Valnoctamide and Sec-Butyl-Propylacetamide (SPD) for Acute Seizures and Status Epilepticus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms of Action of Antiepileptic Drugs
Review Mechanisms of action of antiepileptic drugs Epilepsy affects up to 1% of the general population and causes substantial disability. The management of seizures in patients with epilepsy relies heavily on antiepileptic drugs (AEDs). Phenobarbital, phenytoin, carbamazepine and valproic acid have been the primary medications used to treat epilepsy for several decades. Since 1993 several AEDs have been approved by the US FDA for use in epilepsy. The choice of the AED is based primarily on the seizure type, spectrum of clinical activity, side effect profile and patient characteristics such as age, comorbidities and concurrent medical treatments. Those AEDs with broad- spectrum activity are often found to exert an action at more than one molecular target. This article will review the proposed mechanisms of action of marketed AEDs in the US and discuss the future of AEDs in development. 1 KEYWORDS: AEDs anticonvulsant drugs antiepileptic drugs epilepsy Aaron M Cook mechanism of action seizures & Meriem K Bensalem-Owen† The therapeutic armamentarium for the treat- patients with refractory seizures. The aim of this 1UK HealthCare, 800 Rose St. H-109, ment of seizures has broadened significantly article is to discuss the past, present and future of Lexington, KY 40536-0293, USA †Author for correspondence: over the past decade [1]. Many of the newer AED pharmacology and mechanisms of action. College of Medicine, Department of anti epileptic drugs (AEDs) have clinical advan- Neurology, University of Kentucky, 800 Rose Street, Room L-455, tages over older, so-called ‘first-generation’ First-generation AEDs Lexington, KY 40536, USA AEDs in that they are more predictable in their Broadly, the mechanisms of action of AEDs can Tel.: +1 859 323 0229 Fax: +1 859 323 5943 dose–response profile and typically are associ- be categorized by their effects on the neuronal [email protected] ated with less drug–drug interactions. -
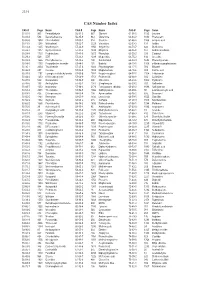
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

Use of Prescribed Psychotropics During Pregnancy: a Systematic Review of Pregnancy, Neonatal, and Childhood Outcomes
brain sciences Review Use of Prescribed Psychotropics during Pregnancy: A Systematic Review of Pregnancy, Neonatal, and Childhood Outcomes Catherine E. Creeley * and Lisa K. Denton Department of Psychology, State University of New York at Fredonia, Fredonia, NY 14063 USA; [email protected] * Correspondence: [email protected]; Tel.: +1-716-673-3890 Received: 19 July 2019; Accepted: 9 September 2019; Published: 14 September 2019 Abstract: This paper reviews the findings from preclinical animal and human clinical research investigating maternal/fetal, neonatal, and child neurodevelopmental outcomes following prenatal exposure to psychotropic drugs. Evidence for the risks associated with prenatal exposure was examined, including teratogenicity, neurodevelopmental effects, neonatal toxicity, and long-term neurobehavioral consequences (i.e., behavioral teratogenicity). We conducted a comprehensive review of the recent results and conclusions of original research and reviews, respectively, which have investigated the short- and long-term impact of drugs commonly prescribed to pregnant women for psychological disorders, including mood, anxiety, and sleep disorders. Because mental illness in the mother is not a benign event, and may itself pose significant risks to both mother and child, simply discontinuing or avoiding medication use during pregnancy may not be possible. Therefore, prenatal exposure to psychotropic drugs is a major public health concern. Decisions regarding drug choice, dose, and duration should be made carefully, by balancing severity, chronicity, and co-morbidity of the mental illness, disorder, or condition against the potential risk for adverse outcomes due to drug exposure. Globally, maternal mental health problems are considered as a major public health challenge, which requires a stronger focus on mental health services that will benefit both mother and child. -

(CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 1: Background and Methods of the Development of Guidelines Konstantinos N
Copyedited by: oup International Journal of Neuropsychopharmacology (2017) 20(2): 95–97 doi:10.1093/ijnp/pyx002 Editorial EDITORIAL Treatment Guidelines in Bipolar Disorders and the Importance of Proper Clinical Trial Design Mauricio Tohen Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, Albuquerque, New Mexico. Correspondence: Mauricio Tohen, MD, DrPH, MBA, Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, 2400 Tucker Ave, Albuquerque, NM 87131, USA ([email protected]). A working group led by Dr. Konstantinos Fountoulakis developed (http://clinicaltrials.gov and http://www.clinicalstudyresults. the first International College of Neuropsychopharmacology org) as well as web pages of pharmaceutical companies with (CINP) clinical guidelines for the treatment of Bipolar Disorders compounds used in bipolar disorder up to March 25, 2016. in adult patients. Their work is very thoroughly described in The authors provide a critical analysis of the existing treat- four separate papers (parts) included in this issue of the journal. ment grading methods that led them to determine that there The first article is Background and Methods of the Development was no optimal method to grade treatments for bipolar disorder, of Guidelines (Fountoulakis et al., 2017d); part 2 is Review, therefore creating their own grading system. Their methodology Grading of the Evidence, and a Precise Algorithm (Fountoulakis provides 32 different levels of recommendations, starting with et al., 2017c); part 3 is The Clinical Guidelines (Fountoulakis the optimal: “At least 1 positive 2 active arm RCT vs placebo et al., 2017a); and Part 4 is Unmet Needs in the Treatment of exists, plus positive 1 active arm RCTs, and no negative RCTs.” Bipolar Disorder and Recommendations for Future Research Lower level scenarios take into account posthoc reports, meta- (Fountoulakis et al., 2017b). -

Stereoselective Anticonvulsant and Pharmacokinetic Analysis of Valnoctamide, a CNS-Active Derivative of Valproic Acid with Low Teratogenic Potential
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Epilepsia Manuscript Author . Author manuscript; Manuscript Author available in PMC 2016 July 28. Published in final edited form as: Epilepsia. 2014 February ; 55(2): 353–361. doi:10.1111/epi.12480. Stereoselective Anticonvulsant and Pharmacokinetic Analysis of Valnoctamide, a CNS-Active Derivative of Valproic Acid with Low Teratogenic Potential Tawfeeq Shekh-Ahmad1, Naama Hen1, Boris Yagen1,2, John H. McDonough3, Richard H. Finnell4, Bogdan J. Wlodarczyk4, and Meir Bialer1,2 1School of Pharmacy, Institute for Drug Research, Faculty of Medicine, The Hebrew University of Jerusalem, Jerusalem 91120, Israel 2David R. Bloom Center for Pharmacy, The Hebrew University of Jerusalem, Israel 3Pharmacology Branch, Research Division, US Army Medical Research Institute of Chemical Defense, Maryland, USA 4Department of Nutritional Sciences, Dell Pediatric Research Institute, The University of Texas at Austin, Austin, Texas, USA Summary Objective—Valnoctamide (VCD), a CNS-active chiral constitutional isomer of valpromide the corresponding amide of valproic acid (VPA), is currently undergoing phase IIb clinical trial in acute mania. VCD exhibits stereoselective pharmacokinetics (PK) in animals and humans. The current study comparatively evaluated the pharmacodynamics (PD; anticonvulsant activity and teratogenicity) and PK of VCD four individual stereoisomers. Methods—The anticonvulsant activity of VCD individual stereoisomers was evaluated in several rodent anticonvulsant models including: maximal electroshock, 6Hz psychomotor, subcutaneous metrazol and the pilocarpine- and soman-induced status epilepticus (SE). The PK- PD (anticonvulsant activity) relationship of VCD stereoisomers was evaluated following ip administration (70mg/kg) to rats. Induction of neural tube defects (NTDs) by VCD stereoisomers was evaluated in a mouse strain highly-susceptible to teratogen-induced neural tube defects. -
ARCI Uniform Classification Guidelines for Foreign Substances, Or Similar State Regulatory Guidelines, Shall Be Assigned Points As Follows
DRUG TESTING STANDARDS AND PRACTICES PROGRAM. Uniform Classification Guidelines for Foreign Substances And Recommended Penalties Model Rule. January, 2019 (V.14.0) © ASSOCIATION OF RACING COMMISSIONERS INTERNATIONAL – 2019. Association of Racing Commissioners International 2365 Harrodsburg Road- B450 Lexington, Kentucky, USA www.arci.com Page 1 of 66 Preamble to the Uniform Classification Guidelines of Foreign Substances The Preamble to the Uniform Classification Guidelines was approved by the RCI Drug Testing and Quality Assurance Program Committee (now the Drug Testing Standards and Practices Program Committee) on August 26, 1991. Minor revisions to the Preamble were made by the Drug Classification subcommittee (now the Veterinary Pharmacologists Subcommittee) on September 3, 1991. "The Uniform Classification Guidelines printed on the following pages are intended to assist stewards, hearing officers and racing commissioners in evaluating the seriousness of alleged violations of medication and prohibited substance rules in racing jurisdictions. Practicing equine veterinarians, state veterinarians, and equine pharmacologists are available and should be consulted to explain the pharmacological effects of the drugs listed in each class prior to any decisions with respect to penalities to be imposed. The ranking of drugs is based on their pharmacology, their ability to influence the outcome of a race, whether or not they have legitimate therapeutic uses in the racing horse, or other evidence that they may be used improperly. These classes of drugs are intended only as guidelines and should be employed only to assist persons adjudicating facts and opinions in understanding the seriousness of the alleged offenses. The facts of each case are always different and there may be mitigating circumstances which should always be considered. -

Medicines Regulations 1984 (SR 1984/143)
Reprint as at 30 March 2021 Medicines Regulations 1984 (SR 1984/143) David Beattie, Governor-General Order in Council At the Government House at Wellington this 5th day of June 1984 Present: His Excellency the Governor-General in Council Pursuant to section 105 of the Medicines Act 1981, and, in the case of Part 3 of the regulations, to section 62 of that Act, His Excellency the Governor-General, acting on the advice of the Minister of Health tendered after consultation with the organisations and bodies that appeared to the Minister to be representatives of persons likely to be substantially affected, and by and with the advice and consent of the Executive Coun- cil, hereby makes the following regulations. Contents Page 1 Title and commencement 5 2 Interpretation 5 Part 1 Classification of medicines 3 Classification of medicines 9 Note Changes authorised by subpart 2 of Part 2 of the Legislation Act 2012 have been made in this official reprint. Note 4 at the end of this reprint provides a list of the amendments incorporated. These regulations are administered by the Ministry of Health. 1 Reprinted as at Medicines Regulations 1984 30 March 2021 Part 2 Standards 4 Standards for medicines, related products, medical devices, 10 cosmetics, and surgical dressings 4A Standard for CBD products 10 5 Pharmacist may dilute medicine in particular case 11 6 Colouring substances [Revoked] 11 Part 3 Advertisements 7 Advertisements not to claim official approval 11 8 Advertisements for medicines 11 9 Advertisements for related products 13 10 Advertisements -

Medicines Amendment Regulations 2018
2018/179 Medicines Amendment Regulations 2018 Patsy Reddy, Governor-General Order in Council At Wellington this 24th day of September 2018 Present: Her Excellency the Governor-General in Council These regulations are made under section 105(1)(j) of the Medicines Act 1981— (a) on the advice and with the consent of the Executive Council; and (b) on the advice of the Minister of Health tendered after consultation with the organisations or bodies appearing to the Minister to be representative of per- sons likely to be substantially affected. Contents Page 1 Title 1 2 Commencement 2 3 Principal regulations 2 4 Schedule 1 replaced 2 5 Regulations revoked 2 Schedule 2 Schedule 1 replaced Regulations 1 Title These regulations are the Medicines Amendment Regulations 2018. 1 r 2 Medicines Amendment Regulations 2018 2018/179 2 Commencement These regulations come into force on the 28th day after the date of their notifi- cation in the Gazette. 3 Principal regulations These regulations amend the Medicines Regulations 1984 (the principal regu- lations). 4 Schedule 1 replaced Replace Schedule 1 with the Schedule 1 set out in the Schedule of these regula- tions. 5 Regulations revoked The Medicines Amendment Regulations (No 2) 2015 (LI 2015/180) are revoked. Schedule Schedule 1 replaced r 4 Schedule 1 Prescription, restricted, and pharmacy-only medicines r 3 Every reference to a medicine in this schedule applies whether the medicine is syn- thetic in origin or is from biological or mineral sources. Unless specific reference is made otherwise, every reference applies also to medicines that are— • preparations and admixtures containing any proportion of any substance listed in this schedule: • salts and esters of any substance listed in this schedule: • preparations or extracts of biological materials listed in this schedule: • salts or oxides of elements listed in this schedule. -

TEXAS RACING COMMISSION January 28, 2021 To
TEXAS RACING COMMISSION P. O. Box 12080, Austin, Texas 78711-2080 8505 Cross Park Drive, Suite 110, Austin, Texas 78754-4552 Phone (512) 833-6699 Fax (512) 833-6907 www.txrc.texas.gov January 28, 2021 To: Stewards, Commission Veterinarians, Test Barn Supervisors, Practicing Veterinarians, Owners, and Trainers From: Chuck Trout, Executive Director Re: Effective February 25, 2021 changes to the following documents: • Permissible Levels of Therapeutic Medications and Naturally Occurring Substances • Equine Medication Classification Policy and Penalty Guidelines • Equine Medication Classification List. This memo is to provide notice that the above listed documents are to be replaced effective this date. The changes include, but are not limited to: • Changes to the list of Permissible Levels of Therapeutic Medications and Naturally Occurring Substances; • Changes to the Equine Medication Classification Policy and Penalty Guidelines; • Changes to the Equine Medication Classification List. These documents are subject to further revision at any time. Test Barn Supervisors - please post this memo and the revised documents in the test barn as soon as possible. Also, please distribute copies of the Permissible Levels of Therapeutic Medications and Naturally Occurring Substances and Equine Medication Classification List to the practicing veterinarians at your racetrack. Licensing Staff - please post this memo and the revised documents where they may be viewed by the public as soon as possible. Copies of these documents will be made available on the Commission's website at http://www.txrc.texas.gov. Attachments: Permissible Levels of Therapeutic Medications and Naturally Occurring Substances Equine Medication Classification Policy and Penalty Guidelines Equine Medication Classification List TEXAS RACING COMMISSION P. -

1.3.1.3 Patient Information Leaflet
Sandoz Business use only Page 1 of 9 1.3.1 spc-label-pl - common-pl - 4,519 20140527 (NL/H/0238/002/IB/040) CARBAMAZEPINE 200 MG PROLONGED RELEASE TABLET 551-031D.00 PACKAGE LEAFLET PACKAGE LEAFLET: INFORMATION FOR THE PATIENT [Nationally completed name, 200 mg, retard tablet] Carbamazepine Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor or pharmacist. This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What [Nationally completed name] is and what it is used for 2. What you need to know before you take [Nationally completed name] 3. How to take [Nationally completed name] 4. Possible side effects 5. How to store [Nationally completed name] 6. Contents of the pack and other information 1. What [Nationally completed name] is and what it is used for Carbamazepine, the active ingredient in [nationally completed name], can affect the body in several different ways. It is an anti-convulsant medicine (prevents fits), it can also modify some types of pain and can control mood disorders. This medicine is used: To treat some forms of epilepsy 2. -

Valproic Acid and Its Amidic Derivatives As New Antivirals Against Alphaherpesviruses
viruses Review Valproic Acid and Its Amidic Derivatives as New Antivirals against Alphaherpesviruses Sabina Andreu 1,2,* , Inés Ripa 1,2, Raquel Bello-Morales 1,2 and José Antonio López-Guerrero 1,2 1 Departamento de Biología Molecular, Universidad Autónoma de Madrid, Cantoblanco, 28049 Madrid, Spain; [email protected] (I.R.); [email protected] (R.B.-M.); [email protected] (J.A.L.-G.) 2 Centro de Biología Molecular Severo Ochoa, Spanish National Research Council—Universidad Autónoma de Madrid (CSIC-UAM), Cantoblanco, 28049 Madrid, Spain * Correspondence: [email protected] Academic Editor: Maria Kalamvoki Received: 14 November 2020; Accepted: 25 November 2020; Published: 26 November 2020 Abstract: Herpes simplex viruses (HSVs) are neurotropic viruses with broad host range whose infections cause considerable health problems in both animals and humans. In fact, 67% of the global population under the age of 50 are infected with HSV-1 and 13% have clinically recurrent HSV-2 infections. The most prescribed antiherpetics are nucleoside analogues such as acyclovir, but the emergence of mutants resistant to these drugs and the lack of available vaccines against human HSVs has led to an imminent need for new antivirals. Valproic acid (VPA) is a branched short-chain fatty acid clinically used as a broad-spectrum antiepileptic drug in the treatment of neurological disorders, which has shown promising antiviral activity against some herpesviruses. Moreover, its amidic derivatives valpromide and valnoctamide also share this antiherpetic activity. This review summarizes the current research on the use of VPA and its amidic derivatives as alternatives to traditional antiherpetics in the fight against HSV infections.