AZERBAIJAN NUTRITION SURVEY (Azns), 2013 TABLE of CONTENTS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Volume II, Issue 2, March 2021.Pages
INTERNATIONAL COUNTER-TERRORISM REVIEW VOLUME II, ISSUE 2 February, 2021 The Revival of Islam How Do External Factors Shape the Potential Islamist Threat in Azerbaijan? FUAD SHAHBAZOV ABOUT ICTR The International Counter-Terrorism Review (ICTR) aspires to be the world’s leading student publication in Terrorism & Counter-Terrorism Studies. ICTR provides a unique opportunity for students and young professionals to publish their papers, share innovative ideas, and develop an academic career in Counter-Terrorism Studies. The publication also serves as a platform for exchanging research and policy recommendations addressing theoretical, empirical and policy dimensions of international issues pertaining to terrorism, counter-terrorism, insurgency, counter-insurgency, political violence and homeland security. ICTR is a project jointly initiated by the International Institute for Counter-Terrorism (ICT) at the Interdisciplinary Center (IDC), Herzliya, Israel and NextGen 5.0. The International Institute for Counter-Terrorism (ICT) is one of the leading academic institutes for counter-terrorism in the world. Founded in 1996, ICT has rapidly evolved into a highly esteemed global hub for counter-terrorism research, policy recommendations and education. The goal of the ICT is to advise decision makers, to initiate applied research and to provide high-level consultation, education and training in order to address terrorism and its effects. NextGen 5.0 is a pioneering non-profit, independent, and virtual think tank committed to inspiring and empowering the next generation of peace and security leaders in order to build a more secure and prosperous world. COPYRIGHT This material is offered free of charge for personal and non-commercial use, provided the source is acknowledged. -

Policy Brief Series
The Migration, Environment Migration, Environment and Climate Change: and Climate Change: Policy Brief Series is produced as part of the Migration, Environment and Climate Change: Evidence for Policy (MECLEP) project funded by the European Union, implemented Policy Brief Series by IOM through a consortium with ISSN 2410-4930 Issue 4 | Vol. 2 | April 2016 six research partners. 2012 East Azerbaijan earthquakes © Mardetanha, 2012 Environmental migration and displacement in Azerbaijan: Highlighting the need for research and policies Irene Leonardelli, IOM Introduction From a geological and environmental point of view, the 362). Simultaneously, due to climate change, the country Caucasus region ‒ where the Republic of Azerbaijan is increasingly exposed to slow-onset processes, such (hereafter “Azerbaijan”) is located ‒ is a very active as water scarcity, salinization and pollution, rising and hazardous area; this is mainly reflected in the temperatures, sea-level fluctuation, droughts and soil intensity and the frequency of floods, storms, landslides, degradation. While natural disasters have displaced mudflows and earthquakes (ogli Mammadov, 2012:361, 67,865 people between 2009 and 2014 (IDMC, 2014), the YEARS This project is funded by the This project is implemented by the European Union International Organization for Migration 44_16 Migration, Environment and Climate Change: Policy Brief Series Issue 4 | Vol. 2 | April 2016 2 progressive exacerbation of environmental degradation Extreme weather events and slow-onset is thought to have significant adverse impacts on livelihoods and communities especially in certain areas processes in Azerbaijan of the country. Azerbaijan’s exposure to severe weather events and After gaining independence in 1991 as a result of the negative impacts on the population are increasing. -

World Bank Document
75967 Review of World Bank engagement in the Public Disclosure Authorized Irrigation and Drainage Sector in Azerbaijan Public Disclosure Authorized Public Disclosure Authorized February 2013 Public Disclosure Authorized © 2012 International Bank for Reconstruction and Development / The World Bank 1818 H Street NW Washington DC 20433 Telephone: 202-473-1000I Internet: www.worldbank.org This volume is a product of the staff of the International Bank for Reconstruction and Development/The World Bank. The findings, interpretations, and conclusions expressed in this paper do not necessarily reflect the views of the Executive Directors of The World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of The World Bank concerning the legal status of any territory or the endorsement or acceptance of such boundaries. The material in this publication is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. The International Bank for Reconstruction and Development/The World Bank encourages dissemination of its work and will normally grant permission to reproduce portions of the work promptly. For permission to photocopy or reprint any part of this work, please send a request with complete information to the Copyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923, USA, telephone 978-750-8400, fax 978-750-4470, http://www.copyright.com/. All other queries on rights and licenses, including subsidiary rights, should be addressed to the Office of the Publisher, The World Bank, 1818 H Street NW, Washington, DC 20433, USA, fax 202-522-2422, e-mail [email protected]. -

Azerbaijan Page 1 of 8
Azerbaijan Page 1 of 8 Azerbaijan BUREAU OF DEMOCRACY, HUMAN RIGHTS, AND LABOR International Religious Freedom Report 2009 October 26, 2009 The Constitution provides for freedom of religion. On March 18, 2009, however, a national referendum approved a series of amendments to the Constitution; two amendments limit the spreading of and propagandizing of religion. Additionally, on May 8, 2009, the Milli Majlis (Parliament) passed an amended Law on Freedom of Religion, signed by the President on May 29, 2009, which could result in additional restrictions to the system of registration for religious groups. In spite of these developments, the Government continued to respect the religious freedom of the majority of citizens, with some notable exceptions for members of religions considered nontraditional. There was some deterioration in the status of respect for religious freedom by the Government during the reporting period. There were changes to the Constitution that undermined religious freedom. There were mosque closures, and state- and locally sponsored raids on evangelical Protestant religious groups. There were reports of monitoring by federal and local officials as well as harassment and detention of both Islamic and nontraditional Christian groups. There were reports of discrimination against worshippers based on their religious beliefs, largely conducted by local authorities who detained and questioned worshippers without any legal basis and confiscated religious material. There were sporadic reports of societal abuses or discrimination based on religious affiliation, belief, or practice. There was some prejudice against Muslims who converted to other faiths, and there was occasional hostility toward groups that proselytized, particularly evangelical Christians, and other missionary groups. -

United Nations Economic Commission for Europe for Suggestions and Comments
Unofficial translation* SUMMARY REPORT UNDER THE PROTOCOL ON WATER AND HEALTH THE REPUBLIC OF AZERBAIJAN Part One General aspects 1. Were targets and target dates established in your country in accordance with article 6 of the Protocol? Please provide detailed information on the target areas in Part Three. YES ☐ NO ☐ IN PROGRESS If targets have been revised, please provide details here. 2. Were they published and, if so, how? Please explain whether the targets and target dates were published, made available to the public (e.g. online, official publication, media) and communicated to the secretariat. The draft document on target setting was presented in December 2015 to the WHO Regional Office for Europe and United Nations Economic Commission for Europe for suggestions and comments. After the draft document review, its discussion with the public is planned. To get suggestions and comments it will be made available on the website of Ministry of Ecology and Natural Resources of Azerbaijan Republic and Ministry of Health of Azerbaijan Republic. Azerbaijan Republic ratified the Protocol on Water and Health in 2012 and as a Protocol Party participated in two cycles of the previous reporting. At present the targets project is prepared and sent to the WHO Regional Office for Europe and United Nations Economic Commission for Europe. It should be noted that the seminar to support the progress of setting targets under the Protocol on Water and Health was held in Baku on 29 September 2015. More than 40 representatives of different ministries and agencies, responsible for water and health issues, participated in it. -
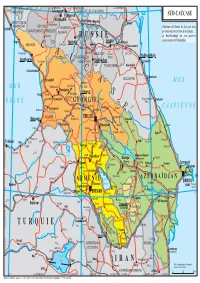
SUD-CAUCASE.Ai
vers RÉP. DES v. PSEBAÏ vers TCHERKESSK vers GUEORGUIEVSK vers ASTRAKHAN 48° TOUAPSÉ ADYGUÉS Essentouki TERRITOIRE DE STAVROPOL ï 44° Piatigorsk Kra novka SUD-CAUCASE Kislovodsk Prokhladnyï Te TERRITOIRE DE Mozdok re Karatchaïevsk Baksan Kizliar k KRASNODAR RÉP. DES L'Abkhazie et l'Ossétie du Sud sont deux Sotchi KABARDINO- Terek KARATCHAÏS-TCHERKESSES BALKARIE provinces sécessionnistes de la Géorgie. Teberda R U S S I E Le Haut-Karabagh est une province Gagra Elbrous Grozny sécessionniste de l'Azerbaïdjan. 5642 T Naltchik Nazran Goudermes ABKHAZIE C yrnyaouz Khassaviourt Kardjine Argoun Goudaouta A Beslan - Kiziliourt 5204 INGOUCHIE Ourous Mestia OSSÉTIE DU Martan Makhatchkala uri Soukhoumi T go U Alaguir Vladikavkaz Kaspiïsk kvartcheli n NORD I TCHÉTCHÉNIE Bouïnaksk Otchamtchire C Kazbek Atchissou Oni 5037 Izberbach Zougdidi A 4492 DAGUESTAN Ossétie M E R M E R Tskhaltoubo Satchkhere du Sud Koutaïssi Tskhinvali Poti Senaki Tchiatoura S Zestafoni Samtredia Tianeti Daguestanskiïe Derbent N O I R E G É O R G I E Bejta Ogni Kaspi 4127 Ozourgueti Khachouri Telavi Kvareli E C A S P I E N N E Kobouleti Borjomi Gori Mtskheta ADJARIE B TBILISSI Gourodjaani Batoumi akouriani Zaqatala r mou Akhaltsikhe Roustavi Tchnori Sa Xaçmaz Hopa Bolnissi Akhalkalaki Qax Marneouli Dedoplis-Tskaro Quba e K I e o e Ardesen ou ri 4466 Kura ra S ki D v ci Trabzon Rize Pazar Artvin Ardahan (K Bazardüzü Alaverdi ü ee Çayeli Tachir Qazax r) Siy z n Tovuz Réservoir de Sürmene 3932 Lac de Ming e çevir Çildir Spitak Idjevan Minguetchaouri e Vanadzor e Gandja (Ming çevir) -

Republic of Azerbaijan Ministry of Transport Road Transport Services Department
Supplementary Appendix C Republic of Azerbaijan Ministry of Transport Road Transport Services Department EAST–WEST HIGHWAY IMPROVEMENT PROJECT RESETTLEMENT PLAN June 2005 THIS IS NOT AN ADB BOARD APPROVED DOCUMENT To: Head of the Road Maintenance Agency of Gornboy/Yevlax/Ganja/Xanlar The draft Resettlement Plan for the Rehabilitation of the East-West Corridor Road of the Azerbaijan Republic has been prepared by the Road Transport Service Department in accordance with the Azerbaijan law and ADB guidelines on resettlement. The Resettlement Plan covers land acquisition and other resettlement aspects for the rehabilitation of the road segments from Yevlax to Ganja and from Gazax to the border with Georgia. The draft Resettlement Plan is based on the studies of social and economic conditions of businesses, ordinary people and families that have been affected by the above mentioned road rehabilitation project as well as on the consultations with local authorities. The impact shown in the Resettlement Plan reflects the results of the Technical Assistance provided by the ADB. The draft Resettlement Plan will be upgraded and completely finalized in 2006 . This draft Resettlement Plan has been approved by RTSD and ADB and may be disclosed to all affected communities and people. We authorize your agency to disclose the Resettlement Plan to all concerned parties as necessary. Attachment: draft resettlement Plan – 54 pages Head of the Road Maintenance Division V. Hajiyev CONTENTS 1. BACKGROUND 1.1. Outline of the Project 1.2 Status of the Road Reserve 2. SOCIOECONOMIC CONDITIONS IN THE PROJECT AREA 2.1 Project Impact Areas 2.2 Social Profile of the Project Areas 3. -

Nagorno-Karabakh Conflict
FT SPECIAL REPORT Azerbaijan Thursday March 12 2015 www.ft.com/reports | @ftreports Roman times. It did not stop Azerbaijan from hosting the 2012 Eurovision Song Inside Contest, and in June it hosts the inaugu- ral European Games, the biggest inter- Reform offers nationalsportseventeverstagedthere. Nagorno-Karabakh The games will take place against a conflict backdrop of troubling geopolitical and Important oil and gas economic developments for the young pipelines run close to state. The Ukrainian uprising that top- the front line the best hope pled President Viktor Yanukovich in February 2014 disturbed President Page 2 Ilham Aliyev of Azerbaijan. Not only was it a popular revolution against an authoritarian ruler, but the US and its Economy under for national western allies, regarded as partners in pressure Baku,openlysympathisedwiththepro- Devaluation and job democracyforcesonthestreetsofKiev. losses as oil price In what looked like an effort to forestall similar events at home, the slide hits hard stability Azerbaijani authorities began to crack Page 3 Foreign policy focuses on independence A long stretch of low Delicate balancing act Oil has given this former Soviet state great wealth oil prices would test the amid regional and but it still struggles on many fronts, says Tony Barber country’s economic model global powers Page 3 aterfront skyscrapers an experience it has no desire to repeat. downonpoliticaldissentandindepend- and blustery winds Azerbaijanstandsatacrossroadsofcivi- ent media even more than in the first Baku seeks a fresh role from the Caspian Sea lisations and markets, old and new, and decade under Mr Aliyev, who replaced in energy markets make Baku, Azerbai- derives its identity from multiple HeydarAliyev,hisfather,aspresidentin Plans are in train to W jan’s capital, look and sources. -

HIST WOR Photo TORIC CENT RLD HERITA O 1-1. Histor RE of SHEK
Photo 1-1. Historic centre of Sheki HISTORIC CENTRE OF SHEKI WITH THE KHAN’S PALACE WORLD HERITAGE NOMINATION FILE 1 TABLE OF CONTENTS Executive Summary_____________________________________ 5 1. Identification of the Property ____________________________ 14 1.a Country____________________________________________ 15 1.b State, Province or Region______________________________ 16 1.c Name of Property___________________________________ 18 1.d Geographical coordinates to the nearest second____________ 19 1.e Maps and plans, showing the boundaries of the nominated property and buffer zone_____________________ 19 1.f Area of nominated property and proposed buffer zone________ 21 2. Description____________________________________________ 22 2.a Description of Property________________________________ 23 2.b History and Development ______________________________ 53 3. Justification for Inscription 3.1.a Brief synthesis_____________________________________ 73 3.1.b Criteria under which inscription is proposed______________ 74 3.1.c Statement of Integrity_________________________________ 82 3.1.d Statement of Authenticity______________________________ 85 3.1.e Protection and management requirements__________________ 93 3.2 Comparative Analysis__________________________________ 95 3.3 Proposed Statement of Outstanding Universal Value___________ 110 4. State of conservation and factors affecting the Property_______ 113 4a Present state of conservation_____________________________ 114 4b Factors affecting the property____________________________ 123 -

Democracy and Minority Rights in Azerbaijan in Light of the 2013 Presidential Elections Report on Fact-Finding Mission to Dagestan and Azerbaijan September 2013
UNPO Democracy and Minority Rights in Azerbaijan in light of the 2013 presidential elections Report on Fact-Finding Mission to Dagestan and Azerbaijan September 2013 1 Summary After the collapse of the Soviet Union, and in the wake of the Chechen war, the border between Azerbaijan and Russia was closed. The Lezghin people, an ethnic group indigenous to the Caucasus, found itself split between two states. The fact-finding mission to Dagestan and Azerbaijan aimed at examining the situation of the Lezghin, and other ethnic and religious groups, in light of the Azeri Presidential elections of 9 October 2013. Political Representation, Socio-Economic Conditions and Culture and Language were the three key thematics on which the mission gathered data and testimonies. Due to the political make-up and geographical location of the Republic of Dagestan, the distribution of wealth and resources doesn’t target the Lezghin as major beneficiaries. Even though 14 nationalities are officially represented and protected, the lack of official quota for public offices, and unwritten rules about ethnic representation, constitute a threat to the political representation of the Lezghin. Protection and support to native languages is provided by local administrations, and attempts are made to reinvigorate the use of local languages. The dominance of Russian in administration does pose a threat to the indigenous languages. 2 Artistic expression typical for ethnic traditions are encouraged and aim at connecting different ethnic and 3 religious groups. The fate of evicted villagers of former Russian exclaves in Azerbaijan, such as the village of Hrah-Uba, remains worrying. Examining the same thematics and the same ethnic group right across the border in Azerbaijan raised major concerns. -

10 3 243 260 Logunov Guseinov.Pm6
Arthropoda Selecta 10 (3): 243260 © ARTHROPODA SELECTA, 2001 Faunistic review of the jumping spiders of Azerbaijan (Aranei: Salticidae), with additional faunistic records from neighbouring Caucasian countries Ôàóíèñòè÷åñêèé îáçîð ïàóêîâ-ñêàêóí÷èêîâ Àçåðáàéäæàíà (Aranei: Salticidae), ñ äîïîëíèòåëüíûìè ôàóíèñòè÷åñêèìè íàõîäêàìè èç ïðèëåãàþùèõ êàâêàçñêèõ ñòðàí D.V. Logunov* & E.F. Guseinov** Ä.Â. Ëîãóíîâ* & Ý.Ô. Ãóñåéíîâ** * The Manchester Museum, The University of Manchester, Oxford Road, Manchester M13 9PL, UK. ** Institute of Zoology, Kvartal 504, proezd 1128, Baku 370073, Azerbaijan. ** Èíñòèòóò Çîîëîãèè, êâàðòàë 504, ïðîåçä 1128, Áàêó 370073, Àçåðáàéäæàí. KEY WORDS: Salticidae, Azerbaijan, annotated checklist, new species, Neaetha. ÊËÞ×ÅÂÛÅ ÑËÎÂÀ: Salticidae, Àçåðáàéäæàí, àííîòèðîâàííûé ñïèñîê, íîâûé âèä, Neaetha. ABSTRACT: This paper presents an annotated haemorrhoicus from Lenkoran) and Wierzbicki [1902; checklist of the Salticidae of Azerbaijan which includes Evarcha arcuata from Gusar]. The only further record 82 species in 35 genera. Eight species are reported for was of Bianor aurocinctus (apparently Sibianor the Azerbaijanian fauna for the first time and twenty-five turkestanicus; see below) reported by Charitonov [1932] previously recorded species are excluded from the list. from Gyandja. The above three species were the only A new species, Neaetha absheronica sp.n. (#), from the recorded salticids from Azerbaijan until Dunins exten- Absheron Peninsula is described. Three species of Ylle- sive faunistic works [Dunin, 1979, 1984, 1989; Dunin & nus, and a single species of Euophrys and Phlegra Mamedov, 1992], with a few further additions by Neni- remain unidentified. Additional new records from the nin [1985]. According to these and also recent data of the neighbouring Caucasian countries, Georgia, Armenia present authors [Guseinov, 1999; Logunov, 1995, 1998, and Russia, are presented for twenty-five species. -

Turkic Toponyms of Eurasia BUDAG BUDAGOV
BUDAG BUDAGOV Turkic Toponyms of Eurasia BUDAG BUDAGOV Turkic Toponyms of Eurasia © “Elm” Publishing House, 1997 Sponsored by VELIYEV RUSTAM SALEH oglu T ranslated by ZAHID MAHAMMAD oglu AHMADOV Edited by FARHAD MAHAMMAD oglu MUSTAFAYEV Budagov B.A. Turkic Toponyms of Eurasia. - Baku “Elm”, 1997, -1 7 4 p. ISBN 5-8066-0757-7 The geographical toponyms preserved in the immense territories of Turkic nations are considered in this work. The author speaks about the parallels, twins of Azerbaijani toponyms distributed in Uzbekistan, Kazakhstan, Turkmenistan, Altay, the Ural, Western Si beria, Armenia, Iran, Turkey, the Crimea, Chinese Turkistan, etc. Be sides, the geographical names concerned to other Turkic language nations are elucidated in this book. 4602000000-533 В ------------------------- 655(07)-97 © “Elm” Publishing House, 1997 A NOTED SCIENTIST Budag Abdulali oglu Budagov was bom in 1928 at the village o f Chobankere, Zangibasar district (now Masis), Armenia. He graduated from the Yerevan Pedagogical School in 1947, the Azerbaijan State Pedagogical Institute (Baku) in 1951. In 1955 he was awarded his candidate and in 1967 doctor’s degree. In 1976 he was elected the corresponding-member and in 1989 full-member o f the Azerbaijan Academy o f Sciences. Budag Abdulali oglu is the author o f more than 500 scientific articles and 30 books. Researches on a number o f problems o f the geographical science such as geomorphology, toponymies, history o f geography, school geography, conservation o f nature, ecology have been carried out by academician B.A.Budagov. He makes a valuable contribution for popularization o f science.