Capabilities Performance Outcomes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
(Als) Ambulance Inventory List
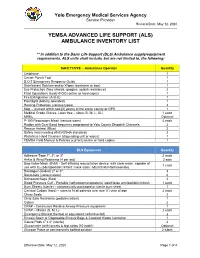
Yolo Emergency Medical Services Agency Service Provider Revised Date: May 12, 2020 YEMSA ADVANCED LIFE SUPPORT (ALS) AMBULANCE INVENTORY LIST ** In addition to the Basic Life Support (BLS) Ambulance supply/equipment requirements, ALS units shall include, but are not limited to, the following: SAFETY/PPE – Ambulance Operator Quantity Cellphone 1 Center Punch Tool 1 D.O.T Emergency Response Guide 1 Disinfectant Solution and/or Wipes (container or box) 1 Eye Protection (face shields, goggles, splash resistance) 2 Field Operations Guide (FOG) online or hard copies 1 Fire Extinguisher (A-B-C) 1 Flashlight (battery operated) 1 Hearing Protection (various types) 2 Map – (current within two [2] years) of the entire county or GPS 1 Medical Grade Gloves, Latex free – sizes (S, M, L, XL) 1 each MREs Optional P-100 Respiratory Mask (various sizes) 4 each Radios with Dual Band frequency programed to Yolo County Dispatch Channels 2 Rescue Helmet (Blue) 2 Safety Vest meeting ANSI/OSHA standards 2 Waterless Hand Cleanser (dispensing unit or wipes) 1 YEMSA Field Manual & Policies (current) online or hard copies 1 BLS Equipment Quantity Adhesive Tape 1", 2", or 3" 2 each Ankle & Wrist Restraints (4 per set) 2 sets Bag-Valve-Mask (BVM) - Self-inflating resuscitation device, with clear mask, capable of 1 each use with O2 (adult/pediatric/infant; mask sizes: adult/child/infant/neonate) Bandages (Rolled) 2" or 3" 3 Band-Aids (various sizes) 6 Biohazard Bags (Red) 2 Blood Pressure Cuff - Portable (sphygmomanometers) (adult/large arm/pediatric/infant) 1 each -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b. -

State Ambulance Policies and Services (OEI-09-95-00410; 2/98)
- - -- -------- --of -- - OFFICE OF INSPECTOR GENERAL FEBRUARY 1998 OEI-09-95-00410 EXECUTIVE SUMMARY PURPOSE To provide baseline data about the ambulance industry and determine how State and local ordinances affect the delivery of ambulance services. BACKGROUND According to Section 1861(s)(7) of Social Security Act, Medicare pays for medically necessary ambulance services when other forms of transportation would endanger the beneficiary’s health. Ambulance suppliers provide two distinct levels of service--advanced life support and basic life support. The major distinctions between the levels are the types of vehicles and the skills of the personnel and the services they render. The Health Care Financing Administration (HCFA) is considering proposed Medicare regulations that would base reimbursement for ambulance services on the patient’s condition rather than the type of vehicle and personnel used. The final rule may include a special waiver for suppliers in non-Metropolitan Statistical Areas who would be hurt financially if they use only advanced life support ambulances. The HCFA may consider several options and may include a special waiver only if HCFA is convinced through overwhelming information of the need for the waiver. We decided to examine the effect and need for a special waiver based on Metropolitan Statistical Areas and non-Metropolitan Statistical Areas. In addition, we developed baseline information on the number of ambulance suppliers, vehicles, and personnel nationwide. We conducted in-person and telephone interviews with 53 State Emergency Medical Services Directors for the 50 States, the District of Columbia, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands. Using a structured discussion guide, we (1) identified State, county, and municipal mandates that require specific levels of ambulance services and (2) obtained baseline data on the number of suppliers, licensed vehicles, and certified personnel operating within the States in 1995 and 1996. -

Collective Advanced Life Support Ambulance an Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response
Collective Advanced Life Support Ambulance An Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response Thierry Lentz SAMU 92 Charles Groizard SAMU 92 Abel Colomes SAMU 92 Anna Ozguler ( [email protected] ) INSERM https://orcid.org/0000-0002-9277-610X Michel Baer SAMU 92 Thomas Loeb SAMU 92 Research article Keywords: Emergency medical service, Critical care transport, Interhospital transfer of critically ill patients, Collective Transport, Mass casualty incidents, Disaster DOI: https://doi.org/10.21203/rs.3.rs-48425/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/14 Abstract Background: During the COVID-19 pandemic, as the number of available Intensive Care beds in France did not meet the needs, it appeared necessary to transfer a large number of patients from the most affected areas to the less ones. Mass transportation resources were deemed necessary. To achieve that goal, the concept of a Collective Advanced Life Support Ambulance (CALSA) was proposed in the form of a long-distance bus re-designed and equipped so as to accommodate up to six intensive care patients and allow Advanced Life Support (ALS) techniques to be performed while en route. Methods: The expected beneƒt of the CALSA, when compared to ALS ambulances accommodating a single patient, was to reduce the resources requirements, in particular by a lower personnel headcount for several patients being transferred to the same destination. A foreseen prospect, comparing to other collective transportation vectors such as airplanes, was the door-to-door capability, minimalizing patients’ handovers for safety concerns and time e∆ciency. -

Required ALS and BLS Equipment and Supplies
S T A T E O F H A W A I I D E P A R T M E N T O F H E A L T H ESSENTIAL EQUIPMENT and SUPPLIES FOR BASIC and ADVANCED LIFE SUPPORT Ambulance Service Standards Revised 10-14-10 ESSENTIAL EQUIPMENT FOR BASIC LIFE SUPPORT Ambulance cot w/ 3 seatbelts Sheets, linen or disp., 4 ea Cot fasteners, Floor/Wall Mount Blankets, non-synthetic, 4 ea Portable oxygen unit 360L min. tank Gauze pads, sterile, 3x3 min, 24 ea Flowmeter 0-15L/min Gauze rolls, sterile, 2" x 5 yds, 4 ea Positive pressure elder-type valve Gauze rolls, sterile 3"/4" x 5 yds, 4 ea Oxygen masks, clear, disposable, adult/pedi 1 ea Gauze rolls, sterile, 6" x 5 yds, 4 ea Oxygen nasal cannula, disposable 2 ea Triangle bandage, 40" min, 3 ea Oropharyngeal airways, adult/ped/infant 1 ea Universal dressing, 8 x 10 min, sterile, 1 ea Nasopharyngeal airways, 2 ea Tape, 1" and 2" x 5 yds, 1 ea Oxygen tanks, spare, 360L min, 2 ea Bandaids, assorted Bag-valve-mask, pedi w/02 reservoir Plastic wrap, 12" x' 12" min, 1 ea Bag-valve-mask, adult w/02 reservoir Burn sheets, sterile, 2 ea Suction, portable, battery operated Sphygmomanometer, adult, 1 ea Widebore tubing Extra large adult, 1 ea Rigid pharyngeal suction tip Pediatric, 1 ea Suction catheters 5, 10, 14, 18fr, 1 ea Stethescope, 1 ea Bite sticks (mouth gag), 2 ea Scissors, bandage, 5" min Ammonia inhalants, 3 ea Thermometer, oral and rectal, 1 ea Antiseptic swabs, 50 ea Spineboard, short, w/straps, 1 ea Bulb syringe, 3 oz. -

2016-05 REMAC Advisory ALS Medical Director
THE REGIONAL EMERGENCY MEDICAL SERVICES COUNCIL OF NEW YORK CITY, INC. NYC REMAC Advisory No. 2016-05 Title: Requirements for the Provision of Advanced Life Support Level Care, Section III: Paramedic (EMTP) Service Medical Director (Updated) Issue Date: July 1, 2016 Effective Date: July 1, 2016, Sunsets July 1, 2017 Supersedes: n/a Page: 1 of 4 The Regional Emergency Medical Advisory Committee (REMAC) of New York City is responsible to develop, approve and implement prehospital treatment and transport protocols for use within the five boroughs of the City of New York. The Regional Emergency Medical Advisory Committee (REMAC) of New York City operates under the auspices of Article 30 of the New York State Public Health Law. Requirements for Advanced Life Support Medical Director have been revised and are attached. These requirements apply to all medical directors of Advanced Life Support EMS Agencies operating in the NYC region. Medical Director Requirements are effective July 1, 2016. These requirements will be assessed when ALS Agency recertifies. Agency will be responsible to provide all information needed. Any agency renewing after July 1, 2016 must meet new standards, with a sunset date of July 1, 2017. If requirements not met, ALS agency will receive a 30-day warning letter, then suspension. Current and Updated Protocols can be accessed at the Regional EMS Council website: www.nycremsco.org. Owners/operators of Ambulance and ALS First Response Services providing prehospital medical treatment within the five boroughs of the City of New York are responsible to provide copies of the NYC REMAC Prehospital Treatment Protocols to their personnel, and to ensure that Service Medical Directors and EMS personnel are informed of all changes/updates to the NYC REMAC Prehospital Treatment Protocols. -

Event Medical Flyer.Pub
EMS DETAIL PRICE LIST MedStar Vision Ambulance Crew We aspire to be a world class Mobile Healthcare Provider for ALS: $110.00 per hour with a 4 hour minimum both our customers and employees and to set standards for others to follow BLS: $100.00 per hour with a 4 hour minimum Bicycle Team $100.00 per hour with a 4 hour minimum MedStar Mission Mule Team To provide World Class Mobile Healthcare with the highest quality Customer Service and Clinical Excellence in a Fiscally ALS: $110.00 per hour with a 4 hour minimum Responsible Manner. BLS: $100.00 per hour with a 4 hour minimum First‐Aid One ALS Provider: $60.00 per hour with a 4 hour minimum One BLS Provider: $45.00 per hour with a 4 hour minimum ALS Team: $110.00 per hour with a 4 hour minimum BLS Team: $100.00 per hour with a 4 hour minimum Rodeo Team for 2 person team ALS: $110.00 per hour with a 4 hour minimum MedStar Mobile Healthcare BLS: $100.00 per hour with a 4 hour minimum 2900 Alta Mere Drive EMS Supervisor Fort Worth, TX 76116 $80.00 per hour with a 4 hour minimum Tina Marn, EMT ALS: Advanced Life Support is a set of life‐saving protocols and Special Operaons Supervisor skills that extend BLS to further support the circulaon and pro‐ Office: 817‐840‐2058 vide an open airway and adequate venlaon (breathing). MedStar Mobile Healthcare is the exclusive Cell: 817‐372‐2123 emergency and non‐emergency mobile BLS: Basic Life Support is basic First Aid and Airway management Email: [email protected] healthcare provider to Fort Worth and 14 other without the use of medicaons and advance skills and treat‐ hp://www.medstar911.org/community‐events surrounding cies including Haltom City, Bur‐ ments. -

Resolution 19-025 Backup Information Medical Director
Resolution 19-025 backup information Medical Director Scope: The City of Homer is seeking the services of a Medical Director to lead in the oversight and medical direction of the Homer Volunteer Fire Departments ALS Ambulance Service and the Homer Police Departments Emergency Medical Dispatch programs. Qualifications The medical director will be required to meet the qualifications set in 7AAC 26.630. 1. Licensed to practice in the State of Alaska 2. Participate in an orientation provided by the Fire and Police Departments. 3. Maintain an AHA ACLS certification. 4. Be an active member of SPH Medical Staff and a participant in ER Core. Responsibilities The Medical Director will be responsible for the medical direction and oversight of emergency medical services for Homer Volunteer Fire Department as stated in accordance with 7AAC 26.610 through 7aac 26.690 and 12 AAC 40.300 through 12AAC 40.390, which include, but not limited to: 1. Direct or indirect supervision of the medical care provided by each state certified ETT, EMT-1, EMT-2, EMT-3 with ACLS and Expanded Scope Procedures, MICP. Meeting any required changes under Alaska standards for EMS. 2. Conducting medical case reviews for fire department personnel on a monthly basis. (4hrs/month est.) 3. Review and participate in the quality assurance program, including a weekly review of EMS documentation w/ FD Assistant Chief. (2hrs/month est.) 4. Participate in the review and development Medical Operations Manual, standard operating procedures on an annual basis. (.5 hrs/month est.) 5. May be required to provide consultation and recommendations to the Fire Department administration regarding employee health questionnaires, fitness-for- duty assessments and return-to-work documentations. -

Emt - Paramedic
EMT - PARAMEDIC General Statement of Duties Performs basic and advanced life support, stabilization procedures, and emergency medical care at the paramedic level of training and certification and performs equipment operation duties on a twenty-four hour shift providing EMS services for the County. Distinguishing Features of the Class An employee in this class staffs the County’s EMS units, and is responsible for providing Paramedic level of emergency medical care, and providing emergency medical transport to medical facilities. Employees work a 24 hour shift and performs work including assuring that quality emergency patient care standards are in place, proper equipment and treatment are available, and sound judgment and treatment decisions are made. Work is subject to both inside and outside environmental conditions, extremes in temperatures, noise, vibrations, hazards associated with emergency medical work including exposures to fumes, odors, dusts mists, gases, poor ventilation, and oils. The worker may be required to wear a respirator at work; the employee is exposed to human blood and other bodily fluids and is subject to the OSHA requirements on blood borne pathogens. Work is performed under general supervision and is evaluated through conferences, observation, discussion of procedures at fire scenes and treatments at emergency situations, and public feedback. Duties and Responsibilities Essential Duties and Tasks Provides responses to emergency calls and ambulance requests; operates emergency medical equipment, as certified. Completes necessary records and reports for emergency calls including information for billing documentation, and legal accountability. Assists with daily cleaning and inventorying of emergency equipment, supplies, fluids, administration sets and drugs. Reports facility maintenance, radio, vehicle and equipment problems to appropriate level of authority. -

Basic Life Support 1 1.2 Advanced Life Support 5
RESUSCITATION Edited by Conor Deasy SECTION 1 1.1 Basic life support 1 1.2 Advanced life support 5 1.1 Basic life support Sameer A. Pathan compressions and rapid defibrillation, which ESSENTIALS significantly improves the chances of survival from ventricular fibrillation (VF) in OHCA.1–3 CPR 1 A patient with sudden out-of-hospital cardiac arrest (OHCA) requires activation of plus defibrillation within 3 to 5 minutes of collapse the Chain of Survival, which includes early high-quality cardiopulmonary resuscitation following VF in OHCA can produce survival rates (CPR) and early defibrillation. The emergency medical dispatcher plays a crucial and as high as 49% to 75%.5–7 Each minute of delay central role in this process. before defibrillation reduces the probability of survival to hospital discharge by 10% to 12%.2,3 2 Over telephone, the dispatcher should provide instructions for external chest The final links in the Chain of Survival are effec- compressions only CPR to any adult caller wishing to aid a victim of OHCA. This approach tive ALS and integrated post-resuscitation care has shown absolute survival benefit and improved rates of bystander CPR. targeted at optimizing and preserving cardiac 8 3 In the out-of-hospital setting, bystanders should deliver chest compressions to any and cerebral function. unresponsive patient with abnormal or absent breathing. Bystanders who are trained, able, and willing to give rescue breaths should do so without compromising the main focus on high quality of chest compressions. Development of protocols Any guidelines for BLS must be evidence based 4 Early defibrillation should be regarded as part of Basic Life Support (BLS) training, as and consistent across a wide range of providers. -

Adult Advanced Life Support: 2020 International Consensus On
Circulation Adult Advanced Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations ABSTRACT: This 2020 International Consensus on Cardiopulmonary Katherine M. Berg, MD Resuscitation and Emergency Cardiovascular Care Science With ⁝ Treatment Recommendations for advanced life support includes updates Jerry P. Nolan, MBChB on multiple advanced life support topics addressed with 3 different types On behalf of the Adult of reviews. Topics were prioritized on the basis of both recent interest Advanced Life Support within the resuscitation community and the amount of new evidence Collaborators available since any previous review. Systematic reviews addressed higher- The full author list is available on page priority topics, and included double-sequential defibrillation, intravenous S127. versus intraosseous route for drug administration during cardiac arrest, point-of-care echocardiography for intra-arrest prognostication, cardiac arrest caused by pulmonary embolism, postresuscitation oxygenation and Downloaded from http://ahajournals.org by on November 6, 2020 ventilation, prophylactic antibiotics after resuscitation, postresuscitation seizure prophylaxis and treatment, and neuroprognostication. New or updated treatment recommendations on these topics are presented. Scoping reviews were conducted for anticipatory charging and monitoring of physiological parameters during cardiopulmonary resuscitation. Topics for which systematic reviews and new Consensuses -

State Board of Health Page 1 of 185 CHAPTER 31. VIRGINIA
State Board of Health Page 1 of 185 CHAPTER 31. VIRGINIA EMERGENCY MEDICAL SERVICES REGULATIONS. PART I. GENERAL PROVISIONS. Article 1. Definitions. 12 VAC 5-31-10. Definitions. The following words and terms when used in this chapter shall have the following meanings unless the context clearly indicates otherwise. "Abandonment" means the termination of a health care provider-patient relationship without assurance that an equal or higher level of care meeting the assessed needs of the patient's condition is present and available. "Acute" means a medical condition having a rapid onset and a short duration. "Acute care hospital" means any hospital that provides emergency medical services on a 24- hour basis. "Administrative Process Act" or "APA" means Chapter 40 (§ 2.2-4000 et seq.) of Title 2.2 of the Code of Virginia. "Advanced life support" or "ALS" means the application by EMS personnel of invasive and noninvasive medical procedures or the administration of medications that is authorized by the Office of Emergency Medical Services. State Board of Health Page 2 of 185 "Advanced life support certification course" means a training program that allows a student to become eligible for a new ALS certification level. Programs must meet the educational requirements established by the Office of EMS as defined by the respective advanced life support curriculum. Initial certification courses include: 1. Emergency Medical Technician-Enhanced; 2. EMT-Enhanced to EMT-Intermediate Bridge; 3. Emergency Medical Technician-Intermediate; 4. EMT-Intermediate to EMT-Paramedic Bridge; 5. Emergency Medical Technician-Paramedic; 6. Registered Nurse to EMT-Paramedic Bridge; and 7. Other programs approved by the commissioner [Office of EMS].