Autonomic Nerve Preservation During Rectal Cancer Resection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Autonomic Nerve Activity and Cardiac Arrhythmias
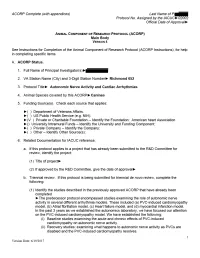
ACORP Complete (with appendices) Last Name of PI► Protocol No. Assigned by the IACUC►02002 Official Date of Approval► 1. Caging needs. Complete the table below to describe the housing that will have to be accommodated by the housing sites for this protocol: d. Is this housing e. Estimated c. Number of consistent with the maximum number a. Species b. Type of housing* individuals per Guide and USDA of housing units housing unit** regulations? needed at any one (yes/no***) time Chain link run, 3x6 Canines 1 no 7 and 4x10 feet cage *See ACORP Instructions, for guidance on describing the type of housing needed. If animals are to be housed according to a local Standard Operating Procedure (SOP), enter “standard (see SOP)” here, and enter the SOP into the table in Item Y. If the local standard housing is not described in a SOP, enter “standard, see below” in the table and describe the standard housing here: Chain link run, 3x6 feet cages ** The Guide states that social animals should generally be housed in stable pairs or groups. Provide a justification if any animals will be housed singly (if species is not considered “social”, then so note) Dogs are housed singly in chain link runs but can socialize with one another since each room has two to five dog runs. In addition, while their runs are being cleaned on a daily basis, pairs of dogs are allowed to exercise and play together in a designated "romper room". Animals are fitted with DSI transmitters and need to be housed singly in a cage for which DSI receivers are installed to receive signals from the transmitters. -

Dear Subscribers! This Issue of Our Magazine Is Devoted to Cooperation of Our Editorial Board with Ukrainian Medical Scientists
Deutscher Wissenschaftsherold • German Science Herald, N 4/2016 Dear subscribers! This issue of our magazine is devoted to cooperation of our editorial board with Ukrainian medical scientists. We present you the results of their researches. UDC: 611.831.1:611.216-018.73 Boichuk O.M. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, M.H. Turkevych Department of Human Anatomy, Chernivtsi, Ukraine, [email protected] Kryvetska I.I. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, S.M. Savenko Department of Neurology, Psychiatry and Medical Psychology Chernivtsi, Ukraine Bambuliak A.V. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, Department of Surgical and Pediatric Dentistry, Chernivtsi, Ukraine, [email protected] Sapunkov O.D. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, Department of Pediatric Surgery and Otolaryngology, Chernivtsi, Ukraine STRUCTURAL COMPONENTS OF AUTONOMIC INNERVATION OF MUCOSA OF NASAL CAVITY AND PARANASAL SINUSES Abstract. Autonomic innervation of mucosa of the nasal cavity and paranasal sinuses has been studied using complex morphological methods. It was determined that autonomic innervation of the nasal cavity and paranasal sinuses mostly occurs due to the branches of the pterygopalatine ganglion Keywords: nasal cavity, paranasal sinuses, innervation, pterygopalatine ganglion, mucosa, anatomy. Introduction. Mucosa of nasal cavity is peripheral element of olfactory analyzer functionally large receptor surface with a very consists of highly specialized epithelium of the complex and various reflex connections. It is upper nasal passage, short dendrites, which equipped with lots of blood and lymphatic ends with receptors, and axons form olfactory vessels, which are surrounded with numerous filaments that enter the olfactory bulb where nerve endings. -

The Sacral Autonomic Outflow Is Sympathetic
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UCL Discovery The sacral autonomic outflow is sympathetic Isabel Espinosa-Medina1,†, Orthis Saha1,†, Franck Boismoreau1, Zoubida Chettouh1, Francesca Rossi1, William D. Richardson2 and Jean-François Brunet1* 1 Institut de Biologie de l’ENS (IBENS), INSERM, CNRS, École Normale Supérieure, PSL Research University, Paris, 75005 France. 2 Wolfson Institute for Biomedical Research, University College London, London UK. †These authors contributed equally to this work *Correspondence to [email protected] 1 Abstract In the autonomic nervous system of mammals and birds, sacral preganglionic neurons are considered parasympathetic, as are their targets in the pelvic ganglia that prominently control rectal, bladder and genital functions. The allocation of the sacral autonomic outflow to the parasympathetic nervous system —i.e. as the second tier of a “cranio-sacral outflow”— has an ancient history: rooted in the work of Gaskell 1, formalized by Langley2 and universally accepted ever since (e.g. 3). The rationale lied in several perceived similarities between the sacral and cranial outflows: anatomical —separation from the thoracolumbar, sympathetic outflow by a gap at limb levels 1, a target territory less diffuse than that of the latter and a lack of projections to the paravertebral sympathetic chain 1; physiological —an influence on some organs opposite to that of the thoracolumbar outflow 4; and pharmacological — an overall sensitivity to muscarinic antagonists2. However, cell-phenotypic criteria have been lacking and were never sought. Here we uncover fifteen phenotypic and ontogenetic features that distinguish pre- and postganglionic neurons of the cranial parasympathetic outflow from those of the thoracolumbar sympathetic outflow. -

Sympathetic Tales: Subdivisons of the Autonomic Nervous System and the Impact of Developmental Studies Uwe Ernsberger* and Hermann Rohrer
Ernsberger and Rohrer Neural Development (2018) 13:20 https://doi.org/10.1186/s13064-018-0117-6 REVIEW Open Access Sympathetic tales: subdivisons of the autonomic nervous system and the impact of developmental studies Uwe Ernsberger* and Hermann Rohrer Abstract Remarkable progress in a range of biomedical disciplines has promoted the understanding of the cellular components of the autonomic nervous system and their differentiation during development to a critical level. Characterization of the gene expression fingerprints of individual neurons and identification of the key regulators of autonomic neuron differentiation enables us to comprehend the development of different sets of autonomic neurons. Their individual functional properties emerge as a consequence of differential gene expression initiated by the action of specific developmental regulators. In this review, we delineate the anatomical and physiological observations that led to the subdivision into sympathetic and parasympathetic domains and analyze how the recent molecular insights melt into and challenge the classical description of the autonomic nervous system. Keywords: Sympathetic, Parasympathetic, Transcription factor, Preganglionic, Postganglionic, Autonomic nervous system, Sacral, Pelvic ganglion, Heart Background interplay of nervous and hormonal control in particular The “great sympathetic”... “was the principal means of mediated by the sympathetic nervous system and the ad- bringing about the sympathies of the body”. With these renal gland in adapting the internal -

Neuropeptides and the Innervation of the Avian Lacrimal Gland
Investigative Ophthalmology & Visual Science, Vol. 30, No. 7, July 1989 Copyright © Association for Research in Vision and Ophthalmology Neuropeptides and the Innervation of the Avian Lacrimal Gland Denjomin Wolcorr,* Patrick A. 5ibony,j- and Kent T. Keyser^: The chicken Harderian gland, the major lacrimal gland, has two major cell populations: a cortical secretory epithelium and a medullary interstitial cell population of lymphoid cells. There is an exten- sive acetylcholinesterase (AChE) network throughout the gland, as well as catecholamine positive fibers among the interstitial cells. There are substance P-like (SPLI) and vasoactive intestinal poly- peptide-like (VIPLI) immunoreactivite fibers throughout the gland. These fibers are particularly dense and varicose among the interstitial cells. The adjacent pterygopalatine ganglion complex has neuronal somata that exhibit VIPLI and were AChE-positive. This ganglion complex also contains SPLI and catecholamine-positive fibers. In regions of the ganglion, the somata appear surrounded by SPLI varicosities. Surgical ablation of the ganglion eliminated or reduced the VIPLI, AChE and catecholamine staining in the gland. The SPLI was reduced only in some regions. Ablation of the superior cervical ganglion or severance of the radix autonomica resulted in the loss of catecholamine staining in the pterygopalatine ganglion and the gland. Severance of the ophthalmic or infraorbital nerves had no effect on the VIPLI or the SPLI staining pattern in the gland. Invest Ophthalmol Vis Sci 30:1666-1674, 1989 The avian Harderian gland is the major source of further investigation. Using immunohistochemical serous fluid1 and immunoglobulins2 in tears. Like the techniques and surgical ablations, the source, pat- mammalian lacrimal gland, it is innervated by both terns and regional distribution of cholinergic, adren- sympathetic and parasympathetic nerve fibers.34 The ergic and neuropeptide innervation of the chicken avian gland differs from the mammalian lacrimal Harderian gland were studied. -

Autonomic Nerve Regulation for Prostate Cancer: Study Based on the Tissue Transcriptional Analysis
6767 Original Article Autonomic nerve regulation for prostate cancer: study based on the tissue transcriptional analysis Fang Liu1#, Huan Xu2#, Junyi Chen3#, Bo Yang2, Lin Zhao2, Jin Ji2, Zhi Cao2, Ji Lyu2, Fubo Wang2 1Department of Urology, Pingxiang People’s Hospital, Pingxiang, China; 2Department of Urology, Shanghai Changhai Hospital, Second Military Medical University, Shanghai, China; 3Department of Urology, the Second Affiliated Hospital of Fujian Medical University, Quanzhou, China Contributions: (I) Conception and design: H Xu; (II) Administrative support: F Wang; (III) Provision of study materials or patients: F Liu, J Chen, J Lyu; (IV) Collection and assembly of data: B Yang; (V) Data analysis and interpretation: L Zhao, J Ji, Z Cao; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Fubo Wang. Department of Urology, Shanghai Changhai Hospital, Second Military Medical University, 168 Changhai Road, Shanghai, China. Email: [email protected]. Background: The whole-body energy metabolism is regulated by autonomic nerves which also play important roles in the regulation of the generation and development of different kinds of cancers. This study is to analyze the expression of autonomic nerve receptors and their relationship with the development of prostate cancer (PCa) and to further understand the central regulation of the prostate. Methods: RNA sequencing data concerning autonomic nerve receptors from paired tumor and adjacent benign tissues from 65 patients were collected. The mRNA expression and patient data were analyzed. The Cancer Genome Atlas (TCGA) data confirmed the results, and Pearson analysis, Pearson heat maps, gene heat maps, multivariate logistic regression models, receiver operating characteristic (ROC) curves and Gene Set Enrichment Analysis (GSEA) and Pearson’s analysis were analyzed for correlation analysis in this study. -

The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction
Journal of Cardiovascular Development and Disease Review The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction Laura Fedele * and Thomas Brand * Developmental Dynamics, National Heart and Lung Institute (NHLI), Imperial College, London W12 0NN, UK * Correspondence: [email protected] (L.F.); [email protected] (T.B.); Tel.: +44-(0)-207-594-6531 (L.F.); +44-(0)-207-594-8744 (T.B.) Received: 17 August 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: The cardiac autonomic nervous system (CANS) plays a key role for the regulation of cardiac activity with its dysregulation being involved in various heart diseases, such as cardiac arrhythmias. The CANS comprises the extrinsic and intrinsic innervation of the heart. The intrinsic cardiac nervous system (ICNS) includes the network of the intracardiac ganglia and interconnecting neurons. The cardiac ganglia contribute to the tight modulation of cardiac electrophysiology, working as a local hub integrating the inputs of the extrinsic innervation and the ICNS. A better understanding of the role of the ICNS for the modulation of the cardiac conduction system will be crucial for targeted therapies of various arrhythmias. We describe the embryonic development, anatomy, and physiology of the ICNS. By correlating the topography of the intracardiac neurons with what is known regarding their biophysical and neurochemical properties, we outline their physiological role in the control of pacemaker activity of the sinoatrial and atrioventricular nodes. We conclude by highlighting cardiac disorders with a putative involvement of the ICNS and outline open questions that need to be addressed in order to better understand the physiology and pathophysiology of the ICNS. -

Pattern of Autonomic Innervation
Pattern of Innervation of the Viscera The nerves supplying the viscera are derived from the autonomic nervous system – sympathetic and parasympathetic. The viscera of the thorax, abdomen and pelvis are supplied segmentally by branches of the sympathetic chain, and branches of the vagus nerve, as discussed below. The autonomic supply of structures in the head and neck follows a specific pattern that will be dealt with separately. The sympathetic chain: Communicates with the spinal nerves via white and grey rami communicantes The white rami communicantes: are present only at the levels of T1 to L2 spinal nerves convey all the sympathetic efferents from the spinal cord to the sympathetic chain consist of myelinated pre-ganglionic axons have their cell bodies in the lateral grey column of the spinal cord synapse in the sympathetic ganglia with postganglionic neurons NOTE: The cervical, lower lumbar and sacral ganglia have no white rami, and receive their sympathetic inflow from the thoracic and lumbar segments via ascending or descending axons in the sympathetic chain The grey rami communicantes consist of unmyelinated postganglionic neurons are the axons of postganglionic neurons distribute somatic branches via the cutaneous nerves to the arteries, sweat glands and arrectores pilorum in the skin, (where they are vasoconstrictor, secretomotor, and pilomotor respectively. are present in all spinal ganglia Visceral sympathetic branches are distributed to the viscera via autonomic nerve plexuses (listed in the table below) arise as -

Possible Involvement of the Autonomic Nervous System in Cervical
Matsui et al. BMC Musculoskeletal Disorders (2021) 22:419 https://doi.org/10.1186/s12891-021-04293-7 RESEARCH ARTICLE Open Access Possible involvement of the autonomic nervous system in cervical muscles of patients with myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) Takayoshi Matsui1,2, Kazuhiro Hara2, Makoto Iwata1, Shuntaro Hojo1, Nobuyuki Shitara1, Yuzo Endo1, Hideoki Fukuoka1, Masaki Matsui2 and Hiroshi Kawaguchi1* Abstract Background: Patients with myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) sometimes present with stiffness of the cervical muscles. To investigate the pathophysiology of ME/CFS, this observational study compared patients with versus without recovery from ME/CFS through local modulation of the cervical muscles. Methods: Over a period of 11 years, a total of 1226 inpatients with ME/CFS who did not respond to outpatient care were enrolled in this study. All patients received daily cervical muscle physical therapy during hospitalization. Self-rated records documenting the presence or absence of ME/CFS, as well as the representative eight symptoms that frequently accompany it at admission and discharge, were compared. Pupil diameter was also measured to examine autonomic nervous system function involvement. Results: The recovery rate of ME/CFS after local therapy was 55.5%, and did not differ significantlybysex,agestrata,and hospitalization period. The recovery rates of the eight symptoms were variable (36.6–86.9%); however, those of ME/CFS in the symptom subpopulations were similar (52.3–55.8%). The recovery rates of all symptoms showed strong associations with that of ME/CFS (p < 0.001). The pupil diameter was more constricted in the ME/CFS-recovered patients than in the ME/CFS- unrecovered patients in the total population and the subpopulations stratified by sex, age, and hospitalization period. -

Autonomic Nervous System
NERVOUS SYSTEM OUTLINE 18.1 Comparison of the Somatic and Autonomic Nervous Systems 540 18.2 Overview of the Autonomic Nervous System 542 18 18.3 Parasympathetic Division 545 18.3a Cranial Nerves 545 18.3b Sacral Spinal Nerves 545 18.3c Effects and General Functions of the Parasympathetic Division 545 Autonomic 18.4 Sympathetic Division 547 18.4a Organization and Anatomy of the Sympathetic Division 547 18.4b Sympathetic Pathways 550 Nervous 18.4c Effects and General Functions of the Sympathetic Division 550 18.5 Other Features of the Autonomic Nervous System 552 System 18.5a Autonomic Plexuses 552 18.5b Neurotransmitters and Receptors 553 18.5c Dual Innervation 554 18.5d Autonomic Reflexes 555 18.6 CNS Control of Autonomic Function 556 18.7 Development of the Autonomic Nervous System 557 MODULE 7: NERVOUS SYSTEM mck78097_ch18_539-560.indd 539 2/14/11 3:46 PM 540 Chapter Eighteen Autonomic Nervous System n a twisting downhill slope, an Olympic skier is concentrat- Recall from figure 14.2 (page 417) that the somatic nervous O ing on controlling his body to negotiate the course faster than system and the autonomic nervous system are part of both the anyone else in the world. Compared to the spectators in the viewing central nervous system and the peripheral nervous system. The areas, his pupils are more dilated, and his heart is beating faster SNS operates under our conscious control, as exemplified by vol- and pumping more blood to his skeletal muscles. At the same time, untary activities such as getting out of a chair, picking up a ball, organ system functions not needed in the race are practically shut walking outside, and throwing the ball for the dog to chase. -

Anatomy: Know Your Abdomen
Anatomy: Know Your Abdomen Glossary Abdomen - part of the body below the thorax (chest cavity); separated by the diaphragm. Anterior - towards the front of the body. For example, the umbilicus is anterior to the spine. Appendix - blind ended pouch. Autonomic nervous system – part of the nervous system responsible for functions we are not consciously aware of, such as heart rate and digestion. Aponeurosis – thin, flat fibrous sheath that replaces tendon for thin flat muscles. Bile - yellow/brown fluid produced and secreted by the liver and stored in the gallbladder. Aids digestion of lipids (fats). Conjoint tendon – the posterior wall of the inguinal canal directly behind the superficial inguinal ring formed by the union of the internal oblique and transversus abdominis muscles. CT – computerised topography. A method of using x-rays to examine the internal structures by rotating the x-ray source around the body. Dorsal – this term relates to the ‘back’ of an organism. For humans this is similar to ‘posterior’ and is used more when describing embryological development. Distal – far from the centre of the body or point of attachment. For example, the wrist is distal to the elbow. Duodenum - the first part of the small intestine. It is continuous with the stomach and jejunum (second part of the small intestine), so food will pass from stomach to duodenum to jejunum. Duodenal papillae - small round elevations in the mucosa of the second part of the duodenum. There are two duodenal papillae, major and minor. The major papilla is also known as the ‘Papilla of Vater’. The major duodenal papilla is where the ampulla of Vater (joining of pancreatic duct and common bile duct) opens into the duodenum, allowing bile and enzymes to be delivered to facilitate digestion. -

Autonomic Nervous System of the Pelvis — General Overview
FOLIA MEDICA CRACOVIENSIA Vol. LVIII, 2, 2018: 21–44 PL ISSN 0015-5616 DOI: 10.24425/fmc.2018.124656 Autonomic nervous system of the pelvis — general overview Justyna Sienkiewicz-Zawilińska1, Jarosław Zawiliński1, Lourdes Niroya Kaythampillai1, Marcin Jakiel1, Jacenty Urbaniak1, Tomasz Bereza1, Wojciech Kowalski2, Marios Loukas3, Jerzy Walocha1 1Department of Anatomy, Jagiellonian University Medical College, Kraków, Poland 2Gabinety Lekarskie Wojciech Kowalski, Kraków, Poland 3Department of Anatomy, St. George’s University, Grenada Corresponding author: Jerzy A. Walocha, MD, PhD Department of Anatomy, Jagiellonian University Medical College ul. Kopernika 12, 31-034 Kraków, Poland Phone: +48 12 422 95 11; E-mail: [email protected] Abstract: Autonomic nervous system of the pelvis is still poorly understood. Every year more and more pelvic procedures are carried out on patients suff ering from diff erent pelvic disorders what leads to numerous pelvic dysfunctions. Authors tried to review, starting from historical and clinical background, the most important reports on anatomy of the pelvic autonomic plexuses. We also pay attention to complete lack of knowledge of students of medicine on the autonomic nervous structures in the area studied. We present anatomical description of the pelvic plexuses including their visceral branches and anatomy of surrounding pelvic tissues which still remains unclear. More and more attention is paid to the topography of the plexuses specially because of new pain releasing techniques — neurolysies. Key words: autonomic nervous system, inferior hypogastric plexus, anatomy, nerve sparing, pelvis. 22 Justyna Sienkiewicz-Zawilińska, Jarosław Zawiliński, et al. Introduction Th e innervation of human pelvis was a subject of numerous studies and reports of the scientists who studied both fresh and embalmed cadavers (Hunter, Lee, Beck, Frankenhäuser, Davis, Labate, Krantz, Quinn).