Beyond Lithium in the Treatment of Bipolar Illness Robert M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

View / Download Pdf Version of This Article
role of CALCIUM CHANNEL BLOCKERS in HYPERTENSION KEY POINTS ThIAZIDES ARE APPROPRIATE INITIAL THERAPY FOR MOST PEOPLE WITH HYPERTENSION Thiazides are appropriate initial therapy for most ▪ There is limited evidence of superiority of one antihypertensive people with hypertension. over another but evidence suggests that for most patients, ▪ Choice of other antihypertensives is decided by diuretics can be considered first, based on their effectiveness, individual patient factors. safety and low cost. ▪ Factors which potentially favour use of calcium channel blockers include arrhythmia (verapamil CHOICE OF ADDITIONAL ANTIHYPERTENSIVES only), angina, older age and high risk of stroke. IS DECIDED BY INDIVIDUAL PATIENT FACTORS ▪ Factors which may weigh against the use of Other agents may be chosen for individual patients based calcium channel blockers include potential drug on concurrent medical conditions, patient tolerability and interactions, and diltiazem and verapamil are drug interactions. Indications for treatment with different contraindicated in heart block and heart failure. antihypertensive agents are discussed in BPJ 6 (June 2007). ▪ Choice between the different calcium channel blockers depends on patient tolerability, co- morbidity and drug interactions. FACTORS FOR AND AGAINST THE USE OF CALCIUM chANNEL BLOCKERS Factors that potentially favour the use of calcium channel Factors favouring use of calcium channel blockers include arrhythmia (verapamil only), angina, or high blockers: risk of stroke. Verapamil can also be used post myocardial infarction if beta blockers are contraindicated or not tolerated. ▪ Hypertension with co-morbid angina In addition, calcium channel blockers may be more suitable than other agents for elderly people and those of African ▪ Hypertension with co-morbid arrhythmia 1 (verapamil only) descent. -

Valproic Acid and Its Amidic Derivatives As New Antivirals Against Alphaherpesviruses
viruses Review Valproic Acid and Its Amidic Derivatives as New Antivirals against Alphaherpesviruses Sabina Andreu 1,2,* , Inés Ripa 1,2, Raquel Bello-Morales 1,2 and José Antonio López-Guerrero 1,2 1 Departamento de Biología Molecular, Universidad Autónoma de Madrid, Cantoblanco, 28049 Madrid, Spain; [email protected] (I.R.); [email protected] (R.B.-M.); [email protected] (J.A.L.-G.) 2 Centro de Biología Molecular Severo Ochoa, Spanish National Research Council—Universidad Autónoma de Madrid (CSIC-UAM), Cantoblanco, 28049 Madrid, Spain * Correspondence: [email protected] Academic Editor: Maria Kalamvoki Received: 14 November 2020; Accepted: 25 November 2020; Published: 26 November 2020 Abstract: Herpes simplex viruses (HSVs) are neurotropic viruses with broad host range whose infections cause considerable health problems in both animals and humans. In fact, 67% of the global population under the age of 50 are infected with HSV-1 and 13% have clinically recurrent HSV-2 infections. The most prescribed antiherpetics are nucleoside analogues such as acyclovir, but the emergence of mutants resistant to these drugs and the lack of available vaccines against human HSVs has led to an imminent need for new antivirals. Valproic acid (VPA) is a branched short-chain fatty acid clinically used as a broad-spectrum antiepileptic drug in the treatment of neurological disorders, which has shown promising antiviral activity against some herpesviruses. Moreover, its amidic derivatives valpromide and valnoctamide also share this antiherpetic activity. This review summarizes the current research on the use of VPA and its amidic derivatives as alternatives to traditional antiherpetics in the fight against HSV infections. -

(12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant Et Al
US 2010.0143507A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant et al. (43) Pub. Date: Jun. 10, 2010 (54) CARBOXYLIC ACID INHIBITORS OF Publication Classification HISTONE DEACETYLASE, GABA (51) Int. Cl. TRANSAMINASE AND SODIUM CHANNEL A633/00 (2006.01) A 6LX 3/553 (2006.01) A 6LX 3/553 (2006.01) (75) Inventors: Thomas G. Gant, Carlsbad, CA A63L/352 (2006.01) (US); Sepehr Sarshar, Cardiff by A6II 3/19 (2006.01) the Sea, CA (US) C07C 53/128 (2006.01) A6IP 25/06 (2006.01) A6IP 25/08 (2006.01) Correspondence Address: A6IP 25/18 (2006.01) GLOBAL PATENT GROUP - APX (52) U.S. Cl. .................... 424/722:514/211.13: 514/221; 10411 Clayton Road, Suite 304 514/456; 514/557; 562/512 ST. LOUIS, MO 63131 (US) (57) ABSTRACT Assignee: AUSPEX The present invention relates to new carboxylic acid inhibi (73) tors of histone deacetylase, GABA transaminase, and/or PHARMACEUTICALS, INC., Sodium channel activity, pharmaceutical compositions Vista, CA (US) thereof, and methods of use thereof. (21) Appl. No.: 12/632,507 Formula I (22) Filed: Dec. 7, 2009 Related U.S. Application Data (60) Provisional application No. 61/121,024, filed on Dec. 9, 2008. US 2010/014.3507 A1 Jun. 10, 2010 CARBOXYLIC ACID INHIBITORS OF HISTONE DEACETYLASE, GABA TRANSAMNASE AND SODIUM CHANNEL 0001. This application claims the benefit of priority of Valproic acid U.S. provisional application No. 61/121,024, filed Dec. 9, 2008, the disclosure of which is hereby incorporated by ref 0004 Valproic acid is extensively metabolised via erence as if written herein in its entirety. -

Alcoholism Pharmacotherapy
101 ALCOHOLISM PHARMACOTHERAPY JOSEPH R. VOLPICELLI SUCHITRA KRISHNAN-SARIN STEPHANIE S. O’MALLEY Alcoholism remains one of the most common and signifi- PHARMACOLOGIC TREATMENTS FOR cant medical problems in the United States and internation- ALCOHOL DETOXIFICATION ally. For example, in the United States, over 4% of the general population is alcohol dependent and another 5 to The first step in the pharmacologic treatment of alcoholism 10 million people drink hazardously at least several times is to help patients safely detoxify from alcohol. Although per month (1). The economic and medical costs of alcohol- historically, alcohol detoxification has occurred in inpatient ism and alcohol abuse continue to escalate. Most recent setting, increasingly alcohol detoxification is being con- figures put the economic costs of alcohol-related expenses ducted in ambulatory settings. Except in the case of medical at $176 billion annually in the United States (2). This in- or psychiatric emergencies, outcome studies generally show cludes the economic costs of increased health care expenses, that successful detoxification can safely and effectively be lost productivity at work, and legal expenses. Similarly, al- carried out in ambulatory setting using medications such though there have been some reductions in the number of as benzodiazepines (5,6). In addition, the use of anticonvul motor vehicle deaths attributed to excessive alcohol drink- sants has received recent interest. ing, the overall number of alcohol-related annual deaths is 105,000 in the United States (3). Benzodiazepines Current psychosocial approaches to alcohol addiction are moderately effective, with perhaps as many as half the pa- Benzodiazepines are �-aminobutyric acid (GABA) agonists tients receiving treatment becoming abstinent or signifi- that metaanalysis of placebo-controlled double-blind studies cantly reducing episodes of binge drinking (4). -

IJBCP International Journal of Basic & Clinical Pharmacology Antiepileptic
Print ISSN: 2319-2003 | Online ISSN: 2279-0780 IJBCP International Journal of Basic & Clinical Pharmacology DOI: http://dx.doi.org/10.18203/2319-2003.ijbcp20161495 Review Article Antiepileptic drugs: newer targets and new drugs Vihang S. Chawan, Abhishek M. Phatak*, Kalpesh V. Gawand, Sagar V. Badwane, Sagar S. Panchal Department of Pharmacology, TNMC and BYL Nair Ch. Hospital Mumbai, Maharashtra, India ABSTRACT Received: 10 March 2016 Epilepsy is a common neurological disorder affecting 0.5-1% of the population Accepted: 15 April 2016 in India. Majority of patients respond to currently available antiepileptic drugs (AEDs), but a small percentage of patients have shown poor and inadequate *Correspondence to: response to AEDs in addition to various side effects and drug interactions while Dr. Abhishek Madan Phatak, on therapy. Thus there is a need to develop more effective AEDs in drug Email: abhishekphatak9288 resistant epilepsy which have a better safety profile with minimal adverse @gmail.com effects. The United States food and drug administration (USFDA) has approved eslicarbazepine acetate, ezogabine, perampanel and brivaracetam which have Copyright: © the author(s), shown a promising future as better AEDs and drugs like ganaxolone, intranasal publisher and licensee Medip diazepam, ICA- 105665, valnoctamide, VX-765, naluzotan are in the pipeline. Academy. This is an open- access article distributed under Keywords: Epilepsy, Newer antiepileptic drugs, Eslicarbazepine Acetate, the terms of the Creative Ezogabine (Retigabine), Perampanel, Brivaracetam, Naluzotan Commons Attribution Non- Commercial License, which permits unrestricted non- commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. INTRODUCTION to AEDs or those patient who have suffered from recurrent seizures, may require surgery. -
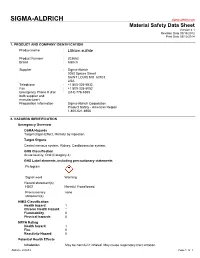
Lithium Sulfate
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Antiparasitic Properties of Cardiovascular Agents Against Human Intravascular Parasite Schistosoma Mansoni
pharmaceuticals Article Antiparasitic Properties of Cardiovascular Agents against Human Intravascular Parasite Schistosoma mansoni Raquel Porto 1, Ana C. Mengarda 1, Rayssa A. Cajas 1, Maria C. Salvadori 2 , Fernanda S. Teixeira 2 , Daniel D. R. Arcanjo 3 , Abolghasem Siyadatpanah 4, Maria de Lourdes Pereira 5 , Polrat Wilairatana 6,* and Josué de Moraes 1,* 1 Research Center for Neglected Diseases, Guarulhos University, Praça Tereza Cristina 229, São Paulo 07023-070, SP, Brazil; [email protected] (R.P.); [email protected] (A.C.M.); [email protected] (R.A.C.) 2 Institute of Physics, University of São Paulo, São Paulo 05508-060, SP, Brazil; [email protected] (M.C.S.); [email protected] (F.S.T.) 3 Department of Biophysics and Physiology, Federal University of Piaui, Teresina 64049-550, PI, Brazil; [email protected] 4 Ferdows School of Paramedical and Health, Birjand University of Medical Sciences, Birjand 9717853577, Iran; [email protected] 5 CICECO-Aveiro Institute of Materials & Department of Medical Sciences, University of Aveiro, 3810-193 Aveiro, Portugal; [email protected] 6 Department of Clinical Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok 10400, Thailand * Correspondence: [email protected] (P.W.); [email protected] (J.d.M.) Citation: Porto, R.; Mengarda, A.C.; Abstract: The intravascular parasitic worm Schistosoma mansoni is a causative agent of schistosomiasis, Cajas, R.A.; Salvadori, M.C.; Teixeira, a disease of great global public health significance. Praziquantel is the only drug available to F.S.; Arcanjo, D.D.R.; Siyadatpanah, treat schistosomiasis and there is an urgent demand for new anthelmintic agents. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -

Management and Treatment of Lithium-Induced Nephrogenic Diabetes Insipidus
REVIEW Management and treatment of lithium- induced nephrogenic diabetes insipidus Christopher K Finch†, Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as Tyson WA Brooks, many as 10 to 15% of patients taking lithium developing this condition. Clinicians have Peggy Yam & Kristi W Kelley been well aware of lithium toxicity for many years; however, the treatment of this drug- induced condition has generally been remedied by discontinuation of the medication or a †Author for correspondence Methodist University reduction in dose. For those patients unresponsive to traditional treatment measures, Hospital, Department several pharmacotherapeutic regimens have been documented as being effective for the of Pharmacy, University of management of lithium-induced diabetes insipidus including hydrochlorothiazide, Tennessee, College of Pharmacy, 1265 Union Ave., amiloride, indomethacin, desmopressin and correction of serum lithium levels. Memphis, TN 38104, USA Tel.: +1 901 516 2954 Fax: +1 901 516 8178 [email protected] Lithium carbonate is well known for its wide use associated with a mutation(s) of vasopressin in bipolar disorders due to its mood stabilizing receptors. Acquired causes are tubulointerstitial properties. It is also employed in aggression dis- disease (e.g., sickle cell disease, amyloidosis, orders, post-traumatic stress disorders, conduct obstructive uropathy), electrolyte disorders (e.g., disorders and even as adjunctive therapy in hypokalemia and hypercalcemia), pregnancy, or depression. Lithium has many well documented conditions induced by a drug (e.g., lithium, adverse effects as well as a relatively narrow ther- demeclocycline, amphotericin B and apeutic range of 0.4 to 0.8 mmol/l. Clinically vincristine) [3,4]. Lithium is the most common significant adverse effects include polyuria, mus- cause of drug-induced nephrogenic DI [5]. -

Subchronic Lithium Treatment Increases the Anxiolytic-Like Effect of Mirtazapine on the Expression of Contextual Title Conditioned Fear
Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual Title conditioned fear Author(s) An, Yan; Inoue, Takeshi; Kitaichi, Yuji; Nakagawa, Shin; Wang, Ce; Chen, Chong; Song, Ning; Kusumi, Ichiro European journal of pharmacology, 747, 13-17 Citation https://doi.org/10.1016/j.ejphar.2014.11.009 Issue Date 2015-01-15 Doc URL http://hdl.handle.net/2115/58243 Type article (author version) File Information AnManuscript.pdf Instructions for use Hokkaido University Collection of Scholarly and Academic Papers : HUSCAP Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual conditioned fear Yan Ana, Takeshi Inouea*, Yuji Kitaichia, Shin Nakagawaa, Ce Wangb, Chong Chena, Ning Songa, Ichiro Kusumia a Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan b Department of Neuropharmacology, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Number of figures: 3 Corresponding address: Takeshi Inoue, Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Phone: +81(11)706-5160 Fax: +81(11)706-5081 E-mail: [email protected] 1 Abstract Lithium not only has a mood-stabilizing effect but also the augmentation effect of an antidepressant, the mechanism of which remains unclear. Although lithium may augment the effect of mirtazapine, this augmentation has not been confirmed. Using a contextual fear conditioning test in rats, an animal model of anxiety or fear, we examined the effect of subchronic lithium carbonate (in diet) in combination with systemic mirtazapine on the expression of contextual conditioned fear. -

Pharmacokinetic and Pharmacodynamic Interactions Between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy
University of Kentucky UKnowledge Psychiatry Faculty Publications Psychiatry 11-2014 Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Domenico Italiano University of Messina, Italy Edoardo Spina University of Messina, Italy Jose de Leon University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits oy u. Follow this and additional works at: https://uknowledge.uky.edu/psychiatry_facpub Part of the Psychiatry and Psychology Commons Repository Citation Italiano, Domenico; Spina, Edoardo; and de Leon, Jose, "Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants" (2014). Psychiatry Faculty Publications. 40. https://uknowledge.uky.edu/psychiatry_facpub/40 This Article is brought to you for free and open access by the Psychiatry at UKnowledge. It has been accepted for inclusion in Psychiatry Faculty Publications by an authorized administrator of UKnowledge. For more information, please contact [email protected]. Pharmacokinetic and Pharmacodynamic Interactions between Antiepileptics and Antidepressants Notes/Citation Information Published in Expert Opinion on Drug Metabolism & Toxicology, v. 10, Issue 11, p. 1457-1489. © 2014 Taylor & Francis Group This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov. 2014, available online: http://www.tandfonline.com/10.1517/ 17425255.2014.956081 Digital Object Identifier (DOI) http://dx.doi.org/10.1517/17425255.2014.956081 This article is available at UKnowledge: https://uknowledge.uky.edu/psychiatry_facpub/40 1 This is an Accepted Manuscript of an article published by Taylor & Francis Group in Expert Opinion on Drug Metabolism & Toxicology in Nov.