Stereoselective Anticonvulsant and Pharmacokinetic Analysis of Valnoctamide, a CNS-Active Derivative of Valproic Acid with Low Teratogenic Potential
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms of Action of Antiepileptic Drugs
Review Mechanisms of action of antiepileptic drugs Epilepsy affects up to 1% of the general population and causes substantial disability. The management of seizures in patients with epilepsy relies heavily on antiepileptic drugs (AEDs). Phenobarbital, phenytoin, carbamazepine and valproic acid have been the primary medications used to treat epilepsy for several decades. Since 1993 several AEDs have been approved by the US FDA for use in epilepsy. The choice of the AED is based primarily on the seizure type, spectrum of clinical activity, side effect profile and patient characteristics such as age, comorbidities and concurrent medical treatments. Those AEDs with broad- spectrum activity are often found to exert an action at more than one molecular target. This article will review the proposed mechanisms of action of marketed AEDs in the US and discuss the future of AEDs in development. 1 KEYWORDS: AEDs anticonvulsant drugs antiepileptic drugs epilepsy Aaron M Cook mechanism of action seizures & Meriem K Bensalem-Owen† The therapeutic armamentarium for the treat- patients with refractory seizures. The aim of this 1UK HealthCare, 800 Rose St. H-109, ment of seizures has broadened significantly article is to discuss the past, present and future of Lexington, KY 40536-0293, USA †Author for correspondence: over the past decade [1]. Many of the newer AED pharmacology and mechanisms of action. College of Medicine, Department of anti epileptic drugs (AEDs) have clinical advan- Neurology, University of Kentucky, 800 Rose Street, Room L-455, tages over older, so-called ‘first-generation’ First-generation AEDs Lexington, KY 40536, USA AEDs in that they are more predictable in their Broadly, the mechanisms of action of AEDs can Tel.: +1 859 323 0229 Fax: +1 859 323 5943 dose–response profile and typically are associ- be categorized by their effects on the neuronal [email protected] ated with less drug–drug interactions. -

Valproic Acid and Its Amidic Derivatives As New Antivirals Against Alphaherpesviruses
viruses Review Valproic Acid and Its Amidic Derivatives as New Antivirals against Alphaherpesviruses Sabina Andreu 1,2,* , Inés Ripa 1,2, Raquel Bello-Morales 1,2 and José Antonio López-Guerrero 1,2 1 Departamento de Biología Molecular, Universidad Autónoma de Madrid, Cantoblanco, 28049 Madrid, Spain; [email protected] (I.R.); [email protected] (R.B.-M.); [email protected] (J.A.L.-G.) 2 Centro de Biología Molecular Severo Ochoa, Spanish National Research Council—Universidad Autónoma de Madrid (CSIC-UAM), Cantoblanco, 28049 Madrid, Spain * Correspondence: [email protected] Academic Editor: Maria Kalamvoki Received: 14 November 2020; Accepted: 25 November 2020; Published: 26 November 2020 Abstract: Herpes simplex viruses (HSVs) are neurotropic viruses with broad host range whose infections cause considerable health problems in both animals and humans. In fact, 67% of the global population under the age of 50 are infected with HSV-1 and 13% have clinically recurrent HSV-2 infections. The most prescribed antiherpetics are nucleoside analogues such as acyclovir, but the emergence of mutants resistant to these drugs and the lack of available vaccines against human HSVs has led to an imminent need for new antivirals. Valproic acid (VPA) is a branched short-chain fatty acid clinically used as a broad-spectrum antiepileptic drug in the treatment of neurological disorders, which has shown promising antiviral activity against some herpesviruses. Moreover, its amidic derivatives valpromide and valnoctamide also share this antiherpetic activity. This review summarizes the current research on the use of VPA and its amidic derivatives as alternatives to traditional antiherpetics in the fight against HSV infections. -

(12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant Et Al
US 2010.0143507A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant et al. (43) Pub. Date: Jun. 10, 2010 (54) CARBOXYLIC ACID INHIBITORS OF Publication Classification HISTONE DEACETYLASE, GABA (51) Int. Cl. TRANSAMINASE AND SODIUM CHANNEL A633/00 (2006.01) A 6LX 3/553 (2006.01) A 6LX 3/553 (2006.01) (75) Inventors: Thomas G. Gant, Carlsbad, CA A63L/352 (2006.01) (US); Sepehr Sarshar, Cardiff by A6II 3/19 (2006.01) the Sea, CA (US) C07C 53/128 (2006.01) A6IP 25/06 (2006.01) A6IP 25/08 (2006.01) Correspondence Address: A6IP 25/18 (2006.01) GLOBAL PATENT GROUP - APX (52) U.S. Cl. .................... 424/722:514/211.13: 514/221; 10411 Clayton Road, Suite 304 514/456; 514/557; 562/512 ST. LOUIS, MO 63131 (US) (57) ABSTRACT Assignee: AUSPEX The present invention relates to new carboxylic acid inhibi (73) tors of histone deacetylase, GABA transaminase, and/or PHARMACEUTICALS, INC., Sodium channel activity, pharmaceutical compositions Vista, CA (US) thereof, and methods of use thereof. (21) Appl. No.: 12/632,507 Formula I (22) Filed: Dec. 7, 2009 Related U.S. Application Data (60) Provisional application No. 61/121,024, filed on Dec. 9, 2008. US 2010/014.3507 A1 Jun. 10, 2010 CARBOXYLIC ACID INHIBITORS OF HISTONE DEACETYLASE, GABA TRANSAMNASE AND SODIUM CHANNEL 0001. This application claims the benefit of priority of Valproic acid U.S. provisional application No. 61/121,024, filed Dec. 9, 2008, the disclosure of which is hereby incorporated by ref 0004 Valproic acid is extensively metabolised via erence as if written herein in its entirety. -

IJBCP International Journal of Basic & Clinical Pharmacology Antiepileptic
Print ISSN: 2319-2003 | Online ISSN: 2279-0780 IJBCP International Journal of Basic & Clinical Pharmacology DOI: http://dx.doi.org/10.18203/2319-2003.ijbcp20161495 Review Article Antiepileptic drugs: newer targets and new drugs Vihang S. Chawan, Abhishek M. Phatak*, Kalpesh V. Gawand, Sagar V. Badwane, Sagar S. Panchal Department of Pharmacology, TNMC and BYL Nair Ch. Hospital Mumbai, Maharashtra, India ABSTRACT Received: 10 March 2016 Epilepsy is a common neurological disorder affecting 0.5-1% of the population Accepted: 15 April 2016 in India. Majority of patients respond to currently available antiepileptic drugs (AEDs), but a small percentage of patients have shown poor and inadequate *Correspondence to: response to AEDs in addition to various side effects and drug interactions while Dr. Abhishek Madan Phatak, on therapy. Thus there is a need to develop more effective AEDs in drug Email: abhishekphatak9288 resistant epilepsy which have a better safety profile with minimal adverse @gmail.com effects. The United States food and drug administration (USFDA) has approved eslicarbazepine acetate, ezogabine, perampanel and brivaracetam which have Copyright: © the author(s), shown a promising future as better AEDs and drugs like ganaxolone, intranasal publisher and licensee Medip diazepam, ICA- 105665, valnoctamide, VX-765, naluzotan are in the pipeline. Academy. This is an open- access article distributed under Keywords: Epilepsy, Newer antiepileptic drugs, Eslicarbazepine Acetate, the terms of the Creative Ezogabine (Retigabine), Perampanel, Brivaracetam, Naluzotan Commons Attribution Non- Commercial License, which permits unrestricted non- commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. INTRODUCTION to AEDs or those patient who have suffered from recurrent seizures, may require surgery. -

Valnoctamide and Sec-Butyl-Propylacetamide (SPD) for Acute Seizures and Status Epilepticus
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Epilepsia Manuscript Author . Author manuscript; Manuscript Author available in PMC 2018 December 17. Published in final edited form as: Epilepsia. 2013 September ; 54(Suppl 6): 99–102. doi:10.1111/epi.12290. Valnoctamide and sec-butyl-propylacetamide (SPD) for acute seizures and status epilepticus Tawfeeq Shekh-Ahmad1, Naama Hen1, John H. McDonough2, Boris Yagen1, and Meir Bialer, PhD1 1Institute for Drug Research, School of Pharmacy, Faculty of Medicine, The Hebrew University of Jerusalem, Israel 2Pharamcology Branch, Research Division, US Army Medical Research Institute of Chemical Defense (MRICD), Aberdeen Proving Ground, Maryland, USA Summary: sec-Butyl-propylacetamide (SPD) is a one-carbon homologue of valnoctamide (VCD), a chiral constitutional isomer of valproic acid’s (VPA) corresponding amide valpromide. VCD has a potential in epilepsy including status epilepticus (SE) and neuropathic pain, and is currently being developed for the treatment of bipolar disorder. Both VCD and SPD possess two stereogenic carbons in their chemical structure. SPD possess a unique and broad-spectrum antiseizure profile superior to that of VPA and better than that of VCD. In addition SPD blocked behavioral- and electrographic-SE induced by pilocarpine and soman (organophosphate nerve gas) and afforded in vivo neuroprotection that was associated with cognitive sparing. VCD has similar activity as SPD in the pilocarpine-induced-SE although at higher doses. The activity of SPD and VCD against SE is superior to that of diazepam in terms of rapid onset, potency and ability to block SE when given 20 to 60 min after seizure onset. When administered 20 and 40min after SE onset, SPD (100–174mg/kg) produced long- lasting efficacy (e.g., 4–8hr) against soman-induced convulsive- and electrographic-SE in both rats and guinea pigs. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -
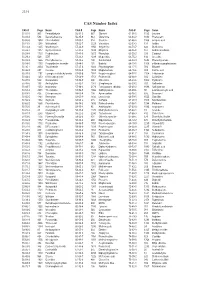
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Pharmacokinetic and Pharmacodynamic Interactions Between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy
University of Kentucky UKnowledge Psychiatry Faculty Publications Psychiatry 11-2014 Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy Edoardo Spina University of Messina, Italy Jose de Leon University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits oy u. Follow this and additional works at: https://uknowledge.uky.edu/psychiatry_facpub Part of the Psychiatry and Psychology Commons Repository Citation Italiano, Domenico; Spina, Edoardo; and de Leon, Jose, "Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants" (2014). Psychiatry Faculty Publications. 40. https://uknowledge.uky.edu/psychiatry_facpub/40 This Article is brought to you for free and open access by the Psychiatry at UKnowledge. It has been accepted for inclusion in Psychiatry Faculty Publications by an authorized administrator of UKnowledge. For more information, please contact [email protected]. Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Notes/Citation Information Published in Expert Opinion on Drug Metabolism & Toxicology, v. 10, Issue 11, p. 1457-1489. © 2014 Taylor & Francis Group This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. 2014, available online: http://www.tandfonline.com/10.1517/ 17425255.2014.956081 Digital Object Identifier (DOI) http://dx.doi.org/10.1517/17425255.2014.956081 This article is available at UKnowledge: https://uknowledge.uky.edu/psychiatry_facpub/40 1 This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau Et Al
US 20150202317A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau et al. (43) Pub. Date: Jul. 23, 2015 (54) DIPEPTDE-BASED PRODRUG LINKERS Publication Classification FOR ALPHATIC AMNE-CONTAINING DRUGS (51) Int. Cl. A647/48 (2006.01) (71) Applicant: Ascendis Pharma A/S, Hellerup (DK) A638/26 (2006.01) A6M5/9 (2006.01) (72) Inventors: Harald Rau, Heidelberg (DE); Torben A 6LX3/553 (2006.01) Le?mann, Neustadt an der Weinstrasse (52) U.S. Cl. (DE) CPC ......... A61K 47/48338 (2013.01); A61 K3I/553 (2013.01); A61 K38/26 (2013.01); A61 K (21) Appl. No.: 14/674,928 47/48215 (2013.01); A61M 5/19 (2013.01) (22) Filed: Mar. 31, 2015 (57) ABSTRACT The present invention relates to a prodrug or a pharmaceuti Related U.S. Application Data cally acceptable salt thereof, comprising a drug linker conju (63) Continuation of application No. 13/574,092, filed on gate D-L, wherein D being a biologically active moiety con Oct. 15, 2012, filed as application No. PCT/EP2011/ taining an aliphatic amine group is conjugated to one or more 050821 on Jan. 21, 2011. polymeric carriers via dipeptide-containing linkers L. Such carrier-linked prodrugs achieve drug releases with therapeu (30) Foreign Application Priority Data tically useful half-lives. The invention also relates to pharma ceutical compositions comprising said prodrugs and their use Jan. 22, 2010 (EP) ................................ 10 151564.1 as medicaments. US 2015/0202317 A1 Jul. 23, 2015 DIPEPTDE-BASED PRODRUG LINKERS 0007 Alternatively, the drugs may be conjugated to a car FOR ALPHATIC AMNE-CONTAINING rier through permanent covalent bonds. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

A History of the Pharmacological Treatment of Bipolar Disorder
International Journal of Molecular Sciences Review A History of the Pharmacological Treatment of Bipolar Disorder Francisco López-Muñoz 1,2,3,4,* ID , Winston W. Shen 5, Pilar D’Ocon 6, Alejandro Romero 7 ID and Cecilio Álamo 8 1 Faculty of Health Sciences, University Camilo José Cela, C/Castillo de Alarcón 49, 28692 Villanueva de la Cañada, Madrid, Spain 2 Neuropsychopharmacology Unit, Hospital 12 de Octubre Research Institute (i+12), Avda. Córdoba, s/n, 28041 Madrid, Spain 3 Portucalense Institute of Neuropsychology and Cognitive and Behavioural Neurosciences (INPP), Portucalense University, R. Dr. António Bernardino de Almeida 541, 4200-072 Porto, Portugal 4 Thematic Network for Cooperative Health Research (RETICS), Addictive Disorders Network, Health Institute Carlos III, MICINN and FEDER, 28029 Madrid, Spain 5 Departments of Psychiatry, Wan Fang Medical Center and School of Medicine, Taipei Medical University, 111 Hsin Long Road Section 3, Taipei 116, Taiwan; [email protected] 6 Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Avda. Vicente Andrés, s/n, 46100 Burjassot, Valencia, Spain; [email protected] 7 Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Complutense University, Avda. Puerta de Hierro, s/n, 28040 Madrid, Spain; [email protected] 8 Department of Biomedical Sciences (Pharmacology Area), Faculty of Medicine and Health Sciences, University of Alcalá, Crta. de Madrid-Barcelona, Km. 33,600, 28871 Alcalá de Henares, Madrid, Spain; [email protected] * Correspondence: fl[email protected] or [email protected] Received: 4 June 2018; Accepted: 13 July 2018; Published: 23 July 2018 Abstract: In this paper, the authors review the history of the pharmacological treatment of bipolar disorder, from the first nonspecific sedative agents introduced in the 19th and early 20th century, such as solanaceae alkaloids, bromides and barbiturates, to John Cade’s experiments with lithium and the beginning of the so-called “Psychopharmacological Revolution” in the 1950s. -

An Inventory of Literature on the Relation Between Drug Use, Impaired Driving and Traffic Accidents
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by National Documentation Centre on Drug Use E.M.C.D.D.A. DRUGS MISUSE RESEARCH DIVISION HEALTH RESEARCH BOARD An Inventory of Literature on the Relation between Drug Use, Impaired Driving and Traffic Accidents CT.97.EP.14 Research Team: Colin Gemmell Trinity College, Dublin Rosalyn Moran Drugs Misuse Research Division, Health Research Board James Crowley Professor, Transport Policy Research Institute, University College Dublin Richeal Courtney Medical Expert, for the Health Research Board EMCDDA: Lucas Wiessing February 1999 Please use the following citation: European Monitoring Centre for Drugs and Drug Addiction. An Inventory of Literature on the Relation betweenDrug Use, Impaired Driving and Traffic Accidents. (CT.97.EP.14) Lisbon: EMCDDA, February 1999. Contact Details Drugs Misuse Research Division Health Research Board 73 Lower Baggot Street Dublin 2 Ireland European Monitoring Centre for Drugs and Drug Addiction Rua Cruz de Santa Apolónia 23/25 1100, Lisboa Portugal. Further copies of this bibliography can be obtained from the EMCDDA at the above address. CREDITS Principal Researchers Ms Rosalyn Moran, Project Leader, Health Research Board Professor James Crowley, Professor, Transport Policy Research Institute, UCD Dr Richeal Courtney, Medical Expert, on behalf of the Health Research Board Research Assistants Colin Gemmell (Synthesis and Final Reports) Sarah Heywood (Literature Search and Collaborative Network) For the EMCDDA Lucas Wiessing