia, dysmetria, dysdiadochokinesia, dysarthria (cerebellar ataxia). Normal myocardial necrosis markers and normal electrolytes ECO 1: anteroseptal-apical akinesis; LVEF = 30% ECO 2 (third day): -

Design of a Bioactive Small Molecule That Targets R(AUUCU) Repeats in Spinocerebellar Ataxia 10
ARTICLE Received 24 Jun 2015 | Accepted 18 Apr 2016 | Published 1 Jun 2016 DOI: 10.1038/ncomms11647 OPEN Design of a bioactive small molecule that targets r(AUUCU) repeats in spinocerebellar ataxia 10 Wang-Yong Yang1, Rui Gao2, Mark Southern3, Partha S. Sarkar2 & Matthew D. Disney1 RNA is an important target for chemical probes of function and lead therapeutics; however, it is difficult to target with small molecules. One approach to tackle this problem is to identify compounds that target RNA structures and utilize them to multivalently target RNA. Here we show that small molecules can be identified to selectively bind RNA base pairs by probing a library of RNA-focused small molecules. A small molecule that selectively binds AU base pairs informed design of a dimeric compound (2AU-2) that targets the pathogenic RNA, expanded r(AUUCU) repeats, that causes spinocerebellar ataxia type 10 (SCA10) in patient- derived cells. Indeed, 2AU-2 (50 nM) ameliorates various aspects of SCA10 pathology including improvement of mitochondrial dysfunction, reduced activation of caspase 3, and reduction of nuclear foci. These studies provide a first-in-class chemical probe to study SCA10 RNA toxicity and potentially define broadly applicable compounds targeting RNA AU base pairs in cells. 1 Departments of Chemistry and Neuroscience, The Scripps Research Institute, Scripps Florida, Jupiter, Florida 33458, USA. 2 Mitchell Center for Neurodegenerative Disorders, Department of Neurology, Neuroscience and Cell Biology, University of Texas Medical Branch, Galveston, Texas 77555, USA. 3 Informatics Core, The Scripps Research Institute, Scripps Florida, Jupiter, Florida 33458, USA. Correspondence and requests for materials should be addressed to M.D.D. -

Neurogenic Bowel Dysfunction in Patients with Multiple Sclerosis Open Access to Scientific and Medical Research DOI
Journal name: Degenerative Neurological and Neuromuscular Disease Article Designation: Review Year: 2018 Volume: 8 Degenerative Neurological and Neuromuscular Disease Dovepress Running head verso: Preziosi et al Running head recto: Neurogenic bowel dysfunction in patients with multiple sclerosis open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DNND.S138835 Open Access Full Text Article REVIEW Neurogenic bowel dysfunction in patients with multiple sclerosis: prevalence, impact, and management strategies Giuseppe Preziosi Abstract: Bowel dysfunction in patients with multiple sclerosis (MS) is highly prevalent. Ayeshah Gordon-Dixon Constipation and fecal incontinence can coexist and alternate, impacting on the patient’s quality Anton Emmanuel of life and social interactions, as well as burdening the caregivers. The cost for the health care providers is also significant, with increased number of hospital admissions, treatment-related Gastro-Intestinal Physiology Unit, University College London Hospital, costs, and hospital appointments. The origin is multifactorial, and includes alteration of neu- London, UK rological pathways, polypharmacy, behavioral elements, and ability to access the toilet. Every patient with MS should be sensitively questioned about bowel function, and red flag symptoms should prompt adequate investigations. Manipulation of life style factors and establishment of a bowel regime should be attempted in the first place, and if this fails, other measures such For personal use only. as biofeedback and transanal irrigation should be included. A stoma can improve quality of life, and is not necessarily a last-ditch option. Antegrade colonic enemas can also be an effec- tive option, whilst neuromodulation has not proved its role yet. Effective treatment of bowel dysfunction improves quality of life, reduces incidence of urinary tract infection, and reduces health care costs. -

Neurodegenerative Triplet Repeat Expansion Disorders
The Pharma Innovation Journal 2018; 7(11): 34-40 ISSN (E): 2277- 7695 ISSN (P): 2349-8242 NAAS Rating: 5.03 Neurodegenerative triplet repeat expansion disorders: TPI 2018; 7(11): 34-40 © 2018 TPI A review www.thepharmajournal.com Received: 15-09-2018 Accepted: 20-10-2018 Mitesh Patel, RK Patel, Tushar Chauhan, Jigar Suthar and Sanjay Dave Mitesh Patel Genetics Group of Gujarat Abstract Diagnostic Centre, Mehsana, Epigenetic alterations are the major causes of triplet repeat expansion. The repetitive DNA expands of its Gujarat, India normal length results in sever neurodegenerative conditions. The common types of triplet repeat expansion (TNE) disorders are: Huntington disease, Friedreich ataxia, myotonic dystrophy, SBMA and RK Patel SCA1 out of which Huntington disease, SBMA and SCA1 are categorized as a poly glutamine disorder Sandor Animal Biogenics Pvt. due to the repeat of CAG. In contrast, the friedreich ataxia is occurred due to expansion of the GAA Ltd., Hyderabad, Telangana, whereas myotonic dystrophy is due to the expansion of CTG. The triplet disease follows the mechanism India of anticipation in which the onset of the disease increases with age. Conclusively, no clear mechanism can explain the origin of the disease. The pre mutation can be expanded in full mutation in successive Tushar Chauhan Genetics Group of Gujarat generations and the number of repeats increased with each generation. TNE can observe in both somatic Diagnostic Centre, Mehsana, as well as germ line tissues. Gujarat, India Keywords: triplet repeat expansion disorder, trinucleotide repeats, Huntington disease, SBMA, SCA1, Jigar Suthar friedreich ataxia Genetics Group of Gujarat Diagnostic Centre, Mehsana, Introduction Gujarat, India Since the early 1990s, a new class of molecular disease has been characterized based upon the Sanjay Dave presence of unstable and abnormal expansions of DNA-triplets (Trinucleotides). -

1 Supporting Information for a Microrna Network Regulates
Supporting Information for A microRNA Network Regulates Expression and Biosynthesis of CFTR and CFTR-ΔF508 Shyam Ramachandrana,b, Philip H. Karpc, Peng Jiangc, Lynda S. Ostedgaardc, Amy E. Walza, John T. Fishere, Shaf Keshavjeeh, Kim A. Lennoxi, Ashley M. Jacobii, Scott D. Rosei, Mark A. Behlkei, Michael J. Welshb,c,d,g, Yi Xingb,c,f, Paul B. McCray Jr.a,b,c Author Affiliations: Department of Pediatricsa, Interdisciplinary Program in Geneticsb, Departments of Internal Medicinec, Molecular Physiology and Biophysicsd, Anatomy and Cell Biologye, Biomedical Engineeringf, Howard Hughes Medical Instituteg, Carver College of Medicine, University of Iowa, Iowa City, IA-52242 Division of Thoracic Surgeryh, Toronto General Hospital, University Health Network, University of Toronto, Toronto, Canada-M5G 2C4 Integrated DNA Technologiesi, Coralville, IA-52241 To whom correspondence should be addressed: Email: [email protected] (M.J.W.); yi- [email protected] (Y.X.); Email: [email protected] (P.B.M.) This PDF file includes: Materials and Methods References Fig. S1. miR-138 regulates SIN3A in a dose-dependent and site-specific manner. Fig. S2. miR-138 regulates endogenous SIN3A protein expression. Fig. S3. miR-138 regulates endogenous CFTR protein expression in Calu-3 cells. Fig. S4. miR-138 regulates endogenous CFTR protein expression in primary human airway epithelia. Fig. S5. miR-138 regulates CFTR expression in HeLa cells. Fig. S6. miR-138 regulates CFTR expression in HEK293T cells. Fig. S7. HeLa cells exhibit CFTR channel activity. Fig. S8. miR-138 improves CFTR processing. Fig. S9. miR-138 improves CFTR-ΔF508 processing. Fig. S10. SIN3A inhibition yields partial rescue of Cl- transport in CF epithelia. -
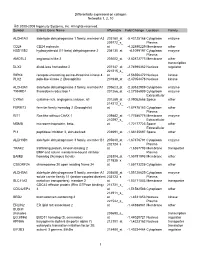
Differentially Expressed on Collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All Rights Reserved. Symbol Entrez
Differentially expressed on collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All rights reserved. Symbol Entrez Gene Name Affymetrix Fold Change Location Family ALDH1A3 aldehyde dehydrogenase 1 family, member A3 203180_at -5.43125168 Cytoplasm enzyme 209772_s_ Plasma CD24 CD24 molecule at -4.32890229 Membrane other HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 204130_at -4.1099197 Cytoplasm enzyme Plasma AMOTL2 angiomotin like 2 203002_at -2.82872773 Membrane other transcription DLX2 distal-less homeobox 2 207147_at -2.74996362 Nucleus regulator 221215_s_ RIPK4 receptor-interacting serine-threonine kinase 4 at -2.56556472 Nucleus kinase PLK2 polo-like kinase 2 (Drosophila) 201939_at -2.47054478 Nucleus kinase ALDH3A1 aldehyde dehydrogenase 3 family, memberA1 205623_at -2.30532989 Cytoplasm enzyme TXNRD1 thioredoxin reductase 1 201266_at -2.27936909 Cytoplasm enzyme Extracellular CYR61 cysteine-rich, angiogenic inducer, 61 201289_at -2.09052668 Space other 214212_x_ FERMT2 fermitin family homolog 2 (Drosophila) at -1.87478183 Cytoplasm other Plasma RIT1 Ras-like without CAAX 1 209882_at -1.77586775 Membrane enzyme 210297_s_ Extracellular MSMB microseminoprotein, beta- at -1.72177723 Space other Extracellular PI3 peptidase inhibitor 3, skin-derived 203691_at -1.68135697 Space other ALDH3B1 aldehyde dehydrogenase 3 family, member B1 205640_at -1.67376791 Cytoplasm enzyme 202124_s_ Plasma TRAK2 trafficking protein, kinesin binding 2 at -1.6367793 Membrane transporter BMP and activin membrane-bound inhibitor Plasma BAMBI -

Supplemental Information
Supplemental information Dissection of the genomic structure of the miR-183/96/182 gene. Previously, we showed that the miR-183/96/182 cluster is an intergenic miRNA cluster, located in a ~60-kb interval between the genes encoding nuclear respiratory factor-1 (Nrf1) and ubiquitin-conjugating enzyme E2H (Ube2h) on mouse chr6qA3.3 (1). To start to uncover the genomic structure of the miR- 183/96/182 gene, we first studied genomic features around miR-183/96/182 in the UCSC genome browser (http://genome.UCSC.edu/), and identified two CpG islands 3.4-6.5 kb 5’ of pre-miR-183, the most 5’ miRNA of the cluster (Fig. 1A; Fig. S1 and Seq. S1). A cDNA clone, AK044220, located at 3.2-4.6 kb 5’ to pre-miR-183, encompasses the second CpG island (Fig. 1A; Fig. S1). We hypothesized that this cDNA clone was derived from 5’ exon(s) of the primary transcript of the miR-183/96/182 gene, as CpG islands are often associated with promoters (2). Supporting this hypothesis, multiple expressed sequences detected by gene-trap clones, including clone D016D06 (3, 4), were co-localized with the cDNA clone AK044220 (Fig. 1A; Fig. S1). Clone D016D06, deposited by the German GeneTrap Consortium (GGTC) (http://tikus.gsf.de) (3, 4), was derived from insertion of a retroviral construct, rFlpROSAβgeo in 129S2 ES cells (Fig. 1A and C). The rFlpROSAβgeo construct carries a promoterless reporter gene, the β−geo cassette - an in-frame fusion of the β-galactosidase and neomycin resistance (Neor) gene (5), with a splicing acceptor (SA) immediately upstream, and a polyA signal downstream of the β−geo cassette (Fig. -

Abadie's Sign Abadie's Sign Is the Absence Or Diminution of Pain Sensation When Exerting Deep Pressure on the Achilles Tendo
A.qxd 9/29/05 04:02 PM Page 1 A Abadie’s Sign Abadie’s sign is the absence or diminution of pain sensation when exerting deep pressure on the Achilles tendon by squeezing. This is a frequent finding in the tabes dorsalis variant of neurosyphilis (i.e., with dorsal column disease). Cross References Argyll Robertson pupil Abdominal Paradox - see PARADOXICAL BREATHING Abdominal Reflexes Both superficial and deep abdominal reflexes are described, of which the superficial (cutaneous) reflexes are the more commonly tested in clinical practice. A wooden stick or pin is used to scratch the abdomi- nal wall, from the flank to the midline, parallel to the line of the der- matomal strips, in upper (supraumbilical), middle (umbilical), and lower (infraumbilical) areas. The maneuver is best performed at the end of expiration when the abdominal muscles are relaxed, since the reflexes may be lost with muscle tensing; to avoid this, patients should lie supine with their arms by their sides. Superficial abdominal reflexes are lost in a number of circum- stances: normal old age obesity after abdominal surgery after multiple pregnancies in acute abdominal disorders (Rosenbach’s sign). However, absence of all superficial abdominal reflexes may be of localizing value for corticospinal pathway damage (upper motor neu- rone lesions) above T6. Lesions at or below T10 lead to selective loss of the lower reflexes with the upper and middle reflexes intact, in which case Beevor’s sign may also be present. All abdominal reflexes are preserved with lesions below T12. Abdominal reflexes are said to be lost early in multiple sclerosis, but late in motor neurone disease, an observation of possible clinical use, particularly when differentiating the primary lateral sclerosis vari- ant of motor neurone disease from multiple sclerosis. -

Appendix 2. Significantly Differentially Regulated Genes in Term Compared with Second Trimester Amniotic Fluid Supernatant
Appendix 2. Significantly Differentially Regulated Genes in Term Compared With Second Trimester Amniotic Fluid Supernatant Fold Change in term vs second trimester Amniotic Affymetrix Duplicate Fluid Probe ID probes Symbol Entrez Gene Name 1019.9 217059_at D MUC7 mucin 7, secreted 424.5 211735_x_at D SFTPC surfactant protein C 416.2 206835_at STATH statherin 363.4 214387_x_at D SFTPC surfactant protein C 295.5 205982_x_at D SFTPC surfactant protein C 288.7 1553454_at RPTN repetin solute carrier family 34 (sodium 251.3 204124_at SLC34A2 phosphate), member 2 238.9 206786_at HTN3 histatin 3 161.5 220191_at GKN1 gastrokine 1 152.7 223678_s_at D SFTPA2 surfactant protein A2 130.9 207430_s_at D MSMB microseminoprotein, beta- 99.0 214199_at SFTPD surfactant protein D major histocompatibility complex, class II, 96.5 210982_s_at D HLA-DRA DR alpha 96.5 221133_s_at D CLDN18 claudin 18 94.4 238222_at GKN2 gastrokine 2 93.7 1557961_s_at D LOC100127983 uncharacterized LOC100127983 93.1 229584_at LRRK2 leucine-rich repeat kinase 2 HOXD cluster antisense RNA 1 (non- 88.6 242042_s_at D HOXD-AS1 protein coding) 86.0 205569_at LAMP3 lysosomal-associated membrane protein 3 85.4 232698_at BPIFB2 BPI fold containing family B, member 2 84.4 205979_at SCGB2A1 secretoglobin, family 2A, member 1 84.3 230469_at RTKN2 rhotekin 2 82.2 204130_at HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 81.9 222242_s_at KLK5 kallikrein-related peptidase 5 77.0 237281_at AKAP14 A kinase (PRKA) anchor protein 14 76.7 1553602_at MUCL1 mucin-like 1 76.3 216359_at D MUC7 mucin 7, -

Rats and Axolotls Share a Common Molecular Signature After Spinal Cord Injury Enriched in Collagen-1
Rats and axolotls share a common molecular signature after spinal cord injury enriched in collagen-1 Athanasios Didangelos1, Katalin Bartus1, Jure Tica1, Bernd Roschitzki2, Elizabeth J. Bradbury1 1Wolfson CARD King’s College London, United Kingdom. 2Centre for functional Genomics, ETH Zurich, Switzerland. Running title: spinal cord injury in rats and axolotls Correspondence: A Didangelos: [email protected] SUPPLEMENTAL FIGURES AND LEGENDS Supplemental Fig. 1: Rat 7 days microarray differentially regulated transcripts. A-B: Protein-protein interaction networks of upregulated (A) and downregulated (B) transcripts identified by microarray gene expression profiling of rat SCI (4 sham versus 4 injured spinal cord samples) 7 days post-injury. Microarray expression data and experimental information is publicly available online (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE45006) and is also summarised in Supplemental Table 1. Protein-protein interaction networks were performed in StringDB using the full range of protein interaction scores (0.15 – 0.99) to capture maximum evidence of proteins’ interactions. Networks were then further analysed for betweeness centrality and gene ontology (GO) annotations (BinGO) in Cytoscape. Node colour indicates betweeness centrality while edge colour and thickness indicate interaction score based on predicted functional links between nodes (green: low values; red: high values). C-D: The top 10 upregulated (C) or downregulated (D) transcripts sorted by betweeness centrality score in protein-protein interaction networks shown in A & B. E-F: Biological process GO analysis was performed on networks of upregulated and downregulated genes using BinGO in Cytoscape. Graphs indicate the 20 most significant GO categories and the number of genes in each category. -

Whole Genome Sequencing of Familial Non-Medullary Thyroid Cancer Identifies Germline Alterations in MAPK/ERK and PI3K/AKT Signaling Pathways
biomolecules Article Whole Genome Sequencing of Familial Non-Medullary Thyroid Cancer Identifies Germline Alterations in MAPK/ERK and PI3K/AKT Signaling Pathways Aayushi Srivastava 1,2,3,4 , Abhishek Kumar 1,5,6 , Sara Giangiobbe 1, Elena Bonora 7, Kari Hemminki 1, Asta Försti 1,2,3 and Obul Reddy Bandapalli 1,2,3,* 1 Division of Molecular Genetic Epidemiology, German Cancer Research Center (DKFZ), D-69120 Heidelberg, Germany; [email protected] (A.S.); [email protected] (A.K.); [email protected] (S.G.); [email protected] (K.H.); [email protected] (A.F.) 2 Hopp Children’s Cancer Center (KiTZ), D-69120 Heidelberg, Germany 3 Division of Pediatric Neurooncology, German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), D-69120 Heidelberg, Germany 4 Medical Faculty, Heidelberg University, D-69120 Heidelberg, Germany 5 Institute of Bioinformatics, International Technology Park, Bangalore 560066, India 6 Manipal Academy of Higher Education (MAHE), Manipal, Karnataka 576104, India 7 S.Orsola-Malphigi Hospital, Unit of Medical Genetics, 40138 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +49-6221-42-1709 Received: 29 August 2019; Accepted: 10 October 2019; Published: 13 October 2019 Abstract: Evidence of familial inheritance in non-medullary thyroid cancer (NMTC) has accumulated over the last few decades. However, known variants account for a very small percentage of the genetic burden. Here, we focused on the identification of common pathways and networks enriched in NMTC families to better understand its pathogenesis with the final aim of identifying one novel high/moderate-penetrance germline predisposition variant segregating with the disease in each studied family.