(CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 1: Background and Methods of the Development of Guidelines Konstantinos N
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The SULPYCO Method Using Sulpiride Integrated with an Atypical Adjuvant Therapy for Treating Depressive Syndrome: an Observational Study Amgad M
oepidem ac io m lo r g a y Rabie, Adv Pharmacoepidem Drug Safety 2013, 2:1 h & P Advances in Pharmacoepidemiology & D n i DOI: 10.4172/2167-1052.1000126 r u s g e c ISSN: 2167-1052 S n a a f v e t d y A Drug Safety Research Article Open Access The SULPYCO Method Using Sulpiride Integrated with an Atypical Adjuvant Therapy for Treating Depressive Syndrome: An Observational Study Amgad M. Rabie* Pharmaceutical Organic Chemistry Department, Faculty of Pharmacy, Mansoura University, Mansoura, Dakahlia Governorate, Egypt Abstract In this observational study, we studied the effects of a new drug combination on depression. Patients were analyzed before and after antidepressant treatment using the Hamilton rating scale for depression (HAMD). One group of patients was treated with the new integrated medicine consisting of two separate subcutaneous injections of a low dose (20 mg) of sulpiride and a 2.2 ml complex homeopathic solution based on the Krebs cycle elements; each injection was administered once daily. Another group of patients was treated with conventional therapy of 20 mg sulpiride only. The third group was treated with only the homeopathic solution. The differences in the HAMD scores were evaluated before and after 3 months of treatment in these three groups of patients. The HAMD score showed a statistically significant decrease in the group treated with combined sulpiride and homeopathy. This observation suggests that a low parenteral dose (20 mg) of sulpiride, when administered subcutaneously with a complex homeopathic remedy, may give better therapeutic results for mild and moderate depression than either sulpiride or complex homeopathy alone. -

Pharmaceuticals and Medical Devices Safety Information No
Pharmaceuticals and Medical Devices Safety Information No. 258 June 2009 Table of Contents 1. Selective serotonin reuptake inhibitors (SSRIs) and aggression ······································································································································ 3 2. Important Safety Information ······································································· 10 . .1. Isoflurane ························································································· 10 3. Revision of PRECAUTIONS (No. 206) Olmesartan medoxomil (and 3 others)··························································· 15 4. List of products subject to Early Post-marketing Phase Vigilance.....................................................17 Reference 1. Project for promoting safe use of drugs.............................................20 Reference 2. Manuals for Management of Individual Serious Adverse Drug Reactions..................................................................................21 Reference 3. Extension of cooperating hospitals in the project for “Japan Drug Information Institute in Pregnancy” ..............25 This Pharmaceuticals and Medical Devices Safety Information (PMDSI) is issued based on safety information collected by the Ministry of Health, Labour and Welfare. It is intended to facilitate safer use of pharmaceuticals and medical devices by healthcare providers. PMDSI is available on the Pharmaceuticals and Medical Devices Agency website (http://www.pmda.go.jp/english/index.html) and on the -

Olanzapine Versus Divalproex Sodium for the Treatment of Acute Mania and Maintenance of Remission: a 47-Week Study
Article Olanzapine Versus Divalproex Sodium for the Treatment of Acute Mania and Maintenance of Remission: A 47-Week Study Mauricio Tohen, M.D., Dr.P.H. Objective: Few double-blind trials have was significantly greater for the olanzapine compared longer-term efficacy and safety group. Median time to symptomatic ma- Terence A. Ketter, M.D. of medications for bipolar disorder. The nia remission was significantly shorter for authors report a 47-week comparison of olanzapine, 14 days, than for divalproex, olanzapine and divalproex. 62 days. There were no significant differ- Carlos A. Zarate, M.D. Method: This 47-week, randomized, ences between treatments in the rates of double-blind study compared flexibly symptomatic mania remission over the 47 Trisha Suppes, M.D., Ph.D. dosed olanzapine (5–20 mg/day) to dival- weeks (56.8% and 45.5%, respectively) and proex (500–2500 mg/day) for manic or subsequent relapse into mania or depres- Mark Frye, M.D. mixed episodes of bipolar disorder (N= sion (42.3% and 56.5%). Treatment-emer- 251). The only other psychoactive medi- gent adverse events occurring significantly Lori Altshuler, M.D. cation allowed was lorazepam for agita- more frequently during olanzapine treat- tion. The primary efficacy instrument was ment were somnolence, dry mouth, in- the Young Mania Rating Scale; a priori creased appetite, weight gain, akathisia, John Zajecka, M.D. protocol-defined threshold scores were and high alanine aminotransferase levels; ≥20 for inclusion, ≤12 for remission, and those for divalproex were nausea and ≥15 for relapse. Analytical techniques in- Leslie M. Schuh, Ph.D. -

Obituary Johan Schioldann
Obituary Johan Schioldann To cite this version: Johan Schioldann. Obituary. History of Psychiatry, SAGE Publications, 2006, 17 (2), pp.247-252. 10.1177/0957154X06061602. hal-00570850 HAL Id: hal-00570850 https://hal.archives-ouvertes.fr/hal-00570850 Submitted on 1 Mar 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. HPY 17(2) Schou obituary 2/5/06 09:21 Page 1 History of Psychiatry, 17(2): 247–252 Copyright © 2006 SAGE Publications (London, Thousand Oaks, CA and New Delhi) www.sagepublications.com [200606] DOI: 10.1177/0957154X06061602 Obituary Mogens Abelin Schou (1918–2005) – half a century with lithium JOHAN SCHIOLDANN* Mogens Schou, the most prominent of the pioneers of modern lithium therapy, passed away on 29 September 2005. He was 86 years old. A couple of days before, he had returned home from an IGSLI (International Group for the Study of Lithium-Treated Patients) meeting in Poland. He succumbed to pneumonia, having managed to finish a last manuscript just hours before. Schou was born in Copenhagen in 1918. His father, Hans Jacob Schou, an influential figure in Danish psychiatry, adopted the notion of a biological basis of affective disorders from his countryman, Carl Lange, one of the early era lithium pioneers (Schioldann, 2001), and established a research laboratory to study the possible biochemical and physiological changes in manic-depressive illness (Schou, 2005). -

Pharmacology and Toxicology of Amphetamine and Related Designer Drugs
Pharmacology and Toxicology of Amphetamine and Related Designer Drugs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Pharmacology and Toxicology of Amphetamine and Related Designer Drugs Editors: Khursheed Asghar, Ph.D. Division of Preclinical Research National Institute on Drug Abuse Errol De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse NIDA Research Monograph 94 1989 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 Pharmacology and Toxicology of Amphetamine and Related Designer Drugs ACKNOWLEDGMENT This monograph is based upon papers and discussion from a technical review on pharmacology and toxicology of amphetamine and related designer drugs that took place on August 2 through 4, 1988, in Bethesda, MD. The review meeting was sponsored by the Biomedical Branch, Division of Preclinical Research, and the Addiction Research Center, National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other matieral in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. -

Mechanisms of Action of Antiepileptic Drugs
Review Mechanisms of action of antiepileptic drugs Epilepsy affects up to 1% of the general population and causes substantial disability. The management of seizures in patients with epilepsy relies heavily on antiepileptic drugs (AEDs). Phenobarbital, phenytoin, carbamazepine and valproic acid have been the primary medications used to treat epilepsy for several decades. Since 1993 several AEDs have been approved by the US FDA for use in epilepsy. The choice of the AED is based primarily on the seizure type, spectrum of clinical activity, side effect profile and patient characteristics such as age, comorbidities and concurrent medical treatments. Those AEDs with broad- spectrum activity are often found to exert an action at more than one molecular target. This article will review the proposed mechanisms of action of marketed AEDs in the US and discuss the future of AEDs in development. 1 KEYWORDS: AEDs anticonvulsant drugs antiepileptic drugs epilepsy Aaron M Cook mechanism of action seizures & Meriem K Bensalem-Owen† The therapeutic armamentarium for the treat- patients with refractory seizures. The aim of this 1UK HealthCare, 800 Rose St. H-109, ment of seizures has broadened significantly article is to discuss the past, present and future of Lexington, KY 40536-0293, USA †Author for correspondence: over the past decade [1]. Many of the newer AED pharmacology and mechanisms of action. College of Medicine, Department of anti epileptic drugs (AEDs) have clinical advan- Neurology, University of Kentucky, 800 Rose Street, Room L-455, tages over older, so-called ‘first-generation’ First-generation AEDs Lexington, KY 40536, USA AEDs in that they are more predictable in their Broadly, the mechanisms of action of AEDs can Tel.: +1 859 323 0229 Fax: +1 859 323 5943 dose–response profile and typically are associ- be categorized by their effects on the neuronal [email protected] ated with less drug–drug interactions. -

Valnoctamide and Sec-Butyl-Propylacetamide (SPD) for Acute Seizures and Status Epilepticus
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Epilepsia Manuscript Author . Author manuscript; Manuscript Author available in PMC 2018 December 17. Published in final edited form as: Epilepsia. 2013 September ; 54(Suppl 6): 99–102. doi:10.1111/epi.12290. Valnoctamide and sec-butyl-propylacetamide (SPD) for acute seizures and status epilepticus Tawfeeq Shekh-Ahmad1, Naama Hen1, John H. McDonough2, Boris Yagen1, and Meir Bialer, PhD1 1Institute for Drug Research, School of Pharmacy, Faculty of Medicine, The Hebrew University of Jerusalem, Israel 2Pharamcology Branch, Research Division, US Army Medical Research Institute of Chemical Defense (MRICD), Aberdeen Proving Ground, Maryland, USA Summary: sec-Butyl-propylacetamide (SPD) is a one-carbon homologue of valnoctamide (VCD), a chiral constitutional isomer of valproic acid’s (VPA) corresponding amide valpromide. VCD has a potential in epilepsy including status epilepticus (SE) and neuropathic pain, and is currently being developed for the treatment of bipolar disorder. Both VCD and SPD possess two stereogenic carbons in their chemical structure. SPD possess a unique and broad-spectrum antiseizure profile superior to that of VPA and better than that of VCD. In addition SPD blocked behavioral- and electrographic-SE induced by pilocarpine and soman (organophosphate nerve gas) and afforded in vivo neuroprotection that was associated with cognitive sparing. VCD has similar activity as SPD in the pilocarpine-induced-SE although at higher doses. The activity of SPD and VCD against SE is superior to that of diazepam in terms of rapid onset, potency and ability to block SE when given 20 to 60 min after seizure onset. When administered 20 and 40min after SE onset, SPD (100–174mg/kg) produced long- lasting efficacy (e.g., 4–8hr) against soman-induced convulsive- and electrographic-SE in both rats and guinea pigs. -
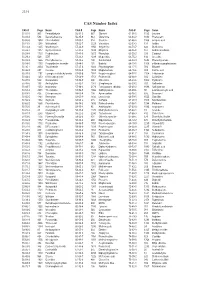
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Monoamine Depletion in Psychiatric and Healthy Populations
Molecular Psychiatry (2003) 8, 951–973 & 2003 Nature Publishing Group All rights reserved 1359-4184/03 $25.00 www.nature.com/mp FEATURE REVIEW Monoamine depletion in psychiatric and healthy populations: review L Booij1, AJW Van der Does1,2 and WJ Riedel3,4,5 1Department of Psychology, Leiden University, Leiden 2333 AK, The Netherlands; 2Department of Psychiatry, Leiden University, Leiden 2333 AK, The Netherlands; 3GlaxoSmithKline, Translational Medicine & Technology, Cambridge, UK; 4Department of Psychiatry, University of Cambridge, UK; 5Faculty of Psychology, Maastricht University, The Netherlands A number of techniques temporarily lower the functioning of monoamines: acute tryptophan depletion (ATD), alpha-methyl-para-tyrosine (AMPT) and acute phenylalanine/tyrosine deple- tion (APTD). This paper reviews the results of monoamine depletion studies in humans for the period 1966 until December 2002. The evidence suggests that all three interventions are specific, in terms of their short-term effects on one or two neurotransmitter systems, rather than on brain protein metabolism in general. The AMPT procedure is somewhat less specific, affecting both the dopamine and norepinephrine systems. The behavioral effects of ATD and AMPT are remarkably similar. Neither procedure has an immediate effect on the symptoms of depressed patients; however, both induce transient depressive symptoms in some remitted depressed patients. The magnitude of the effects, response rate and quality of response are also comparable. APTD has not been studied in recovered major depressive patients. Despite the similarities, the effects are distinctive in that ATD affects a subgroup of recently remitted patients treated with serotonergic medications, whereas AMPT affects recently remitted patients treated with noradrenergic medications. -

Antipsychotic Agents and Bipolar Disorder
Tohen and Zarate Antipsychotic Agents and Bipolar Disorder Mauricio Tohen, M.D., Dr.P.H., and Carlos A. Zarate, Jr., M.D. Antipsychotic agents have been used commonly in the treatment of bipolar disorder. This article © Copyrightreviews the evolution 1998of the use ofPhysicians antipsychotic agents andPostgraduate their role in the acute and Press, maintenance Inc. treatment of bipolar disorder. The focus is on neuroleptic drugs, the atypical antipsychotic drugs (ris- peridone and clozapine), and two of the new atypical antipsychotic drugs that were recently approved. (J Clin Psychiatry 1998;59[suppl 1]:38–48) ntipsychotic drugs have been utilized for the man- clozapine) in the treatment of bipolar disorder,4 and the A agement of patients with bipolar disorder for sev- new atypical antipsychotic drugs that have been approved eral decades. A number of alternative somatic treatments recently. approaches have been reported for patients who do not re- spond well to or who are intolerant to lithium treatment.1,2 ANTIPSYCHOTICS IN BIPOLAR DISORDER Somatic treatments other than lithiumOne reported personal to have copy a may be printed role in the management of bipolar disorder include neuro- Prior to the lithium era, the pharmacologic strategies for leptics, anticonvulsant agents (carbamazepine, valproate, bipolar disorder primarily included neuroleptics and anti- lamotrigine, gabapentin), calcium channel blockers, anti- depressants. Antipsychotic agents have been used in the depressants, cholinergic agents, adrenergic blockers, thy- treatment of bipolar disorder for close to 40 years. The use roid hormones, phototherapy, and electroconvulsive ther- of the neuroleptic drug chlorpromazine to control agitated apy.1,2 Still, in spite of all these alternatives, a proportion states was introduced by Delay and Deniker in 1952.7 Neu- of patients with bipolar disorder continue to fail or roleptic drugs then were found to be quite instrumental in be intolerant to these agents. -

The Effects of Clonidine and Idazoxan on Cerebral Blood Flow in Rats Studied by Arterial Spin Labeling Magnetic Resonance Perfusion Imaging
The Effects of Clonidine and Idazoxan on Cerebral Blood Flow in Rats Studied by Arterial Spin Labeling Magnetic Resonance Perfusion Imaging X. Du1, H. Lei1 1State Key Laboratory of Magnetic Resonance and Atomic and Molecular Physics, Wuhan Institute of Physics & Mathematics, Chinese Academy of Sciences, Wuhan, Hubei, China, People's Republic of Introduction Agonists of α2-adrenoceptors are known to produce many central and peripheral effects. For example, xylazine, a selective α2-adrenoceptors agonist, has been shown to cause region-dependent CBF decreases in rat [1]. Clonidine, an agonist for both α2-adrenergic receptor and imidazoline receptor, is a widely used drug for treating hypertension. Its effect on CBF, however, is not well understood. In this study, continuous arterial labeling (CASL) MR perfusion imaging was used to investigate the effects of clonidine and idazoxan, an antagonist for α2-adrenergic and imidazoline receptors, on CBF in rats. Materials and Methods Twelve male Sprague-Dawley rats, weighting 250-320 g, were used. After intubation, the rats were anesthetized by 1.0-1.5% isoflurane in a 70:30 N2O/O2 gas mixture. For each rat, bilateral femoral arteries and the right femoral vein were catheterized for monitoring blood gases and blood pressure, and for delivering drugs. Rectal temperature was maintained at 37.0-37.5 oC using a warm water pad. After measuring baseline CBF, the rats were divided into two groups. In the first group (n=7), clonidine (10 µg/kg, i.v.) was injected first, followed by idazoxan injection (300 µg/kg, i.v.) at 30 minutes later. Perfusion maps were obtained after administration of each drug. -

Direct-To-Consumer Ads Are Misleading: Concise Statements of Effectiveness Should Be Required
California Western School of Law CWSL Scholarly Commons Faculty Scholarship 2019 Direct-To-Consumer Ads are Misleading: Concise Statements of Effectiveness Should Be Required Robert A. Bohrer California Western School of Law, [email protected] Follow this and additional works at: https://scholarlycommons.law.cwsl.edu/fs Part of the First Amendment Commons, Food and Drug Law Commons, Health Law and Policy Commons, and the Pharmacy Administration, Policy and Regulation Commons Recommended Citation Robert A. Bohrer, Direct-To-Consumer Ads are Misleading: Concise Statements of Effectiveness Should Be Required, 22 J. Health Care L. & Pol'y 209 (2019). Available at: https://scholarlycommons.law.cwsl.edu/fs/330 This Article is brought to you for free and open access by CWSL Scholarly Commons. It has been accepted for inclusion in Faculty Scholarship by an authorized administrator of CWSL Scholarly Commons. For more information, please contact [email protected]. DIRECT-TO-CONSUMER ADS ARE MISLEADING: CONCISE STATEMENTS OF EFFECTIVENESS SHOULD BE REQUIRED ROBERT A. BOHRER, J.D., LL.M.* INTRODUCTION: THE PROBLEM WITH PHARMACEUTICAL ADVERTISING The issue of required disclaimers in direct-to-consumer (DTC) advertising of pharmaceuticals boiled to the surface in May 2019, when the Centers for Medicare and Medicaid Services (CMS) published a final rule requiring the disclosure of a drug's price in DTC ads.' The idea is not a new one-the American Medical Association (AMA) adopted a resolution recommending just such a required disclosure in June 2017.2 For a number of reasons, even if the proposal is implemented it may not have much effect.3 Consumers may see price as an indicator of effectiveness, just as a high-priced car is expected to be superior to a lower-priced car, and insurance coverage may reduce patients' C2019 Robert A.