European Paediatric Cardiac Code Short List Crossmapped to STS/EACTS Short List with ICD-9 & ICD-10 Crossmapping
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

446 NQF #0773: Operative Mortality Stratified by the Five STS-EACTS Mortality Categories
Measure #446 (NQF 0733): Operative Mortality Stratified by the Five STS-EACTS Mortality Categories – National Quality Strategy Domain: Patient Safety 2017 OPTIONS FOR INDIVIDUAL MEASURES: REGISTRY ONLY MEASURE TYPE: Outcome DESCRIPTION: Percent of patients undergoing index pediatric and/or congenital heart surgery who die, including both 1) all deaths occurring during the hospitalization in which the procedure was performed, even if after 30 days (including patients transferred to other acute care facilities), and 2) those deaths occurring after discharge from the hospital, but within 30 days of the procedure, stratified by the five STAT Mortality Levels, a multi-institutional validated complexity stratification tool INSTRUCTIONS: This measure is to be reported for all pediatric and/or congenital heart patients each time a surgery is performed during the performance period. This measure is intended to reflect the quality of services provided for patients with congenital heart disease. This measure may be reported by eligible clinicians who perform the quality actions described in the measure based on the services provided and the measure-specific denominator coding. Measure Reporting: The listed denominator criteria is used to identify the intended patient population. The numerator quality-data codes included in this specification are used to submit the quality actions allowed by the measure. All measure-specific coding should be reported on the claim(s) representing the eligible encounter. THERE ARE TWO REPORTING CRITERIA FOR THIS MEASURE: -

Situs Inversus Totalis with Aortopulmonary Shunt: a Case Report in an Ethiopian
Ethiop. J. Health Biomed Sci., 2009. Vol.2, No.1 CASE REPORT SITUS INVERSUS TOTALIS WITH AORTOPULMONARY SHUNT: A CASE REPORT IN AN ETHIOPIAN Ermias Diro1 SUMMARY I report a patient who presented with long standing dyspnea without physical signs of congestive heart failure and finally diag- nosed to have situs inversus totalis with aortopulmonary window. Situs inversus totalis refers to a mirror image reversal of the normal position of the internal organs. The recognition of concomitant congenital anomalies such as in the heart or other or- gans is extremely important as it may disturb surgical procedures for concomitant diseases. This is a very rare condition and a coexisting aortopulmonary window was not described before to the best of my knowledge. their normal positions. Situs inversus with dextrocar- dia is termed situs inversus totalis because the car- INTRODUCTION diac position as well as the atrial chambers and ab- dominal viscera are mirror images of the normal anatomy (3). The purpose of this case report is to describe and discuss a rare situation with an important clinical Typically, patients with situs inversus have a normal significance. life expectancy except in the rare instances of cardiac anomalies, depending on the severity of the defect. Situs describes the position of the cardiac atria and Patients with Kartagners syndrome, a triad of situs viscera. Situs solitus is the normal position, and situs inversus, sinusitis and bronchiectasis, have a normal inversus is the mirror image of situs solitus. Cardiac life expectancy if the bronchiectasis is treated ade- situs is determined by the atrial location. In situs in- quately. -
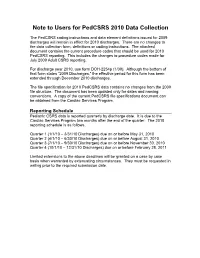
Note to Users for Pedcsrs 2010 Data Collection
Note to Users for PedCSRS 2010 Data Collection The PedCSRS coding instructions and data element definitions issued for 2009 discharges will remain in effect for 2010 discharges. There are no changes to the data collection form, definitions or coding instructions. The attached document contains the current procedure codes that should be used for 2010 PedCSRS reporting. This includes the changes to procedure codes made for July 2009 Adult CSRS reporting. For discharge year 2010, use form DOH-2254p (1/09). Although the bottom of that form states “2009 Discharges,” the effective period for this form has been extended through December 2010 discharges. The file specification for 2010 PedCSRS data contains no changes from the 2009 file structure. The document has been updated only for dates and naming conventions. A copy of the current PedCSRS file specifications document can be obtained from the Cardiac Services Program. Reporting Schedule Pediatric CSRS data is reported quarterly by discharge date. It is due to the Cardiac Services Program two months after the end of the quarter. The 2010 reporting schedule is as follows. Quarter 1 (1/1/10 – 3/31/10 Discharges) due on or before May 31, 2010 Quarter 2 (4/1/10 – 6/30/10 Discharges) due on or before August 31, 2010 Quarter 3 (7/1/10 – 9/30/10 Discharges) due on or before November 30, 2010 Quarter 4 (10/1/10 – 12/31/10 Discharges) due on or before February 28, 2011 Limited extensions to the above deadlines will be granted on a case by case basis when warranted by extenuating circumstances. -

Mustard Procedure Br Heart J: First Published As 10.1136/Hrt.72.1.85 on 1 July 1994
Br Heart J 1994;72:85-88 85 Transcatheter stent implantation for recurrent pulmonary venous pathway obstruction after the Mustard procedure Br Heart J: first published as 10.1136/hrt.72.1.85 on 1 July 1994. Downloaded from Martin C K Hosking, Kenneth A Murdison, Walter J Duncan Abstract pathway obstruction reaching a maximum A 5 year old boy presented with obstruc- flow velocity of 2'0 m/s associated with a tion of the pulmonary venous pathway stenosis measuring 2-3 mm in diameter. four years after the Mustard procedure. Right ventricular dysfunction was a persistent A successful balloon dilatation ofthe pul- echocardiographic finding associated with an monary venous pathway was performed increase in left ventricle dimension in but the benefit was transient. Placement response to the rise of pulmonary arterial of a 10 mm balloon expandable intravas- pressure secondary to the pulmonary venous cular stent across the recurrent stenosis inflow obstruction. A significant systemic to resulted in complete relief ofthe obstruc- pulmonary venous chamber baffle leak mea- tion with prompt resolution ofthe clinical suring 5 mm x 4 mm with right to left shunting signs. The delivery system was modified was seen by Doppler colour flow mapping and to facilitate stent delivery. contributed to central cyanosis. Serial chest x ray films showed persistence of cardiomegaly (Br Heart 1994;72:85-88) with increasing evidence of pulmonary venous congestion. To avoid the risks of surgical repair in a Paediatric experience with transcatheter patient with impaired -

Mustard Operation
Mustard Operation William G. Williams The natural history of infants with complete transposi- desaturation. Mustard reasoned that both vena cavae tion (TGA) is rapid deterioration and death within the could be deliberately diverted to the left atrium while first few months of life. The few babies who do survive allowing the pulmonary return to enter the right atrium, beyond the first year of life usually have an associated thereby correcting the circulation in patients with TGA. ventricular septal defect (VSD) and subsequently dete- The Mustard baffle operation was a simple, reproduc- riorate with progressive pulmonary vascular disease. ible, and elegant technique of transposing venous re- Intervention to improve the outlook for newborns turn. It was easier to learn than the Senning operation, with TGA began with surgical resection of the atrial and became the standard repair in most of the world. septum.' The enlarged atrial defect improves mixing of the pulmonary and systemic circulations, thereby in- creasing the systemic oxygen saturation. Balloon atrial Indications for the Mustard Operation in 1998 septostomy, as described by Rashkind and Miller in The atrial repair of TGA has been almost entirely 1966,2 replaced surgical septectomy. The balloon cath- replaced by the arterial switch operation. However, eter technique continues to provide effective emergency there are three situations were the Mustard operation palliation for the newborn with TGA. may be indicated: In the early 1950s, a number of surgeons, including 1. For infants with isolated TGA who first present M~stard,~attempted arterial repair of TGA in infants, after the neonatal period, the Mustard operation is an all without success until Jatene's report in 1978.4 In alternative to the two-stage arterial switch operation, 1954, Albert5 proposed a surgical technique to trans- ie, a preliminary pulmonary artery banding to prepare pose the venous inflow within the atria to correct TGA. -

Relation of Biventricular Function Quantified by Stress
Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, Tim S. Hornung, Darrel P. Francis, Christine O’Sullivan, Alison Duncan, Michael Gatzoulis and Michael Henein Circulation 2004;110;1380-1386; originally published online Aug 23, 2004; DOI: 10.1161/01.CIR.0000141370.18560.D1 Circulation is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX 72514 Copyright © 2005 American Heart Association. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/cgi/content/full/110/11/1380 Subscriptions: Information about subscribing to Circulation is online at http://circ.ahajournals.org/subsriptions/ Permissions: Permissions & Rights Desk, Lippincott Williams & Wilkins, 351 West Camden Street, Baltimore, MD 21202-2436. Phone 410-5280-4050. Fax: 410-528-8550. Email: [email protected] Reprints: Information about reprints can be found online at http://www.lww.com/static/html/reprints.html Downloaded from circ.ahajournals.org at NHLI - Royal Brompton on January 29, 2006 Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, MD, PhD; Tim S. Hornung, MD; Darrel P. Francis, MRCP; Christine O’Sullivan, BSc; Alison Duncan, MRCP; Michael Gatzoulis, MD, PhD; Michael Henein, MD, PhD Background—Mustard repair for transposition of the great arteries (TGA) is frequently associated with impaired systemic (right) ventricular function and sometimes exercise intolerance. -

Abernathys Surgical Secrets 6Th Edition
1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103–2899 ABERNATHY’S SURGICAL SECRETS, SIXTH EDITION ISBN: 978-0-323-05711-0 Copyright Q 2009, 2005, 2003, 2000, 1996, 1991, 1986 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Permissions may be sought directly from Elsevier’s Rights Department: phone: (þ1) 215 239 3804 (US) or (þ44) 1865 843830 (UK); fax: (þ44) 1865 853333; e-mail: [email protected]. You may also complete your request on-line via the Elsevier website at http://www.elsevier.com/permissions. NOTICE Knowledge and best practice in this field are constantly changing. As new research and experience broaden our knowledge, changes in practice, treatment and drug therapy may become necessary or appropriate. Readers are advised to check the most current information provided (i) on procedures featured or (ii) by the manufacturer of each product to be administered, to verify the recommended dose or formula, the method and duration of administration, and contraindications. It is the responsibility of the practitioner, relying on their own experience and knowledge of the patient, to make diagnoses, to determine dosages and the best treatment for each individual patient, and to take all appropriate safety precautions. To the fullest extent of the law, neither the Publisher nor the Editor assumes any liability for any injury and/or damage to persons or property arising out of or related to any use of the material contained in this book. -

Imperforate Anus Associated with Anomalous Pulmonary Venous Return in Scimitar Syndrome
Aklilu et al. BMC Pediatrics (2019) 19:296 https://doi.org/10.1186/s12887-019-1643-z CASEREPORT Open Access Imperforate anus associated with anomalous pulmonary venous return in scimitar syndrome. Case report from a tertiary hospital in Ethiopia Tamirat Moges Aklilu1* , Messele Chanie Adhana2 and Azmeraw Gissila Aboye3 Abstract Background: Scimitar syndrome is a rare form of partial anomalous pulmonary venous drainage associated with pulmonary hypertension and congestive heart failure that may lead to death in the newborn infant. Although it is described with anomalies of the lung, heart and their vascular structure, extremely rare association with imperforate anus had been reported. The third case of Scimitar syndrome and imperforate anus will be reported in this case report. Case presentation: A 3 days old male neonate with imperforate anus presented with abdominal distention. Loop colostomy was done to relieve abdominal distension. The chest x-ray revealed a curved shadow on the right mid lung zone extending to the diaphragm abutting and indenting the inferior vena cava (scimitar sign). Abdominal ultrasound, transthoracic echocardiography and computerized tomographic angiography confirmed the presence of Scimitar vein and associated dextro-position of the heart, hypoplastic right lung, hypoplastic right pulmonary artery, secundum atrial septal defect with bidirectional shunt, patent ductus arteriosus, pulmonary hypertension, left superior vena cava, and systemic collateral arteries feeding the lower lobe of the right lung. The rare association of scimitar syndrome with imperforate anus is discussed. Conclusion: Scimitar syndrome associated with imperforate anus with and without VACTERL association has been reported previously only in four cases. The knowledge of association between imperforate anus and Scimitar syndrome helps for early detection and management of cases. -

All Forms Combined
Not Started Institutional Practice Details Print this Form Date of Completion DD/MM/YYYY 1. Indicate the day, month, and year the form is being completed. Previous year’s hospital case Less than or equal to 100 per year 2. volume of congenital cardiac 101-250 per year surgeries 251-500 per year Indicate the case volume of Tier 1 AND Tier 2 surgeries for the previous Greater than 500 per year calendar year. (This is the total number of surgeries, not the number of patients.) Active congenital heart surgeons active congenital heart 3. Indicate the number of active congenital heart surgeons currently surgeons practicing at your hospital. How is a congenital heart 3a surgeon certified in your country? Cardioplegia Type Buckberg 4. Check all cardioplegia types that your hospital uses. If there are Custodiol/Bretschneider (HTK) multiple cardioplegia types that your hospital uses that are not Del Nido options in the list provided, enter all of them in the "other, specify" box Microplegia with Adenocaine seperating them by commas (,). 0 option(s) selected Microplegia with Potassium Plegisol/St. Thomas Roe's Solution University of Wisconsin Other, specify Geographic Region Served Local: one city or metro area 5. Regional: geographically larger than a metro area National: one country International: multiple countries Estimated Population Served Less than 10 million 6. Based on answer to the previous question. 10-30 million 31-50 million Greater than 51 million Unknown Total number of institutions Missing Reason: 7. providing pediatric cardiac Clear Unknown services in the region. Based on answer to question 5. Specify the total number including your institution. -

Echocardiographic Assessment of TGA After Atrial Switch Repair
Echocardiographic assessment of TGA after Atrial switch repair Session 6. Transposition of the great arteries Multimodality Imaging in ACHD and PH Annemien van den Bosch Erasmus MC, Thoraxcenter, Rotterdam, The Netherlands Transposition of the Great Arteries . Mustard and Senning operations establish appropriate connection - between systemic venous pathways and subpulmonic ventricle - between pulmonary venous pathway and the systemic ventricle . At the expense of a morphological RV support systemic circulation Atrial switch operation Mustard Procedure: Uses baffles made from Dacron, GoreTex or pericardial tissue to redirect flow Hans Hamer© Atrial switch operation Senning Procedure: Uses tissue from the right atrium and the atrial septum to redirect flow. Diagrams from Popelova et al Post-operative Sequelae Baffle problems . Baffle obstruction - SVC baffle obstruction more common following Mustard operation 5-10% superior, 1% inferior - PV baffle obstruction is more common following Senning operation . Baffle leaks - Small leaks are common and not haemodynamically 25% important, except in the case of cryptogenic stroke - Large leaks are rarer but important due to associated volume overload 1-2 re-op% Post-operative Sequelae . Systemic RV - Hypertrophy - Dilatation (lack of reference values for systemic RV) - Systolic function invariably deteriorates over time . Tricuspid regurgitation - TR is predominantly due to annular dilatation and is likely functional rather than due to primary organic abnormality. In rare cases, structural tricuspid -

Klinička Slika Kasne Novorođenačke Sepse – I Dalje Ozbiljan Diferencijalnodijagnostički Problem
Liječ Vjesn 2019;141:150–161 https://doi.org/10.26800/LV-141-5-6-21 Pregled | Review Klinička slika kasne novorođenačke sepse – i dalje ozbiljan diferencijalnodijagnostički problem Clinical manifestation of late neonatal sepsis – continuous differential diagnostic dilemma Matej Katavić1, Andrea Dasović Buljević2 1 Klinika za pedijatriju, KBC Sestre milosrdnice 2 Zavod za neonatologiju i neonatalno intenzivno liječenje, Klinika za pedijatriju, Medicinski fakultet Sveučilišta u Zagrebu, KBC Zagreb Deskriptori SAŽETAK. Novorođenačka sepsa kao klinički sindrom jedan je od najčešćih dijagnostičko-terapijskih izazova u NOVOROĐENAČKA SEPSA – dijagnoza, etiologija, novorođenačkoj dobi s relativno visokom stopom smrtnosti. Prema dobi manifestacije, dijeli se na ranu i kasnu liječenje; SEPTIČKI ŠOK – dijagnoza, liječenje; sepsu, ovisno o izvorima i mišljenjima raznih stručnjaka. Može se očitovati poremećajem svih organskih sustava i DIFERENCIJALNA DIJAGNOZA; brojnim kasnim komplikacijama te znatnim morbiditetom i mortalitetom. Razdoblje od drugog tjedna života NOVOROĐENAČKE BOLESTI – dijagnoza, liječenje primarni je interes ovog rada jer je u tom periodu (dotad prividno zdrava) novorođenčad otpuštena kući iz rodi- lišta, adaptirana na svakodnevne zahtjeve ekstrauterinog života, s mogućnošću razvoja niza neinfektivnih stanja i bolesti koji klinički izgledaju kao septičko stanje. Široka diferencijalna dijagnoza takvog stanja može biti ozbiljan problem koji nalaže hitnu reakciju, pravilno i pravodobno liječenje te, naposljetku, zbrinjavanje u adekvatnoj -

Cardiovascular Magnetic Resonance (CMR) Page 1 of 11
Cardiovascular Magnetic Resonance (CMR) Page 1 of 11 No review or update is scheduled on this Medical Policy as it is unlikely that further published literature would change the policy position. If there are questions about coverage of this service, please contact Blue Cross and Blue Shield of Kansas customer service, your professional or institutional relations representative, or submit a predetermination request. Medical Policy An independent licensee of the Blue Cross Blue Shield Association Title: Cardiovascular Magnetic Resonance (CMR) Professional Institutional Original Effective Date: August 4, 2005 Original Effective Date: July 1, 2006 Revision Date(s): February 27, 2006, Revision Date(s): May 2, 2007; May 2, 2007; November 1, 2007; November 1, 2007; January 1, 2010; January 1, 2010; February 15, 2013; February 15, 2013; December 11, 2013; December 11, 2013; April 15, 2014; April 15, 2014; July 15, 2014; June 10, 2015; July 15, 2014; June 10, 2015; June 8, 2016; June 8, 2016; October 1, 2016; October 1, 2016; May 10, 2017; May 10, 2017; April 25, 2018; April 25, 2018; October 1, 2018 October 1, 2018 Current Effective Date: July 15, 2014 Current Effective Date: July 15, 2014 Archived Date: July 3, 2019 Archived Date: July 3, 2019 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS.