DHS-Wide EMS Basic Life Support (BLS) & Advanced Life Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First Aid 10/18/07 1:23 PM Page 1
FINAL CATALOGUE -First Aid 10/18/07 1:23 PM Page 1 Regulation FirstFirst Aid Aid Kits by SAFECROSS OCCUPATIONAL HEALTH AND SAFETY REGULATION FIRST AID KITS Regulation first aid kits meet regulations required by Federal, Provincial and Territorial jurisdictions. Regulations change on a continuing basis. Requirements vary from jurisdiction to jurisdiction and are ALBERTA FIRST AID KITS dependent on a number of factors including (but not limited to): • maximum number of employees at the work site (or per shift) http://www.gov.ab.ca/ • location of the place of employment/industry • type of industry and potential hazards • proximity or travel time to a medical facility FEDERAL REGULATION FIRST AID KITS Common federal employers include the following interprovincial and international industries: • Banks • Railways, highway and air transport No. 1 • Ferries, tunnels, bridges and canals FAP 50100 16 unit Plastic with gasket • Telephone and telegraph systems FAP 50103 16 unit Metal • Pipelines FAP 50109B Soft Pack # 16 • Radio and television broadcasting and cable systems • Shipping and shipping services No. 2 • Employment in the operation of ships, trains and aircraft FAP 50124 36 unit Plastic with gasket • Licensed grain elevators, and certain feed mills and feed warehouses, flour mills and grain seed clearing plants FAP 50127 36 unit Metal • Federal public service and persons employed by the public service and Crown corporations and agencies FAP 50133B Soft Pack # 24 • Indian reserves • Exploration and development of petroleum on lands subject to federal jurisdiction No. 3 FAP 50140 # 2 Plastic with gasket FAP 50139 # 2 Metal FAP 50142B Soft Pack Mini Trauma Bag FEDERAL FIRST AID KITS BRITISH COLUMBIA FIRST AID KITS Item required but not included in all kits: accident record book. -

FIRST AID PRODUCTS HEADQUARTERS USA Toll Free Tel: 800-430-4110
NORTH-21456 First Aid Cover_Re 5/21/09 2:37 PM Page 1 Distributed by: www.northsafety.com GLOBAL FIRST AID PRODUCTS HEADQUARTERS USA Toll Free Tel: 800-430-4110 CANADA MONTREAL Toll Free Tel: 1-888-212-SAFE (7233) TORONTO Toll Free Tel: 1-888-316-SAFE (7233) EDMONTON Toll Free Tel: 1-800-661-3638 EUROPE THE NETHERLANDS Tel: +31(0)118 656400 LATIN AMERICA Tel: 1-954-322-1691 ASIA & PACIFIC Tel: 61-3-9337-9111 CHINA Tel: 86-10-67892289/90/91 Trademarks: Redi-Care First Aid Kits™ is a trademark of North by Honeywell; CPR Filtershield™, CPR Microkey™ and Microholster™, are trademarks of Medical Devices International; CPR Microshield is a registered trade- mark of Medical Devices International; Burn Jel®, Cool Jel® and Water Jel® are registered trademarks of Water-Jel Technologies; Bug X™ and Ivy X™ is a trademark of ISIS Investment Inc.; SunX® is a registered trademark of CoreTex Products; Band-Aid® is a registered trademark of Johnson & Johnson; Curad® is a registered trademark of Tyco International; Neosporin® is a registered trademark of Pfizer Consumer Healthcare; Vital 1® is a registered trademark of OBF. 2009 North by Honeywell • Printed in USA PRINTER CODE FACA09XXEUOOOO Table of Contents Stations . .pgs 5-11 CPR Products . .pgs 64-66 First Aid Kits . .pgs 12-17 Outdoor Protection . .pgs 67-71 First Aid Kits, Specialty . .pgs 18-32 Burn Care . .pgs 72-79 First Response . .pgs 33-39 Medicinals . .pgs 80-83 Wound Care . .pgs 40-53 Emergency Preparedness . .pgs 84-89 Eye Care . .pgs 54-57 Miscellaneous First Aid Supplies . -

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

NIMS 508 Stillwater Flood Search and Rescue Team
Resource Typing Definition for Response Mass Search and Rescue Operations STILLWATER/FLOOD SEARCH AND RESCUE TEAM DESCRIPTION The Stillwater/Flood Search and Rescue (SAR) Team conducts search, rescue, and recovery operations for humans and animals in stillwater and stillwater/flood environments RESOURCE CATEGORY Search and Rescue RESOURCE KIND Team OVERALL FUNCTION The Stillwater/Flood SAR team: 1. Searches for and rescues individuals who may be injured or otherwise in need of medical attention 2. Provides emergency medical care, including Basic Life Support (BLS) 3. Provides animal rescue 4. Transports humans and animals to the nearest location for secondary land or air transport 5. Provides shore-based and boat-based water rescue for humans and animals 6. Supports helicopter rescue operations and urban SAR in water environments for humans and animals 7. Operates in environments with or without infrastructure, including environments with disrupted access to roadways, utilities, transportation, and medical facilities, and with limited access to shelter, food, and water COMPOSITION AND ORDERING 1. Requestor and provider address certain needs and issues prior to deployment, including: SPECIFICATIONS a. Communications equipment that enables more than intra-team communications, such as programmable interoperable communications equipment with capabilities for command, logistics, military, air, and so on b. Type of incident and operational environment, such as weather event, levy or dam breach, or risk of hazardous materials (HAZMAT) contamination c. Additional specialized personnel, such as advanced medical staff, animal SAR specialists, logistics specialists, advisors, helicopter support staff, or support personnel for unique operating environments d. Additional transportation-related needs, including specific vehicles, boats, trailers, drivers, mechanics, equipment, supplies, fuel, and so on e. -
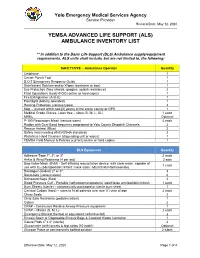
(Als) Ambulance Inventory List
Yolo Emergency Medical Services Agency Service Provider Revised Date: May 12, 2020 YEMSA ADVANCED LIFE SUPPORT (ALS) AMBULANCE INVENTORY LIST ** In addition to the Basic Life Support (BLS) Ambulance supply/equipment requirements, ALS units shall include, but are not limited to, the following: SAFETY/PPE – Ambulance Operator Quantity Cellphone 1 Center Punch Tool 1 D.O.T Emergency Response Guide 1 Disinfectant Solution and/or Wipes (container or box) 1 Eye Protection (face shields, goggles, splash resistance) 2 Field Operations Guide (FOG) online or hard copies 1 Fire Extinguisher (A-B-C) 1 Flashlight (battery operated) 1 Hearing Protection (various types) 2 Map – (current within two [2] years) of the entire county or GPS 1 Medical Grade Gloves, Latex free – sizes (S, M, L, XL) 1 each MREs Optional P-100 Respiratory Mask (various sizes) 4 each Radios with Dual Band frequency programed to Yolo County Dispatch Channels 2 Rescue Helmet (Blue) 2 Safety Vest meeting ANSI/OSHA standards 2 Waterless Hand Cleanser (dispensing unit or wipes) 1 YEMSA Field Manual & Policies (current) online or hard copies 1 BLS Equipment Quantity Adhesive Tape 1", 2", or 3" 2 each Ankle & Wrist Restraints (4 per set) 2 sets Bag-Valve-Mask (BVM) - Self-inflating resuscitation device, with clear mask, capable of 1 each use with O2 (adult/pediatric/infant; mask sizes: adult/child/infant/neonate) Bandages (Rolled) 2" or 3" 3 Band-Aids (various sizes) 6 Biohazard Bags (Red) 2 Blood Pressure Cuff - Portable (sphygmomanometers) (adult/large arm/pediatric/infant) 1 each -

Basic Life Support Health Care Provider
ELLIS & ASSOCIATES Health Care Provider Basic Life Support MEETS CURRENT CPR & ECC GUIDELINES Ellis & Associates / Safety & Health HEALTH CARE PROVIDER BASIC LIFE SUPPORT - I Ellis & Associates, Inc. P.O. Box 2160, Windermere, FL 34786-2160 www.jellis.com Copyright © 2016 by Ellis & Associates, LLC All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Ellis & Associates P.O. Box 2160, Windermere, FL 34786-2160 Ordering Information: Quantity sales. Special discounts are available on quantity purchases by corporations, associations, trade bookstores and wholesalers. For details, contact the publisher at the address above. Disclaimer: The procedures and protocols presented in this manual and the course are based on the most current recommendations of responsible medical sources, including the International Liaison Committee on Resuscitation (ILCOR) 2015 Guidelines for CPR & ECC. Ellis & Associates, however, make no guarantee as to, and assume no responsibility for, the correctness, sufficiency, or completeness of such recommendations or information. Additional procedures may be required under particular circumstances. Ellis & Associates disclaims all liability for damages of any kind arising from the use of, reference to, reliance on, or performance based on such information. Library of Congress Cataloging-in-Publication Data Not Available at Time of Printing ISBN 978-0-9961108-0-8 Unless otherwise indicated on the Credits Page, all photographs and illustrations are copyright protected by Ellis & Associates. -

First Aid Supplies
01/25/2019 First Aid Supplies Page: 1 Bid Opening: 12/20/2018 Period Range: 02/01/2019 - 01/31/2020 Supplies Catalog (By Category) Awarded Vendors Sub Classification: Dental Description/Brand/Alternative/Variance Unit Price Vendor Awarded 11001 Treasure Chest - Small Plastic PACK $7.3600 139 1 / 2019 (to place baby tooth in) School Health Corp. 144/pkg MacGill-4739 90404 11002 Toothsaver Necklace PACKAGE $9.6000 139 1 / 2019 (to place baby teeth in) School Health Corp. 144/pkg 90246/SMILEMAKERS 11004 EMT Tooth Saver EACH $10.2800 282 1 / 2019 (emergency medical treatment) Medco Supply Company 7883139 47013M 11008 Tooth Brushes-Child Size PACK $0.2300 282 1 / 2019 12/pk Medco Supply Company New World 6358366 18601M X 12, SOLD & PRICED PER EACH 11012 Toothbrushes PACK $8.9900 139 1 / 2019 Child Size School Health Corp. 144/pkg 853396 47037/GENERIC 11015 Toothbrush - Adult BOX $10.0800 139 1 / 2019 30 - Tuft Nylon School Health Corp. 144/Box New World 1202562 47038/GENERIC 11019 Ora-Jel EACH $5.9200 139 1 / 2019 .25 oz tube School Health Corp. 43155/ORAJEL 01/25/2019 First Aid Supplies Page: 2 Bid Opening: 12/20/2018 Period Range: 02/01/2019 - 01/31/2020 Supplies Catalog (By Category) Awarded Vendors Sub Classification: Dental Description/Brand/Alternative/Variance Unit Price Vendor Awarded 11023 Anbesol EACH $4.6000 282 1 / 2019 .41 oz. tube Medco Supply Company Alcohol free 00037 11024 Den Tek Comfort Clean Floss Picks PACKAGE $32.1200 139 1 / 2019 Slides easily, advanced flouride coating School Health Corp. -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b. -

State Ambulance Policies and Services (OEI-09-95-00410; 2/98)
- - -- -------- --of -- - OFFICE OF INSPECTOR GENERAL FEBRUARY 1998 OEI-09-95-00410 EXECUTIVE SUMMARY PURPOSE To provide baseline data about the ambulance industry and determine how State and local ordinances affect the delivery of ambulance services. BACKGROUND According to Section 1861(s)(7) of Social Security Act, Medicare pays for medically necessary ambulance services when other forms of transportation would endanger the beneficiary’s health. Ambulance suppliers provide two distinct levels of service--advanced life support and basic life support. The major distinctions between the levels are the types of vehicles and the skills of the personnel and the services they render. The Health Care Financing Administration (HCFA) is considering proposed Medicare regulations that would base reimbursement for ambulance services on the patient’s condition rather than the type of vehicle and personnel used. The final rule may include a special waiver for suppliers in non-Metropolitan Statistical Areas who would be hurt financially if they use only advanced life support ambulances. The HCFA may consider several options and may include a special waiver only if HCFA is convinced through overwhelming information of the need for the waiver. We decided to examine the effect and need for a special waiver based on Metropolitan Statistical Areas and non-Metropolitan Statistical Areas. In addition, we developed baseline information on the number of ambulance suppliers, vehicles, and personnel nationwide. We conducted in-person and telephone interviews with 53 State Emergency Medical Services Directors for the 50 States, the District of Columbia, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands. Using a structured discussion guide, we (1) identified State, county, and municipal mandates that require specific levels of ambulance services and (2) obtained baseline data on the number of suppliers, licensed vehicles, and certified personnel operating within the States in 1995 and 1996. -

Collective Advanced Life Support Ambulance an Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response
Collective Advanced Life Support Ambulance An Innovative Transportation of Critical Care Patients by Bus in COVID-19 Pandemic Response Thierry Lentz SAMU 92 Charles Groizard SAMU 92 Abel Colomes SAMU 92 Anna Ozguler ( [email protected] ) INSERM https://orcid.org/0000-0002-9277-610X Michel Baer SAMU 92 Thomas Loeb SAMU 92 Research article Keywords: Emergency medical service, Critical care transport, Interhospital transfer of critically ill patients, Collective Transport, Mass casualty incidents, Disaster DOI: https://doi.org/10.21203/rs.3.rs-48425/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/14 Abstract Background: During the COVID-19 pandemic, as the number of available Intensive Care beds in France did not meet the needs, it appeared necessary to transfer a large number of patients from the most affected areas to the less ones. Mass transportation resources were deemed necessary. To achieve that goal, the concept of a Collective Advanced Life Support Ambulance (CALSA) was proposed in the form of a long-distance bus re-designed and equipped so as to accommodate up to six intensive care patients and allow Advanced Life Support (ALS) techniques to be performed while en route. Methods: The expected beneƒt of the CALSA, when compared to ALS ambulances accommodating a single patient, was to reduce the resources requirements, in particular by a lower personnel headcount for several patients being transferred to the same destination. A foreseen prospect, comparing to other collective transportation vectors such as airplanes, was the door-to-door capability, minimalizing patients’ handovers for safety concerns and time e∆ciency. -

EMS Spinal Precautions and the Use of the Long Backboard
EMS SPINAL PRECAUTIONS AND THE USE OF THE LONG BACKBOARD – RESOURCE DOCUMENT TO THE POSITION STATEMENT OF THE NATIONAL ASSOCIATION OF EMS PHYSICIANS AND THE AMERICAN COLLEGE OF SURGEONS COMMITTEE ON TRAUMA Chelsea C. White IV, MD, EMT-P, Robert M. Domeier, MD, Michael G. Millin, MD, MPH, and the Standards and Clinical Practice Committee, National Association of EMS Physicians ABSTRACT designed to guide practitioners in understanding of the new position statement. Each item in the position Field spinal immobilization using a backboard and cervical is quoted and followed by a discussion and a review collar has been standard practice for patients with suspected spine injury since the 1960s. The backboard has been a com- of the literature. ponent of field spinal immobilization despite lack of effi- cacy evidence. While the backboard is a useful spinal protec- • “Long backboards are commonly used to attempt tion tool during extrication, use of backboards is not without to provide rigid spinal immobilization among EMS risk, as they have been shown to cause respiratory compro- trauma patients. However, the benefit of long back- mise, pain, and pressure sores. Backboards also alter a pa- boards is largely unproven.” tient’s physical exam, resulting in unnecessary radiographs. Because backboards present known risks, and their value in protecting the spinal cord of an injured patient remains HISTORY OF THE BACKBOARD unsubstantiated, they should only be used judiciously. The following provides a discussion of the elements of the Na- Field spinal immobilization using a cervical collar and tional Association of EMS Physicians (NAEMSP) and Amer- a backboard has been standard practice for patients ican College of Surgeons Committee on Trauma (ACS-COT) with suspected spine injury since the 1960s. -

Protocols, Most Care Is Done by Standing Order Within Your Scope of Practice
ABDOMINAL PAIN 12/03/2013 Follow Assessment, General Procedures Protocol EMR • Assess and support ABCs • Position of comfort • Supine if: • Trauma • Hypotension • Syncope • NPO • Monitor vital signs • Oxygen indicated for: • Unstable vitals • Severity of pain • Suspected GI bleed EMT • 12-lead – See ECG/12 Lead A-EMT • IV – NS with standard tubing • Titrate fluid to patient’s needs – See Shock Protocol EMT-I/ • Cardiac monitoring PARAMEDIC • Pain management – See Acute Pain Management Protocol ACUTE NAUSEA AND VOMITING 12/03/2013 Follow Assessment, General Procedures Protocol Every effort should be made to transport patients that: • Have been vomiting > 6 hours • Show significant signs of dehydration (e.g. tachycardia, hypotension) • Significant abdominal pain • Patients at the extremes of age <5 or >55 • Patients with cardiac history • Patients with a chronic medical condition are especially vulnerable to serious problems associated with prolonged vomiting EMR/EMT • Assess and support ABCs • Position of comfort • Monitor vital signs • Administer oxygen if indicated • Use caution when using a mask EMT • Consider obtaining 12 Lead - See ECG/12 Lead • Check CBG A-EMT • IV – NS with standard tubing • Fluid challenge, titrate fluid to patient’s needs– See Shock Protocol EMT-I • Zofran PARAMEDIC • Inapsine (2nd Line) • Compazine (2nd Line) • Phenergan (2nd Line) ACUTE PAIN MANAGEMENT 02/03/2020 Follow Assessment, General Procedures Protocol Consider administering analgesic medication in the management of any acutely painful condition relating to either trauma or medical causes. The single most reliable indicator of the existence/intensity of acute pain is the patient’s self-report. Most people who suffer pain show it, either by verbal complaint or nonverbal behaviors.