Emergency Medical Services Statutes and Regulations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ambulance Helicopter Contribution to Search and Rescue in North Norway Ragnar Glomseth1, Fritz I
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Glomseth et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:109 DOI 10.1186/s13049-016-0302-8 ORIGINAL RESEARCH Open Access Ambulance helicopter contribution to search and rescue in North Norway Ragnar Glomseth1, Fritz I. Gulbrandsen2,3 and Knut Fredriksen1,4* Abstract Background: Search and rescue (SAR) operations constitute a significant proportion of Norwegian ambulance helicopter missions, and they may limit the service’s capacity for medical operations. We compared the relative contribution of the different helicopter resources using a common definition of SAR-operation in order to investigate how the SAR workload had changed over the last years. Methods: We searched the mission databases at the relevant SAR and helicopter emergency medical service (HEMS) bases and the Joint Rescue Coordination Centre (North) for helicopter-supported SAR operations within the potential operation area of the Tromsø HEMS base in 2000–2010. We defined SAR operations as missions over land or sea within 10 nautical miles from the coast with an initial search phase, missions with use of rescue hoist or static rope, and avalanche operations. Results: There were 769 requests in 639 different SAR operations, and 600 missions were completed. The number increased during the study period, from 46 in 2000 to 77 in 2010. The Tromsø HEMS contributed with the highest number of missions and experienced the largest increase, from 10 % of the operations in 2000 to 50 % in 2010. Simple terrain and sea operations dominated, and avalanches accounted for as many as 12 % of all missions. -

National Ems Scope of Practice Model 2019
NATIONAL EMS SCOPE OF PRACTICE MODEL 2019 The National Highway Traffic Safety Administration Education Credentialing Certification Licensure NHTSA III.NA110NAL -•w•• TRAPPIC u,n, ••-•nunoN DISCLAIMER This publication is distributed by the U.S. Department of Transportation, National Highway Traffic Safety Administration, in the interest of information exchange. The opinions, findings, and conclusions expressed in this publication are those of the authors and not necessarily those of the Department of Transportation or the National Highway Traffic Safety Administration. The United States Government assumes no liability for its contents or use thereof. If trade or manufacturers’ names or products are mentioned, it is because they are considered essential to the object of the publications and should not be construed as an endorsement. The United States Government does not endorse products or manufacturers. Suggested APA Format Citation: National Association of State EMS Officials. National EMS Scope of Practice Model 2019 (Report No. DOT HS 812-666). Washington, DC: National Highway Traffic Safety Administration. The National EMS Scope of Practice Model February 2019 Technical Report Documentation Page 1. Report No. 2. Government Accession No. 3. Recipient’s Catalog No. DOT HS 812 666 4. Title and Subtitle 5. Report Date National EMS Scope of Practice Model 2019 February 2019 6. Performing Organization Code 7. Author(s) 8. Performing Organization Report No. National Association of State EMS Officials DOT-VNTSC-NHTSA-812-666 9. Performing Organization Name and Address 10. Work Unit No. (TRAIS) National Association of State EMS Officials 201 Park Washington Court 11. Contract or Grant No. Falls Church, VA 22046-4527 12. -

Iowa Emergency Medical Care Provider Scope of Practice
Iowa Department of Public Health Bureau of Emergency and Trauma Services Iowa Emergency Medical Care Provider Scope of Practice October 2019 “Protecting and Improving the Health of Iowans” LUCAS STATE OFFICE BUILDING 321 East 12th Street DES MOINES, IOWA 50319-0075 (515) 281-0620 (800) 728-3367 https://idph.iowa.gov/BETS/EMS Scope of Practice – Defined parameters of various duties or services that may be provided by an individual with specific credentials. Whether regulated by rule, statute, or court decision, it represents the limits of services an individual may legally perform. Contents Introduction ....................................................................................................................... 2 Background ....................................................................................................................... 2 Overview of the EMS Profession ................................................................................... 2 The Evolution of the EMS Agenda for the Future .......................................................... 4 National EMS Educational Standards ............................................................................. 5 Interdependent Relationship Between Education, Certification, Licensure, and Credentialing ..................................................................................................................... 7 Medical Supervision.......................................................................................................... 8 Pilot Project ...................................................................................................................... -

Helicopter EMS (HEMS) Programs in the United States Were Largely Not-For-Profit Hospital Or Public Safety Operations Until the Late 1990’S
National Association of State EMS Officials – Air Medical Services Committee Brief Outline of the Federal Pre-emption Issues in Regulating Air Medical Services October, 2011 Helicopter EMS (HEMS) programs in the United States were largely not-for-profit hospital or public safety operations until the late 1990’s. These programs were generally well integrated with state and local EMS system. An increase in Medicare reimbursement for air ambulance transports in the early 2000’s appears to have contributed to a significant increase in the number of HEMS programs, medical helicopters, and for-profit operators. The number of air medical transports doubled between 2000 and 2010. The number of helicopter crashes increased as well, drawing public and National Transportation Safety Board attention to the issue. Some for-profit operators use aggressive tactics and marketing to increase flights. Unlike passengers who choose an air carrier to use on a vacation or business trip, patients typically have little or no say in what service is utilized to transport them by air ambulance. As states have attempted to regulate HEMS programs and ensure their integration with state and local EMS systems, operators have responded with lawsuits asserting the exclusive authority of the Federal Aviation Administration under the Airline Deregulation Act (PL 95-504) of 1978 (ADA). The ADA pre-empts states from regulating the rates, routes, or services of an air carrier. When Congress passed the ADA, there were very few HEMS programs in the United States, and it is doubtful that there was any consideration of the impact of the ADA on the regulation of air ambulances by states. -
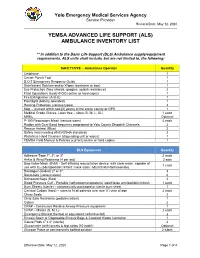
(Als) Ambulance Inventory List
Yolo Emergency Medical Services Agency Service Provider Revised Date: May 12, 2020 YEMSA ADVANCED LIFE SUPPORT (ALS) AMBULANCE INVENTORY LIST ** In addition to the Basic Life Support (BLS) Ambulance supply/equipment requirements, ALS units shall include, but are not limited to, the following: SAFETY/PPE – Ambulance Operator Quantity Cellphone 1 Center Punch Tool 1 D.O.T Emergency Response Guide 1 Disinfectant Solution and/or Wipes (container or box) 1 Eye Protection (face shields, goggles, splash resistance) 2 Field Operations Guide (FOG) online or hard copies 1 Fire Extinguisher (A-B-C) 1 Flashlight (battery operated) 1 Hearing Protection (various types) 2 Map – (current within two [2] years) of the entire county or GPS 1 Medical Grade Gloves, Latex free – sizes (S, M, L, XL) 1 each MREs Optional P-100 Respiratory Mask (various sizes) 4 each Radios with Dual Band frequency programed to Yolo County Dispatch Channels 2 Rescue Helmet (Blue) 2 Safety Vest meeting ANSI/OSHA standards 2 Waterless Hand Cleanser (dispensing unit or wipes) 1 YEMSA Field Manual & Policies (current) online or hard copies 1 BLS Equipment Quantity Adhesive Tape 1", 2", or 3" 2 each Ankle & Wrist Restraints (4 per set) 2 sets Bag-Valve-Mask (BVM) - Self-inflating resuscitation device, with clear mask, capable of 1 each use with O2 (adult/pediatric/infant; mask sizes: adult/child/infant/neonate) Bandages (Rolled) 2" or 3" 3 Band-Aids (various sizes) 6 Biohazard Bags (Red) 2 Blood Pressure Cuff - Portable (sphygmomanometers) (adult/large arm/pediatric/infant) 1 each -

Understanding Code Status
Understanding Code Status It’s important to consider the type of Code status conversations should include questions such as: medical treatments you want before • Which treatments, if any, might you not want to a medical emergency occurs. All receive? patients must choose a code status. • Under which circumstances, if any, do you believe life-prolonging treatments would not be desirable? Understanding what each code means • How has your past experience, if any, created your and selecting a code status will help opinion about resuscitation procedures for yourself? your caregivers and loved ones follow It is very important to have this discussion your wishes. before a medical emergency occurs. What is Code Status? Choosing your Code Status All patients who are admitted to a hospital or an You will work with your health care provider to outpatient facility (such as a dialysis center or discuss the types of resuscitation procedures and outpatient surgery center) will be asked to choose advance medical treatments you would benefit from a code status for the duration of their stay. and the type that you may not want if a medical emergency were to occur. This conversation should Your chosen code status describes the type of help you determine which code status is right for you resuscitation procedures (if any) you would like the to live well with your goals in mind. health care team to conduct if your heart stopped beating and/or you stopped breathing. During this Outcomes after CPR medical emergency, resuscitation procedures must Unfortunately, what you see on TV is not reality. -

Healthy Choices Get a Head Start on Great Health
Healthy Choices Get a Head Start on Great Health 2015 Benefits Guide MedStar Georgetown University Hospital, Non-union MedStar Health Research Institute MedStar National Rehabilitation Network Non-hospital Based Businesses, South Table of Contents 1 Enrollment Checklist 2 Enrollment Guidelines 3 Online Enrollment Instructions 4 Wellness Resources 4 Your Medical Plan Options 5 COBRA Continued Benefit Coverage 6 2015 Medical Plan Options Chart 8 Prescription Drug Plans 9 Your Dental Plan Options 11 Your Vision Plan Option 12 Flexible Spending Accounts (FSAs) 14 Life Insurance 14 Accidental Death and Dismemberment Insurance 15 Disability Plans 15 Universal Life, Critical Illness and Accident Insurances 16 Legal Resources 16 MedStar Associate Advantages 18 Contact Information i 2015 Annual Enrollment Choices For Healthy Living MedStar Health provides a comprehensive benefits If you are a benefit-eligible associate, take advantage of package for you and your family—MedStar Total MedStar Total Rewards. You must enroll online to receive Rewards. You are responsible for selecting the best mix medical, dental, vision, flexible spending accounts, of benefits to meet your needs and actively managing supplemental life, supplemental accidental death and these benefits and your health throughout the year. Use dismemberment, dependent life, or legal coverage in 2015. this guide to select your MedStar Total Rewards health and welfare package for 2015. Enrollment Checklist Read through this guide to design your MedStar Total Rewards package for 2015. Medical Accidental Death and Dismemberment Elect a healthcare coverage option. Insurance • MedStar Select Plan Consider if additional coverage would give your • CareFirst BlueCross BlueShield Preferred family more peace of mind. Provider Organization (PPO) Plan • Kaiser Permanente Health Maintenance Disability Organization (HMO) Plan MedStar provides full-time associates with short- and long-term disability coverage equal to 60 Dental percent of your base pay, at no cost to you. -
JNR0120SE Globalprofile.Pdf
JOURNAL OF NURSING REGULATION VOLUME 10 · SPECIAL ISSUE · JANUARY 2020 THE OFFICIAL JOURNAL OF THE NATIONAL COUNCIL OF STATE BOARDS OF NURSING JOURNAL Volume 10 Volume OF • Special Issue Issue Special NURSING • January 2020 January REGULATION Advancing Nursing Excellence for Public Protection A Global Profile of Nursing Regulation, Education, and Practice National Council of State Boards of Nursing Pages 1–116 Pages JOURNAL OFNURSING REGULATION Official publication of the National Council of State Boards of Nursing Editor-in-Chief Editorial Advisory Board Maryann Alexander, PhD, RN, FAAN Mohammed Arsiwala, MD MT Meadows, DNP, RN, MS, MBA Chief Officer, Nursing Regulation President Director of Professional Practice, AONE National Council of State Boards of Nursing Michigan Urgent Care Executive Director, AONE Foundation Chicago, Illinois Livonia, Michigan Chicago, Illinois Chief Executive Officer Kathy Bettinardi-Angres, Paula R. Meyer, MSN, RN David C. Benton, RGN, PhD, FFNF, FRCN, APN-BC, MS, RN, CADC Executive Director FAAN Professional Assessment Coordinator, Washington State Department of Research Editors Positive Sobriety Institute Health Nursing Care Quality Allison Squires, PhD, RN, FAAN Adjunct Faculty, Rush University Assurance Commission Brendan Martin, PhD Department of Nursing Olympia, Washington Chicago, Illinois NCSBN Board of Directors Barbara Morvant, MN, RN President Shirley A. Brekken, MS, RN, FAAN Regulatory Policy Consultant Julia George, MSN, RN, FRE Executive Director Baton Rouge, Louisiana President-elect Minnesota Board of Nursing Jim Cleghorn, MA Minneapolis, Minnesota Ann L. O’Sullivan, PhD, CRNP, FAAN Treasurer Professor of Primary Care Nursing Adrian Guerrero, CPM Nancy J. Brent, MS, JD, RN Dr. Hildegarde Reynolds Endowed Term Area I Director Attorney At Law Professor of Primary Care Nursing Cynthia LaBonde, MN, RN Wilmette, Illinois University of Pennsylvania Area II Director Philadelphia, Pennsylvania Lori Scheidt, MBA-HCM Sean Clarke, RN, PhD, FAAN Area III Director Executive Vice Dean and Professor Pamela J. -

Cardiopulmonary Resuscitation EFFECTIVE DATE: October 2007 SUPERCEDES DATE: May 2004
HEALTH SERVICES POLICY & PROCEDURE MANUAL North Carolina Department Of Correction SECTION: Care and Treatment of Patient Division Of Prisons POLICY # TX I-7 PAGE 1 of 3 SUBJECT: Cardiopulmonary Resuscitation EFFECTIVE DATE: October 2007 SUPERCEDES DATE: May 2004 PURPOSE To provide guidelines in case of a medical emergency requiring Cardiopulmonary Resuscitation (CPR). To re-establish effective ventilation and circulation. To prevent irreversible brain damage. To provide an efficient and organized team approach in response to a medical emergency requiring Cardiopulmonary Resuscitation (CPR). To delineate the responsibilities of staff in the event of a medical emergency requiring Cardiopulmonary Resuscitation (CPR). POLICY All Health Services personnel will be certified in Cardiopulmonary Resuscitation (CPR) including Automated External Defibrillator (AED) according to guidelines set forth by the American Heart Association (AHA) “Basic Life Support Health Care Provider Course” (BLS-HCP). It is the responsibility of the employee to maintain current BLS-HCP CPR certification, with renewal every two years. Dental hygienists are required to renew annually per professional standards. Failure to recertify may result in the disciplinary process being initiated. Custody Officers are trained to provide CPR according to guidelines set forth by the American Heart Association “HeartSaver-AED Course”. Cardiopulmonary Resuscitation will be initiated on all patients demonstrating cardiac and/or respiratory arrest (i.e., absence of spontaneous respirations and/or pulseless), with the exception of: a. Decapitation b. Body tissue decomposition noted c. Verification of a current Do Not Resuscitate (DNR) order originated or approved by a physician in the employ of N.C. Division of Prisons. (1) Most patients with current DNR orders will be maintained in a Hospice unit, health ward, or infirmary with DNR located in patient’s chart with staff knowledge of such. -

JOURNAL of Health & Life Sciences
Journal of Health & Life Sciences Law VOLUME 4, NUMBER 2 FEBRUARY 2011 TABLE OF Meet the Fraud Busters: Program Safeguard Contractors CO N TE N TS and Zone Program Integrity Contractors ................................. 1 by Sara Kay Wheeler, Stephanie L. Fuller, and J. Austin Broussard The Link Between Quality and Medical Management: Physician Tiering and Other Initiatives .................................. 36 by Rakel Meir and Paul W. Shaw Medical Control of Emergency Medical Services .................. 65 by Rick L. Hindmand and W. Ann Maggiore Quality in Action: Paradigm for a Hospital Board- Driven Quality Program .......................................................... 95 by Elisabeth Belmont, Claire Cowart Haltom, Douglas A. Hastings, Robert G. Homchick, Lewis Morris, Robin Locke Nagele, Kathryn C. Peisert, Brian M. Peters, Beth Schermer, and Julie Taitsman NOTES A N D The Employee Exceptions to the Anti-Kickback and COMME N TS Stark Laws After Tuomey: What’s a Physician’s Employer To Do? ..................................................................... 146 by Susan O. Scheutzow and Steven A. Eisenberg PRACTICE Data Privacy Concerns for U.S. Healthcare RESOURCE Enterprises’ Overseas Ventures ............................................. 173 by Vadim Schick Journal of Health & Life Sciences Law 65 Medical Control of Emergency Medical Services Rick L. Hindmand and W. Ann Maggiore ABSTRACT: Effective medical control by medical directors and other medical oversight professionals is an essential element in providing appropri- ate emergency medical services (EMS). Within an EMS system, EMS medical directors have a supervisory rather than agency relationship with the emer- gency medical technicians (EMTs). Contrary to some commentary on the legal framework of this relationship, EMTs do not practice “under the license” of the medical director, but instead practice pursuant to their own state or county licenses, which generally require physician supervision. -

VHA Dir 1101.05(2), Emergency Medicine
Department of Veterans Affairs VHA DIRECTIVE 1101.05(2) Veterans Health Administration Transmittal Sheet Washington, DC 20420 September 2, 2016 EMERGENCY MEDICINE 1. REASON FOR ISSUE: This Veterans Health Administration (VHA) directive establishes policy and procedures for VHA Emergency Departments (EDs) and Urgent Care Centers (UCCs). 2. SUMMARY OF MAJOR CHANGES: This directive replaces the previous VHA handbook establishing procedures for VA EDs and UCCs. The following major changes are included: a. Information on EDs, UCCs, diversion, Mental Health, sexual assault, temporary beds, ED/UCC staffing, and Emergency Department Integration Software (EDIS) was added. b. Information about the Intermediate Healthcare Technician Program. c. Information about the ED and Women’s Health, Out of Operating Room Airway Management and Ensuring Correct Surgery and Invasive Procedures, and geriatric emergency care. d. Information about the Emergency Medicine Improvement Initiative and support resources. 3. RELATED ISSUE: None. 4. RESPONSIBLE OFFICE: The Office of Patient Care Services (10P), Specialty Care Services (10P4E), is responsible for the content of this VHA Handbook. Questions may be referred to the National Director for Emergency Medicine at 202-461-7120. 5. RESCISSIONS: VHA Handbook 1101.05, dated May 12, 2010; VHA Directive 1051, dated February 21, 2014; VHA Directive 1079, dated February 3, 2014; VHA Directive 2010-008, dated February 22, 2010; VHA Directive 2010-014, dated March 25, 2010; VHA Directive 1009, dated August 28, 2013; VHA Directive 2010-010, dated March 2, 2010; VHA Directive 2011-029, dated July 15, 2011; and VHA Directive 2009-069, dated December 16, 2009 are rescinded. 6. RECERTIFICATION: This VHA directive is scheduled for recertification on or before the last working day of September 2021. -

Medical Emergency Minimum Standard: 5120:1-8-09(E) Revised
Section 6: Jail Emergencies Response Plan Subject: Medical Emergency Minimum Standard: 5120:1-8-09(E) Revised: Authorized: _____________________________ Effective date: ________________________ Sheriff Paul A. Sigsworth POLICY The Erie County Jail shall provide 24-hour emergency medical, dental, and mental health care services. All corrections officers are trained to respond to medical emergencies, and will promptly implement emergency medical procedures for inmates who are in need of emergency medical attention. PROCEDURE A. Policy 1. Any Corrections Officer or member of the Medical Staff who is available will respond when a Medical Emergency is reported and initiate care. B. Definitions: 1. The following occurrence define an emergency, which may result from, but not limited to, injury from attempted suicide or injury from assault. a. Sever Bleeding: i. Apply clean/sterile pressure dressing to wound, apply pressure by use of hands. Monitor for signs and symptoms of shock. Follow American Red Cross Heartsaver Guidelines. b. Unconsciousness: i. Maintain body alignment, observe vital signs, respiration, etc., for any change until the doctor or emergency squad arrives. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. c. Serious Breathing Difficulties: i. Keep in a semi-sitting position. Loosen or remove all tight clothing, observe and reassure. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. d. Head, Neck, and/or Spinal Injury: i. Keep inmate quiet. Stop any bleeding, maintain neck alignment, observe and reassure. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. e. Severe Burns: i. Do not remove clothing. Apply clean wet dressing to area. Prevent chilling, observe and reassure.