Stop Look Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sexual Health Introduction This Constitutes the Full Section on Sexual Health for the Adults’ JSNA 2016
For feedback, please contact [email protected] Last updated 4-Apr-16 Review date 30-Apr-17 Sexual Health Introduction This constitutes the full section on Sexual Health for the Adults’ JSNA 2016. ‘Sexual health is a state of physical, mental and social well-being in relation to sexuality. It requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence.’1 Who’s at risk and why? According to the National Survey of Sexual Attitudes and Lifestyles Surveys (Natsal)2,3 sexual health behaviour of the population of England has changed since the survey was first undertaken in 1991. The 2011 Natsal survey demonstrated an increase in the: number of sexual partners over a person’s lifetime, particularly for women, where this has increased from 3.7 (1991) to 7.7 (2011) sexual repertoire of heterosexual partners, particularly with oral and anal sexual intercourse All sexually active individuals of all ages are at risk of sexually transmitted infections (STIs), including HIV, and unplanned pregnancies (in the fertile years). However, the risks are not equally distributed amongst the population, with certain groups being at greater risk. Poor sexual health may also be associated with other poor health outcomes. Those at highest risk of poor sexual health are often from specific population groups, with varying needs which include: Men who have sex with men (MSM) Young people who are more likely to become re-infected with STIs Some black and ethnic minority groups Sex workers Victims of sexual and domestic abuse Other marginalised or vulnerable groups, including prisoners Nationally, there is a correlation between STIs and deprivation. -

Neighbourhoods in England Rated E for Green Space, Friends of The
Neighbourhoods in England rated E for Green Space, Friends of the Earth, September 2020 Neighbourhood_Name Local_authority Marsh Barn & Widewater Adur Wick & Toddington Arun Littlehampton West and River Arun Bognor Regis Central Arun Kirkby Central Ashfield Washford & Stanhope Ashford Becontree Heath Barking and Dagenham Becontree West Barking and Dagenham Barking Central Barking and Dagenham Goresbrook & Scrattons Farm Barking and Dagenham Creekmouth & Barking Riverside Barking and Dagenham Gascoigne Estate & Roding Riverside Barking and Dagenham Becontree North Barking and Dagenham New Barnet West Barnet Woodside Park Barnet Edgware Central Barnet North Finchley Barnet Colney Hatch Barnet Grahame Park Barnet East Finchley Barnet Colindale Barnet Hendon Central Barnet Golders Green North Barnet Brent Cross & Staples Corner Barnet Cudworth Village Barnsley Abbotsmead & Salthouse Barrow-in-Furness Barrow Central Barrow-in-Furness Basildon Central & Pipps Hill Basildon Laindon Central Basildon Eversley Basildon Barstable Basildon Popley Basingstoke and Deane Winklebury & Rooksdown Basingstoke and Deane Oldfield Park West Bath and North East Somerset Odd Down Bath and North East Somerset Harpur Bedford Castle & Kingsway Bedford Queens Park Bedford Kempston West & South Bedford South Thamesmead Bexley Belvedere & Lessness Heath Bexley Erith East Bexley Lesnes Abbey Bexley Slade Green & Crayford Marshes Bexley Lesney Farm & Colyers East Bexley Old Oscott Birmingham Perry Beeches East Birmingham Castle Vale Birmingham Birchfield East Birmingham -
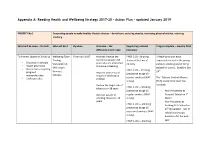
Appendix A: Reading Health and Wellbeing Strategy 2017-20 - Action Plan - Updated January 2019
Appendix A: Reading Health and Wellbeing Strategy 2017-20 - Action Plan - updated January 2019 PRIORITY No 1 Supporting people to make healthy lifestyle choices – dental care, reducing obesity, increasing physical activity, reducing smoking What will be done – the task Who will do it By when Outcome – the Supporting national Progress Update – January 2019 difference it will make indicators To Prevent Uptake of Smoking Wellbeing Team; From April 2017 Maintain/reduce the PHOF 2.03 - Smoking 3 Reading schools have Trading number of people >18 status at the time of expressed interest in the young - Education in schools Standards; CS; years who are estimated delivery person’s smoking and drinking - Health promotion to smoke in Reading S4H; Youth attitudinal survey. Deadline Dec - Quit services targeting PHOF 2.09i – Smoking th pregnant Services; 14 . Improve awareness of prevalence at age 15- women/families Schools; impact of smoking on current smokers (WAY The Tobacco Control Alliance - Underage sales children survey) [TCA] Coordinator work has Reduce the illegal sale of involved: PHOF 2.09ii – Smoking tobacco to >18 years prevalence at age 15 – - Year 9 Assembly at st Increase uptake of regular smokers (WAY Prospect School on 1 smoking cessation >18 survey) March. years - Year 9 students at PHOF 2.09iii – Smoking Reading Girls School on prevalence at age 15 – 27th November – rest of occasional smokers (WAY school year groups survey) booked in for the next PHOF 2.09iv – Smoking year prevalence at age 15 – - Year 7 students about regular smokers (SDD smoking health harms at survey) The Wren School on 7th November. Rest of PHOF 2.09v – Smoking school booked in for prevalence at age 15 – next year. -

Initial Proposals for New Parliamentary Constituency Boundaries in the South East Region Contents
Initial proposals for new Parliamentary constituency boundaries in the South East region Contents Summary 3 1 What is the Boundary Commission for England? 5 2 Background to the 2018 Review 7 3 Initial proposals for the South East region 11 Initial proposals for the Berkshire sub-region 12 Initial proposals for the Brighton and Hove, East Sussex, 13 Kent, and Medway sub-region Initial proposals for the West Sussex sub-region 16 Initial proposals for the Buckinghamshire 17 and Milton Keynes sub-region Initial proposals for the Hampshire, Portsmouth 18 and Southampton sub-region Initial proposals for the Isle of Wight sub-region 20 Initial proposals for the Oxfordshire sub-region 20 Initial proposals for the Surrey sub-region 21 4 How to have your say 23 Annex A: Initial proposals for constituencies, 27 including wards and electorates Glossary 53 Initial proposals for new Parliamentary constituency boundaries in the South East region 1 Summary Who we are and what we do Our proposals leave 15 of the 84 existing constituencies unchanged. We propose The Boundary Commission for England only minor changes to a further 47 is an independent and impartial constituencies, with two wards or fewer non -departmental public body which is altered from the existing constituencies. responsible for reviewing Parliamentary constituency boundaries in England. The rules that we work to state that we must allocate two constituencies to the Isle The 2018 Review of Wight. Neither of these constituencies is required to have an electorate that is within We have the task of periodically reviewing the requirements on electoral size set out the boundaries of all the Parliamentary in the rules. -

11K Donation from the DPS to Help LGBT Young People in Brighton and Hove Find a Home Through YMCA Downslink Group - Youth Advice Centre
Computershare Investor Services PLC The Pavilions Bridgwater Road Bristol BS99 6ZZ Telephone + 44 (0) 870 702 0000 Facsimile + 44 (0) 870 703 6101 www.computershare.com News Release Monday 27 February 2017 Date: Subject: £11k donation from The DPS to help LGBT young people in Brighton and Hove find a home through YMCA DownsLink Group - Youth Advice Centre Bristol, Monday 27 February 2017 – An £11,000 donation by The Deposit Protection Service (The DPS) will fund specialist support from YMCA DownsLink Group - Youth Advice Centre for LGBT young people in Brighton and Hove to help them find a home, the UK’s largest protector of tenancy deposits has announced. The Centre will train volunteers one-to-one to become ‘peer mentors’ and provide support to other members of the local LGBT community. Daren King, Head of Tenancy Deposit Protection at The DPS, said: “83,000 young people experience homelessness every year and the South East has the second highest rate of homeless applications in England. “As a result, we’re delighted to be supporting YMCA DownsLink Group - Youth Advice Centre’s fantastic work in helping LGBT young people in Brighton and Hove find a home.” YMCA DownsLink Group - Youth Advice Centre is a “one-stop shop” for advice and information for young people aged 13-25 years old in the City of Brighton and Hove. Julia Harrison, Advice Services Manager at YMCA DownsLink Group - Youth Advice Centre, said: “LGBT young people account for 13% of the total number of clients accessing our housing service, with a 50% increase in transgender clients since April 2016. -

50 Bus Time Schedule & Line Route
50 bus time schedule & line map 50 Brighton - Hollingdean View In Website Mode The 50 bus line (Brighton - Hollingdean) has 2 routes. For regular weekdays, their operation hours are: (1) Brighton: 5:44 AM - 11:39 PM (2) Brighton: 12:09 AM - 11:54 PM Use the Moovit App to ƒnd the closest 50 bus station near you and ƒnd out when is the next 50 bus arriving. Direction: Brighton 50 bus Time Schedule 28 stops Brighton Route Timetable: VIEW LINE SCHEDULE Sunday 7:24 AM - 11:10 PM Monday 5:44 AM - 11:39 PM Lewes Road Bus Garage, Brighton Tuesday 5:44 AM - 11:39 PM Sainsbury'S, Brighton Lewes Road, Brighton and Hove Wednesday 5:44 AM - 11:39 PM Bottom Of Davey Drive, Brighton Thursday 5:44 AM - 11:39 PM Friday 5:44 AM - 11:39 PM Waverley Crescent, Brighton Saturday 5:53 AM - 11:39 PM St Joseph's School, Brighton Tavistock Down, Brighton Mountƒelds, Brighton 50 bus Info Direction: Brighton Lynchet Close, Brighton Stops: 28 Trip Duration: 32 min Brentwood Crescent, Brighton Line Summary: Lewes Road Bus Garage, Brighton, Sainsbury'S, Brighton, Bottom Of Davey Drive, Hollingbury Rise, Brighton and Hove Brighton, Waverley Crescent, Brighton, St Joseph's School, Brighton, Tavistock Down, Brighton, Burstead Close, Brighton Mountƒelds, Brighton, Lynchet Close, Brighton, Brentwood Crescent, Brighton, Burstead Close, Quarry Bank Road, Brighton Brighton, Quarry Bank Road, Brighton, Hollingbury Stanmer Villas, Brighton and Hove Crescent, Brighton, The Dip, Brighton, Hollingdean Street, Brighton, Bottom Of Roedale Road, Brighton, Hollingbury Crescent, Brighton -
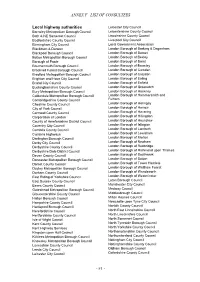
Annex F –List of Consultees
ANNEX F –LIST OF CONSULTEES Local highway authorities Leicester City Council Barnsley Metropolitan Borough Council Leicestershire County Council Bath & NE Somerset Council Lincolnshire County Council Bedfordshire County Council Liverpool City Council Birmingham City Council Local Government Association Blackburn & Darwen London Borough of Barking & Dagenham Blackpool Borough Council London Borough of Barnet Bolton Metropolitan Borough Council London Borough of Bexley Borough of Poole London Borough of Brent Bournemouth Borough Council London Borough of Bromley Bracknell Forest Borough Council London Borough of Camden Bradford Metropolitan Borough Council London Borough of Croydon Brighton and Hove City Council London Borough of Ealing Bristol City Council London Borough of Enfield Buckinghamshire County Council London Borough of Greenwich Bury Metropolitan Borough Council London Borough of Hackney Calderdale Metropolitan Borough Council London Borough of Hammersmith and Cambridgeshire County Council Fulham Cheshire County Council London Borough of Haringey City of York Council London Borough of Harrow Cornwall County Council London Borough of Havering Corporation of London London Borough of Hillingdon County of Herefordshire District Council London Borough of Hounslow Coventry City Council London Borough of Islington Cumbria County Council London Borough of Lambeth Cumbria Highways London Borough of Lewisham Darlington Borough Council London Borough of Merton Derby City Council London Borough of Newham Derbyshire County Council London -

{Download PDF} Portsmouth Pubs Ebook Free Download
PORTSMOUTH PUBS PDF, EPUB, EBOOK Steve Wallis | 96 pages | 15 Feb 2017 | Amberley Publishing | 9781445659893 | English | Chalford, United Kingdom Portsmouth Pubs PDF Book Bristol, 10 pubs per square mile 4. Purnell Farm was then later renamed Middle Farm by the Goldsmith's. Third place is a tie between Bristol, Brighton and Hove, and Norwich, with all three spots having 10 pubs per square mile. St James' Hospital , an institution for the treatment of mental health, first opened in on what was then called Asylum Road, now named Locksway Road. More top stories. From Business: It's more than beer for us; MoMac is a place for the whole neighborhood to have fun. When looking at the UK as a whole, Portsmouth came out on top with almost double the number of pubs per square mile than London overall though many of the capital's boroughs soar far above Portsmouth's total. But it is Brighton and Hove that has the most pubs per people out of all three. Sarah Dinenage Con [9]. But researchers point out that the area is almost 12, square miles in size. Add your own AMAZing articles. Parking Available. Mostly consisting of makeshift houseboats, converted railway carriages and fisherman huts, many of these homes, lacking the basic amenities of electricity and plumbed water supplies, survived into the s until they were cleared. The land is still settling and the cavities of Milton Common make ideal homes for foxes and other wildlife. Trafalgar Arms 11 reviews. Stellar Wine Co. The taste is totally different from what I had and I was a frequent customer for the last years!!! The start of the week is your cue for free pool — you can take to the table free of charge all day on a Monday. -

Appendix 6 Performance Indicator and CIPFA Data Comparisons BVPI Comparisons
Appendix 6 Performance Indicator and CIPFA Data Comparisons BVPI Comparisons Southend-on-Sea vs CPA Environment High Scorers / Nearest Neighbours / Unitaries BV 106: Percentage of new homes built on previously developed land 2001/02 2002/03 2003/04 Southend-on-Sea 100 100 100 CPA 2002 Environment score 3 or 4 in unitary authorities, by indicator 2001/02 2002/03 2003/04 Blackpool 56.8 63 n/a Bournemouth 94 99 n/a Derby 51 63 n/a East Riding of Yorkshire 24.08 16.64 n/a Halton 27.48 49 n/a Hartlepool 40.8 56 n/a Isle of Wight 84 86 n/a Kingston-upon-Hull 40 36 n/a Luton 99 99.01 n/a Middlesbrough 74.3 61 n/a Nottingham 97 99 n/a Peterborough 79.24 93.66 n/a Plymouth 81.3 94.4 n/a South Gloucestershire 41 44.6 n/a Stockton-on-Tees 33 29.34 n/a Stoke-on-Trent 58.4 61 n/a Telford & Wrekin 54 55.35 n/a Torbay 39 58.57 n/a CIPFA 'Nearest Neighbour' Benchmark Group 2001/02 2002/03 2003/04 Blackpool 56.8 63 n/a Bournemouth 94 99 n/a Brighton & Hove 99.7 100 n/a Isle of Wight 84 86 n/a Portsmouth 98.6 100 n/a Torbay 39 58.57 n/a Unitaries 2001/02 2002/03 2003/04 Unitary 75th percentile 94 93.7 n/a Unitary Median 70 65 n/a Unitary 25th percentile 41 52.3 n/a Average 66.3 68.7 n/a Source: ODPM website BV 107: Planning cost per head of population. -

Studentified Areas As Contested Heterotopias : Findings from Southampton
CORE Metadata, citation and similar papers at core.ac.uk Provided by White Rose Research Online This is a repository copy of Studentified areas as contested heterotopias : Findings from Southampton. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/130755/ Version: Published Version Article: Brookfield, Katherine (2018) Studentified areas as contested heterotopias : Findings from Southampton. Area. pp. 1-10. ISSN 0004-0894 https://doi.org/10.1111/area.12458 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Accepted: 26 March 2018 DOI: 10.1111/area.12458 REGULAR PAPER Studentified areas as contested heterotopias: Findings from Southampton Katherine Brookfield Environment Department, University of The ongoing “massification” of higher education in the UK has generated York, York, UK increased demand for student housing. Some of this demand is being met by new, Correspondence purpose-built student accommodation, but much is being met through an intensifi- Katherine Brookfield “ ” Email: [email protected] cation of student properties in established student areas , and the expansion of student housing into neighbourhoods previously unaffected by high levels of stu- Funding information dent in-migration in a process termed “studentification”. -

A Fairer Southampton
A Fairer Southampton A Fairer Southampton Southampton Fairness Commission Final Report: December 2015 1 A Fairer Southampton Contents 1. Acknowledgements 2. Foreword from the Chair 3. Our vision and principles 4. Executive summary and recommendations 5. The Southampton Fairness Commission 6. Why fairness is important for everyone 7. The Southampton picture – not such a fair deal for everyone 8. Consultation, participation and engagement 9. The Commission’s recommendations: Fairer employment Fairer living Fairer organisations Fairer communities 10. A fairness index for the city 11. Next steps Appendix 1: Speakers and facilitators 2 A Fairer Southampton 1. Acknowledgements The Southampton Fairness Commission would like to thank: The countless individuals, groups, organisations who invested their time and energy in contributing to the Commission’s work – there are too many to name individually Those who shared their knowledge and expertise Those who gave us their personal testimonials and life experiences Those who shared their enthusiasm , innovation and ideas Speakers who gave formal presentations at the themed meetings. Other Fairness Commissions that have inspired us. We would also like to thank people who spoke and gave their support at the initial launch of the Southampton Fairness Commission - Lela Kogbara (Islington Council) John Denham (MP for Southampton Itchen until May 2015) and Paula Claisse from KPMG. We would particularly like to thank Councillor Andy Hull (Islington Council) for sharing learning and experience of the first ever Fairness Commission with us. Find out more about the Southampton Fairness Commission by visiting our website: www.southamptonfairnesscommission.org 3 A Fairer Southampton 2. Foreword from the Chair Like everyone else, I want a good life for myself, my family, and my friends. -

BHCC Local Flood Risk Management Strategy
Brighton & Hove City Council BHCC Local Flood Risk Management Strategy Project Ref: 23301/2001 | Rev: 3 | Date: February 2015 Office Address: Caversham Bridge House, Waterman Place, Reading, Berkshire RG1 8DN T: +44 (0)118 950 0761 F: +44 (0)118 959 7498 E: [email protected] Local Flood Risk Management Strategy Brighton and Hove City Council Document Control Sheet Project Name: Brighton and Hove City Council - LFRMS Project Ref: 23301/2001 Report Title: Local Flood Risk Management Strategy Doc Ref: R001 Date: November 2014 Name Position Signature Date Prepared by: Vicky Hogg Senior Engineer VH 21/11/14 Reviewed by: Mark Lennon Senior Engineer ML 21/11/14 Approved by: Daniel Hayes Director 21/11/14 For and on behalf of Peter Brett Associates LLP Revision Date Description Prepared Reviewed Approved 0 21/11/14 Draft VH ML DTH 1 24/11/14 2nd Draft with Appendices VH ML DTH 2 12/12/14 RMA consultation VH ML DTH 3 13/02/15 For Public Consultation ML DTH DTH 4. 16/06/15 Final DTH DTH DTH Peter Brett Associates LLP disclaims any responsibility to the Client and others in respect of any matters outside the scope of this report. This report has been prepared with reasonable skill, care and diligence within the terms of the Contract with the Client and generally in accordance with the appropriate ACE Agreement and taking account of the manpower, resources, investigations and testing devoted to it by agreement with the Client. This report is confidential to the Client and Peter Brett Associates LLP accepts no responsibility of whatsoever nature to third parties to whom this report or any part thereof is made known.