The Sacral Autonomic Outflow Is Sympathetic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Autonomic Nerve Activity and Cardiac Arrhythmias
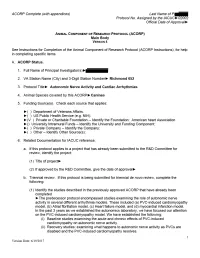
ACORP Complete (with appendices) Last Name of PI► Protocol No. Assigned by the IACUC►02002 Official Date of Approval► 1. Caging needs. Complete the table below to describe the housing that will have to be accommodated by the housing sites for this protocol: d. Is this housing e. Estimated c. Number of consistent with the maximum number a. Species b. Type of housing* individuals per Guide and USDA of housing units housing unit** regulations? needed at any one (yes/no***) time Chain link run, 3x6 Canines 1 no 7 and 4x10 feet cage *See ACORP Instructions, for guidance on describing the type of housing needed. If animals are to be housed according to a local Standard Operating Procedure (SOP), enter “standard (see SOP)” here, and enter the SOP into the table in Item Y. If the local standard housing is not described in a SOP, enter “standard, see below” in the table and describe the standard housing here: Chain link run, 3x6 feet cages ** The Guide states that social animals should generally be housed in stable pairs or groups. Provide a justification if any animals will be housed singly (if species is not considered “social”, then so note) Dogs are housed singly in chain link runs but can socialize with one another since each room has two to five dog runs. In addition, while their runs are being cleaned on a daily basis, pairs of dogs are allowed to exercise and play together in a designated "romper room". Animals are fitted with DSI transmitters and need to be housed singly in a cage for which DSI receivers are installed to receive signals from the transmitters. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

Neuronal Types and Their Specification Dynamics in the Autonomic Nervous System
From the Department of Medical Biochemistry and Biophysics Karolinska Institutet, Stockholm, Sweden NEURONAL TYPES AND THEIR SPECIFICATION DYNAMICS IN THE AUTONOMIC NERVOUS SYSTEM Alessandro Furlan Stockholm 2016 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by E-Print AB © Alessandro Furlan, 2016 ISBN 978-91-7676-419-0 On the cover: abstract illustration of sympathetic neurons extending their axons Credits: Gioele La Manno NEURONAL TYPES AND THEIR SPECIFICATION DYNAMICS IN THE AUTONOMIC NERVOUS SYSTEM THESIS FOR DOCTORAL DEGREE (Ph.D.) By Alessandro Furlan Principal Supervisor: Opponent: Prof. Patrik Ernfors Prof. Hermann Rohrer Karolinska Institutet Max Planck Institute for Brain Research Department of Medical Biochemistry and Research Group Developmental Neurobiology Biophysics Division of Molecular Neurobiology Examination Board: Prof. Jonas Muhr Co-supervisor(s): Karolinska Institutet Prof. Ola Hermansson Department of Cell and Molecular Biology Karolinska Institutet Department of Neuroscience Prof. Tomas Hökfelt Karolinska Institutet Assistant Prof. Francois Lallemend Department of Neuroscience Karolinska Institutet Division of Chemical Neurotransmission Department of Neuroscience Prof. Ted Ebedal Uppsala University Department of Neuroscience Division of Developmental Neuroscience To my parents ABSTRACT The autonomic nervous system is formed by a sympathetic and a parasympathetic division that have complementary roles in the maintenance of body homeostasis. Autonomic neurons, also known as visceral motor neurons, are tonically active and innervate virtually every organ in our body. For instance, cardiac outflow, thermoregulation and even the focusing of our eyes are just some of the plethora of physiological functions under the control of this system. Consequently, perturbation of autonomic nervous system activity can lead to a broad spectrum of disorders collectively known as dysautonomia and other diseases such as hypertension. -

Dear Subscribers! This Issue of Our Magazine Is Devoted to Cooperation of Our Editorial Board with Ukrainian Medical Scientists
Deutscher Wissenschaftsherold • German Science Herald, N 4/2016 Dear subscribers! This issue of our magazine is devoted to cooperation of our editorial board with Ukrainian medical scientists. We present you the results of their researches. UDC: 611.831.1:611.216-018.73 Boichuk O.M. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, M.H. Turkevych Department of Human Anatomy, Chernivtsi, Ukraine, [email protected] Kryvetska I.I. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, S.M. Savenko Department of Neurology, Psychiatry and Medical Psychology Chernivtsi, Ukraine Bambuliak A.V. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, Department of Surgical and Pediatric Dentistry, Chernivtsi, Ukraine, [email protected] Sapunkov O.D. Higher State Educational Institution of Ukraine “Bukovinian State Medical University”, Department of Pediatric Surgery and Otolaryngology, Chernivtsi, Ukraine STRUCTURAL COMPONENTS OF AUTONOMIC INNERVATION OF MUCOSA OF NASAL CAVITY AND PARANASAL SINUSES Abstract. Autonomic innervation of mucosa of the nasal cavity and paranasal sinuses has been studied using complex morphological methods. It was determined that autonomic innervation of the nasal cavity and paranasal sinuses mostly occurs due to the branches of the pterygopalatine ganglion Keywords: nasal cavity, paranasal sinuses, innervation, pterygopalatine ganglion, mucosa, anatomy. Introduction. Mucosa of nasal cavity is peripheral element of olfactory analyzer functionally large receptor surface with a very consists of highly specialized epithelium of the complex and various reflex connections. It is upper nasal passage, short dendrites, which equipped with lots of blood and lymphatic ends with receptors, and axons form olfactory vessels, which are surrounded with numerous filaments that enter the olfactory bulb where nerve endings. -

Thoracic Anatomy Autonomic Nervous System
Thoracic anatomy Autonomic nervous system Thoracic Anatomy 3.G.1.1 James Mitchell (December 24, 2003) Autonomic nervous system Division by direction Visceral efferent Preganglionic myelinated, postganglionic unmyelinated Synapse in ganglia Visceral afferent Similar to somatic afferent Cell body in CNS, peripheral processes travel with autonomic and somatic fibres Division by outflow Sympathetic Thoracolumbar outflow: T1-L3 Synapse in sympathetic trunk ganglia or other ganglia near CNS Preganglionic cholinergic, postganglionic predominantly noradrenergic (also adrenergic, cholinergic sudomotor and purinergic) Parasympathetic Craniosacral outflow: III, VII, IX, X, S2-4 Synapse adjacent to end-organs Cranial nerve parasympathetic ganglia are traversed by other fibres but contain only parasympathetic synapses Parasympathetic anatomy III Edinger-Westphal nuclei → oculomotor n. → n. to inferior oblique → ciliary ganglion → short ciliary nn. → ciliary muscle and sphincter pupillae VII Superior salivatory nucleus → nervus intermedius → facial n. → chorda tympani → lingual n. → submandibular ganglion → submandibular and sublingual glands Geniculate ganglion → greater petrosal n. → pterygopalatine ganglion → zygomatic and lacrimal nerves to lacrimal gland and nasal and palatine branches to nasal mucosa XI Inferior salivatory nucleus → glossopharyngeal nerve → tympanic plexus → lesser petrosal n. → otic ganglion → auriculotemporal n. → parotid gland and oral mucosa X Dorsal nucleus of vagus → vagus n. → minute ganglia in respiratory tract, heart, -

Sympathetic Tales: Subdivisons of the Autonomic Nervous System and the Impact of Developmental Studies Uwe Ernsberger* and Hermann Rohrer
Ernsberger and Rohrer Neural Development (2018) 13:20 https://doi.org/10.1186/s13064-018-0117-6 REVIEW Open Access Sympathetic tales: subdivisons of the autonomic nervous system and the impact of developmental studies Uwe Ernsberger* and Hermann Rohrer Abstract Remarkable progress in a range of biomedical disciplines has promoted the understanding of the cellular components of the autonomic nervous system and their differentiation during development to a critical level. Characterization of the gene expression fingerprints of individual neurons and identification of the key regulators of autonomic neuron differentiation enables us to comprehend the development of different sets of autonomic neurons. Their individual functional properties emerge as a consequence of differential gene expression initiated by the action of specific developmental regulators. In this review, we delineate the anatomical and physiological observations that led to the subdivision into sympathetic and parasympathetic domains and analyze how the recent molecular insights melt into and challenge the classical description of the autonomic nervous system. Keywords: Sympathetic, Parasympathetic, Transcription factor, Preganglionic, Postganglionic, Autonomic nervous system, Sacral, Pelvic ganglion, Heart Background interplay of nervous and hormonal control in particular The “great sympathetic”... “was the principal means of mediated by the sympathetic nervous system and the ad- bringing about the sympathies of the body”. With these renal gland in adapting the internal -

Neuropeptides and the Innervation of the Avian Lacrimal Gland
Investigative Ophthalmology & Visual Science, Vol. 30, No. 7, July 1989 Copyright © Association for Research in Vision and Ophthalmology Neuropeptides and the Innervation of the Avian Lacrimal Gland Denjomin Wolcorr,* Patrick A. 5ibony,j- and Kent T. Keyser^: The chicken Harderian gland, the major lacrimal gland, has two major cell populations: a cortical secretory epithelium and a medullary interstitial cell population of lymphoid cells. There is an exten- sive acetylcholinesterase (AChE) network throughout the gland, as well as catecholamine positive fibers among the interstitial cells. There are substance P-like (SPLI) and vasoactive intestinal poly- peptide-like (VIPLI) immunoreactivite fibers throughout the gland. These fibers are particularly dense and varicose among the interstitial cells. The adjacent pterygopalatine ganglion complex has neuronal somata that exhibit VIPLI and were AChE-positive. This ganglion complex also contains SPLI and catecholamine-positive fibers. In regions of the ganglion, the somata appear surrounded by SPLI varicosities. Surgical ablation of the ganglion eliminated or reduced the VIPLI, AChE and catecholamine staining in the gland. The SPLI was reduced only in some regions. Ablation of the superior cervical ganglion or severance of the radix autonomica resulted in the loss of catecholamine staining in the pterygopalatine ganglion and the gland. Severance of the ophthalmic or infraorbital nerves had no effect on the VIPLI or the SPLI staining pattern in the gland. Invest Ophthalmol Vis Sci 30:1666-1674, 1989 The avian Harderian gland is the major source of further investigation. Using immunohistochemical serous fluid1 and immunoglobulins2 in tears. Like the techniques and surgical ablations, the source, pat- mammalian lacrimal gland, it is innervated by both terns and regional distribution of cholinergic, adren- sympathetic and parasympathetic nerve fibers.34 The ergic and neuropeptide innervation of the chicken avian gland differs from the mammalian lacrimal Harderian gland were studied. -

Autonomic Nerve Regulation for Prostate Cancer: Study Based on the Tissue Transcriptional Analysis
6767 Original Article Autonomic nerve regulation for prostate cancer: study based on the tissue transcriptional analysis Fang Liu1#, Huan Xu2#, Junyi Chen3#, Bo Yang2, Lin Zhao2, Jin Ji2, Zhi Cao2, Ji Lyu2, Fubo Wang2 1Department of Urology, Pingxiang People’s Hospital, Pingxiang, China; 2Department of Urology, Shanghai Changhai Hospital, Second Military Medical University, Shanghai, China; 3Department of Urology, the Second Affiliated Hospital of Fujian Medical University, Quanzhou, China Contributions: (I) Conception and design: H Xu; (II) Administrative support: F Wang; (III) Provision of study materials or patients: F Liu, J Chen, J Lyu; (IV) Collection and assembly of data: B Yang; (V) Data analysis and interpretation: L Zhao, J Ji, Z Cao; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Fubo Wang. Department of Urology, Shanghai Changhai Hospital, Second Military Medical University, 168 Changhai Road, Shanghai, China. Email: [email protected]. Background: The whole-body energy metabolism is regulated by autonomic nerves which also play important roles in the regulation of the generation and development of different kinds of cancers. This study is to analyze the expression of autonomic nerve receptors and their relationship with the development of prostate cancer (PCa) and to further understand the central regulation of the prostate. Methods: RNA sequencing data concerning autonomic nerve receptors from paired tumor and adjacent benign tissues from 65 patients were collected. The mRNA expression and patient data were analyzed. The Cancer Genome Atlas (TCGA) data confirmed the results, and Pearson analysis, Pearson heat maps, gene heat maps, multivariate logistic regression models, receiver operating characteristic (ROC) curves and Gene Set Enrichment Analysis (GSEA) and Pearson’s analysis were analyzed for correlation analysis in this study. -

Nerve Cell Bodies and Small Ganglia in the Connective Tissue Stroma of Human Submandibular Glands
Neuroscience Letters 475 (2010) 53–55 Contents lists available at ScienceDirect Neuroscience Letters journal homepage: www.elsevier.com/locate/neulet Nerve cell bodies and small ganglia in the connective tissue stroma of human submandibular glands Konstantinos I. Tosios a,∗, Michail Nikolakis a, Andreas Christoforos Prigkos a, Smaragda Diamanti a,b, Alexandra Sklavounou a a Department of Oral Pathology, Dental School, National and Kapodistrian University of Athens, 11527 Athens, Greece b Stomatology Clinic, 251 Hellenic Air Force General Hospital, Athens, Greece article info abstract Article history: The objective of the study was to investigate the presence and distribution of nerve cell bodies and Received 13 February 2010 small ganglia in the stroma of human submandibular gland. A retrospective immunohistochemical study Received in revised form 15 March 2010 in 13 human submandibular glands, fixed in neutral buffered formalin and embedded in paraffin wax, Accepted 16 March 2010 was undertaken. Six glands were excised in the course of radical neck dissection for oral squamous cell carcinoma and were disease-free, six showed sialadenitis, and one was involved by tuberculosis. Primary Keywords: antibodies applied were neuron specific enolase, synaptophysin, and glial fibrilliary acidic protein. Neuron Salivary glands specific enolase and synaptophysin positive nerve cell bodies and small ganglia were found in 8/13 and Submandibular gland Nerve tissue 13/13 glands, respectively. They were found in the interlobular connective tissue stroma of human SMG, Ganglion cells in close association to salivary parenchymal cells and blood vessels, and some of them were incorporated in GFAP positive peripheral nerves. To our knowledge, nerve cell bodies and small ganglia have been described only in the connective tissue stroma of autotransplanted human SMG and their functional importance is not clear. -

Synaptic Transmission and Modulation in Submandibular Ganglia: Aspects of a Current-Clamp Study
Bull. Tokyo dent. Coll., Vol. 41, No. 4, pp.149ϳ167, November, 2000 149 Review Article SYNAPTIC TRANSMISSION AND MODULATION IN SUBMANDIBULAR GANGLIA: ASPECTS OF A CURRENT-CLAMP STUDY TAKASHI SUZUKI Department of Physiology, Tokyo Dental College, 1-2-2 Masago, Mihama-ku, Chiba 261-8502, Japan Received 8 September, 2000/Accepted for Publication 10 October, 2000 Abstract The superior salivatory nucleus in the medulla oblongata is the parasympathetic center of the sublingual and the submandibular (SM) glands. The preganglionic axons originating in this parasympathetic center connect postganglionic neurons in the sub- mandibular ganglia. In spite of an earlier electrophysiological study by Langley in 189013), intracellular electrical studies on SM ganglion neurons had not been done because of the technical difficulties in impaling neurons. It was in only 1972 that the authors begun the intracellular electrical studies of SM ganglia in adult rats and hamsters. In this review, we describe the membrane properties of neurons, spontaneous activities of neurons, types of connection between pre- and post-ganglionic neurons, synaptic potentials including fast EPSP, slow IPSP, slow EPSP and slow hyperpolarizing synaptic potential, characteris- tics of the reflex spike discharges and modulation of synaptic transmission by biogenic substances in SM ganglion neurons. Transfer of information within the ganglia is more complex than simple nicotinic-cholinergic relay, and seems to be specialized for compat- ibility with the salivary glands. These data reflect the specific characteristics of synaptic transmission in the SM ganglia. Key words: Membrane properties—Spontaneous membrane activities— Postsynaptic potentials—Biogenic substances—Reflex spike discharges INTRODUCTION humans, it causes release of small amounts of saliva with rich organic constituents from The salivary glands5,13) are supplied with major salivary glands. -

The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction
Journal of Cardiovascular Development and Disease Review The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction Laura Fedele * and Thomas Brand * Developmental Dynamics, National Heart and Lung Institute (NHLI), Imperial College, London W12 0NN, UK * Correspondence: [email protected] (L.F.); [email protected] (T.B.); Tel.: +44-(0)-207-594-6531 (L.F.); +44-(0)-207-594-8744 (T.B.) Received: 17 August 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: The cardiac autonomic nervous system (CANS) plays a key role for the regulation of cardiac activity with its dysregulation being involved in various heart diseases, such as cardiac arrhythmias. The CANS comprises the extrinsic and intrinsic innervation of the heart. The intrinsic cardiac nervous system (ICNS) includes the network of the intracardiac ganglia and interconnecting neurons. The cardiac ganglia contribute to the tight modulation of cardiac electrophysiology, working as a local hub integrating the inputs of the extrinsic innervation and the ICNS. A better understanding of the role of the ICNS for the modulation of the cardiac conduction system will be crucial for targeted therapies of various arrhythmias. We describe the embryonic development, anatomy, and physiology of the ICNS. By correlating the topography of the intracardiac neurons with what is known regarding their biophysical and neurochemical properties, we outline their physiological role in the control of pacemaker activity of the sinoatrial and atrioventricular nodes. We conclude by highlighting cardiac disorders with a putative involvement of the ICNS and outline open questions that need to be addressed in order to better understand the physiology and pathophysiology of the ICNS. -

The Effects of Sympathetic Nerve Damage on Satellite Glial Cells in The
Autonomic Neuroscience: Basic and Clinical 221 (2019) 102584 Contents lists available at ScienceDirect Autonomic Neuroscience: Basic and Clinical journal homepage: www.elsevier.com/locate/autneu The effects of sympathetic nerve damage on satellite glial cells in the mouse superior cervical ganglion T ⁎ Rachel Feldman-Goriachnik, Menachem Hanani Laboratory of Experimental Surgery, Hadassah-Hebrew University Medical Center, Mount Scopus, Jerusalem 91240, Israel Faculty of Medicine, Hebrew University of Jerusalem, Israel ARTICLE INFO ABSTRACT Keywords: Neurons in sensory, sympathetic, and parasympathetic ganglia are surrounded by satellite glial cell (SGCs). Superior cervical ganglion There is little information on the effects of nerve damage on SGCs in autonomic ganglia. We studied the con- Satellite glial cells sequences of damage to sympathetic nerve terminals by 6-hydroxydopamine (6-OHDA) on SGCs in the mouse Gap junctions superior cervical ganglia (Sup-CG). Immunostaining revealed that at 1–30 d post-6-OHDA injection, SGCs in Sup- Purinergic receptors CG were activated, as assayed by upregulation of glial fibrillary acidic protein. Intracellular labeling showed that Sympathetctomy dye coupling between SGCs around different neurons increased 4-6-fold 1-14 d after 6-OHDA injection. Trigeminal ganglion Behavioral testing 1–7 d post-6-OHDA showed that withdrawal threshold to tactile stimulation of the hind paws was reduced by 65–85%, consistent with hypersensitivity. A single intraperitoneal injection of the gap junction blocker carbenoxolone restored normal tactile thresholds in 6-OHDA-treated mice, suggesting a contribution of SGC gap junctions to pain. Using calcium imaging we found that after 6-OHDA treatment responses of SGCs to ATP were increased by about 30% compared with controls, but responses to ACh were reduced by 48%.