TOPICC Public Use Dataset Annotated Ecrf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Program PDF Saturday, March 28, 2020 Updated: 02-14-20
Program PDF Saturday, March 28, 2020 Updated: 02-14-20 Special ‐ Events and Meetings Congenital Heart Disease ‐ Scientific Session #5002 Session #602 Fellowship Administrators in Cardiovascular Education and ACHD Cases That Stumped Me Training Meeting, Day 2 Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. Saturday, March 28, 2020, 7:30 a.m. ‐ 5:30 p.m. Room S105b Marriott Marquis Chicago, Great Lakes Ballroom A CME Hours: 1.5 / CNE Hours: CME Hours: / CNE Hours: Co‐Chair: C. Huie Lin 7:30 a.m. Co‐Chair: Karen K. Stout Fellowship Administrators in Cardiovascular Education and Training Meeting, Day 2 8:00 a.m. LTGA, Severe AV Valve Regurgitation, Moderately Reduced EF, And Atrial Acute and Stable Ischemic Heart Disease ‐ Scientific Arrhythmia Session #601 Elizabeth Grier Treating Patients With STEMI: What They Didn't Teach You in Dallas, TX Fellowship! Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. 8:05 a.m. Room S505a ARS Questions (Pre‐Panel Discussion) CME Hours: 1.5 / CNE Hours: Elizabeth Grier Dallas, TX Co‐Chair: Frederick G. Kushner Co‐Chair: Alexandra J. Lansky 8:07 a.m. Panelist: Alvaro Avezum Panel Discussion: LTGA With AVVR And Reduced EF Panelist: William W. O'Neill Panelist: Jennifer Tremmel Panelist: Jonathan Nathan Menachem Panelist: Joseph A. Dearani 8:00 a.m. Panelist: Michelle Gurvitz Case of a Young Women With STEMI Panelist: David Bradley Jasjit Bhinder Valhalla, NY 8:27 a.m. ARS Questions (Post‐Panel Discussion) 8:05 a.m. Elizabeth Grier Young Women With STEMI: Something Doesn't Make Sense... -

The Increase of the Pulmonary Blood Flow Inhigh-Risk Hypoxic Patients with a Bidirectional Glenn Anastomosis
ORIGINAL ARTICLE The increase of the pulmonary blood flow inhigh-risk hypoxic patients with a bidirectional Glenn anastomosis Jacek Kołcz1, Mirosława Dudyńska2, Aleksandra Morka3, Sebastian Góreczny4, Janusz Skalski1 1Department of Pediatric Cardiac Surgery, Jagiellonian University Medical College, Kraków, Poland 2Department of Pediatric Cardiac Surgery, University Children’s Hospital in Krakow, Kraków, Poland 3Faculty of Health Sciences, Jagiellonian University Medical College, Kraków, Poland 4Department of Pediatric Cardiology, Jagiellonian University Medical College, Kraków, Poland Correspondence to: Jacek Kołcz, MD, PhD, ABSTRACT FECTS, Department of Pediatric Background: An additional shunt in single ventricle patients with Glenn anastomosis may increase Cardiac Surgery, pulmonary flow at the expense of ventricle volume overloading. The performance of the modification Jagiellonian University depends on pulmonary resistance, indicating better results in favorable hemodynamic conditions. Medical College, Wielicka 265, Aims: The study aims at analyzing the influence of precisely adjusted pulsatile shunt in borderline 30–663 Kraków, Poland, phone: +40 12 658 20 11, high-risk Glenn patients on early and late results. e-mail: Methods: The study involved 99 patients (including 21 children) with the bidirectional Glenn and ac- [email protected] cessory pulsatile shunt (BDGS group), and 78 patients with the classic bidirectional Glenn anastomosis Copyright by the Author(s), 2021 (BDG group). Kardiol Pol. 2021; Results: There was 1 death in the BDGS group and 4 deaths in the BDG group. No difference in mortality 79 (6): 638–644; DOI: 10.33963/KP.15939 (P = 0.71) was found. The Fontan completion was achieved in 69 (88.5%) children in the BDG group and Received: 18 (85.7%) patients in the BDGS group, without fatalities. -

The Physiology of the Fontan Circulation ⁎ Andrew Redington
Progress in Pediatric Cardiology 22 (2006) 179–186 www.elsevier.com/locate/ppedcard The physiology of the Fontan circulation ⁎ Andrew Redington Division of Cardiology, The Department of Pediatrics, The Hospital for Sick Children, University of Toronto School of Medicine, Toronto, Ontario, Canada Available online 8 September 2006 Abstract The Fontan circulation, no matter which of its various iterations, is abnormal in virtually every aspect of its performance. Some of these abnormalities are primarily the result of the procedure itself, and others are secondary to the fundamental disturbances of circulatory performance imposed by the ‘single’ ventricle circulation. The physiology of ventricular, systemic arterial and venopulmonary function will be described in this review. © 2006 Elsevier Ireland Ltd. All rights reserved. Keywords: palliation; Fontan circulation; Cavopulmonary anastomosis; Antriopulmonary anastomosis 1. Introduction has the profound consequences for the systemic ventricle that will discussed below. At the same time as the bidirectional In this personal overview, I will discuss the physiology of the cavopulmonary anastomosis was becoming almost uniformly Fontan circulation. Bob Freedom's contribution to our under- adopted, there was abandonment of the ‘classical’ atriopulmon- standing of complex congenital heart disease has meant that ary anastomosis, in favour of the total cavopulmonary con- many more of these patients are surviving with this physiology nection (TCPC). The ‘lateral wall’ TCPC, popularised by Marc than could have been contemplated 30 years ago. Nonetheless, deLeval [1], was shown experimentally and clinically to be they represent a very difficult group of patients and we continue haemodynamically more efficient [1,2] and set the scene for the to learn more about this unique circulation. -

A Better Approach for Left Ventricular Training In
Received: 28 September 2018 | Revised: 7 November 2018 | Accepted: 29 December 2018 DOI: 10.1111/chd.12749 ORIGINAL ARTICLE A better approach for left ventricular training in transposition of the great arteries and intact interventricular septum: Bidirectional cavopulmonary anastomosis and pulmonary artery banding Mehmet Salih Bilal MD1 | Arda Özyüksel MD1,2 | Mustafa Kemal Avşar MD1 | Şener Demiroluk MD3 | Osman Küçükosmanoğlu MD4 | Yalım Yalçın MD5 1Department of Cardiovascular Surgery, Medicana International Hospital, Abstract Istanbul, Turkey Objective: Management of the patients with transposition of the great arteries and 2 Department of Cardiovascular intact ventricular septum may be challenging beyond the newborn period. Herein, we Surgery, Biruni University, Istanbul, Turkey would like to present our alternative strategy for training the left ventricle in these 3Department of Anesthesiology, Medicana International Hospital, Istanbul, Turkey patients. 4Department of Pediatric Methods: Six patients with transposition of the great arteries and intact ventricular Cardiology, Medicana International Hospital, Istanbul, Turkey septum were evaluated in our clinic. Two of them were palliated with Glenn proce- 5Department of Pediatric dure and pulmonary banding as a definitive treatment strategy at other centers. Four Cardiology, Florence Nightingale Hospital, patients were operated on and a bidirectional cavopulmonary anastomosis in combi- Istanbul, Turkey nation with pulmonary artery banding was performed (stage‐1: palliation and ven- Correspondence tricular training) in our center. In four out of these six patients, arterial switch Arda Özyüksel, Department of Cardiovascular Surgery, Medicana operation was performed with takedown and direct re‐anastomosis of the superior International Hospital, Beylikdüzü Caddesi, vena cava to right atrium after an interstage period of 21‐30 months (stage‐2: ana- No:3, Beylikdüzü, Istanbul, Turkey. -

Overview of Partial Left Ventriculectomy
Prepared by ASERNIP-S NATIONAL INSTITUTE FOR CLINICAL EXCELLENCE INTERVENTIONAL PROCEDURES PROGRAMME Interventional procedure overview of Partial Left Ventriculectomy Introduction This overview has been prepared to assist members of IPAC advise on the safety and efficacy of an interventional procedure previously reviewed by SERNIP. It is based on a rapid survey of published literature, review of the procedure by specialist advisors and review of the content of the SERNIP file. It should not be regarded as a definitive assessment of the procedure. Procedure name Partial Left Ventriculectomy The Batista Procedure Specialty society Society of Cardiothoracic Surgeons of Great Britain and Ireland Executive Summary Left partial ventriculectomy (PLV) seeks to treat dilated cardiomyopathy by reducing cardiac volume and hence heart wall pressure through the resection of a portion of the left ventricle. Patients receiving it are generally suitable for cardiac transplant but unable to receive it, often for social or economic reasons. PLV is an emerging procedure and the vast majority of evidence is case series, although there has been one retrospective comparative study of PLV and transplantation. Hospital mortality was reported for up to 30% of patients and overall mortality was around 40% of patients. Thirty day survival ranged from 50% to 99%, and no significant difference was found between PLV and transplant. One-year survival ranged from 46% to 80% and three- year survival was reported in one study as 60%. Event-free survival was reported as 80% at 30 days, 49% at 1 year and 26% at three years. Use of a left ventricular assist device or relisting for cardiac surgery was reported in one study at between 5% and 15% of patients at 30 days and in 43% at 1 year and 58% at 3 years. -
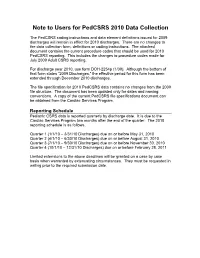
Note to Users for Pedcsrs 2010 Data Collection
Note to Users for PedCSRS 2010 Data Collection The PedCSRS coding instructions and data element definitions issued for 2009 discharges will remain in effect for 2010 discharges. There are no changes to the data collection form, definitions or coding instructions. The attached document contains the current procedure codes that should be used for 2010 PedCSRS reporting. This includes the changes to procedure codes made for July 2009 Adult CSRS reporting. For discharge year 2010, use form DOH-2254p (1/09). Although the bottom of that form states “2009 Discharges,” the effective period for this form has been extended through December 2010 discharges. The file specification for 2010 PedCSRS data contains no changes from the 2009 file structure. The document has been updated only for dates and naming conventions. A copy of the current PedCSRS file specifications document can be obtained from the Cardiac Services Program. Reporting Schedule Pediatric CSRS data is reported quarterly by discharge date. It is due to the Cardiac Services Program two months after the end of the quarter. The 2010 reporting schedule is as follows. Quarter 1 (1/1/10 – 3/31/10 Discharges) due on or before May 31, 2010 Quarter 2 (4/1/10 – 6/30/10 Discharges) due on or before August 31, 2010 Quarter 3 (7/1/10 – 9/30/10 Discharges) due on or before November 30, 2010 Quarter 4 (10/1/10 – 12/31/10 Discharges) due on or before February 28, 2011 Limited extensions to the above deadlines will be granted on a case by case basis when warranted by extenuating circumstances. -

Mustard Procedure Br Heart J: First Published As 10.1136/Hrt.72.1.85 on 1 July 1994
Br Heart J 1994;72:85-88 85 Transcatheter stent implantation for recurrent pulmonary venous pathway obstruction after the Mustard procedure Br Heart J: first published as 10.1136/hrt.72.1.85 on 1 July 1994. Downloaded from Martin C K Hosking, Kenneth A Murdison, Walter J Duncan Abstract pathway obstruction reaching a maximum A 5 year old boy presented with obstruc- flow velocity of 2'0 m/s associated with a tion of the pulmonary venous pathway stenosis measuring 2-3 mm in diameter. four years after the Mustard procedure. Right ventricular dysfunction was a persistent A successful balloon dilatation ofthe pul- echocardiographic finding associated with an monary venous pathway was performed increase in left ventricle dimension in but the benefit was transient. Placement response to the rise of pulmonary arterial of a 10 mm balloon expandable intravas- pressure secondary to the pulmonary venous cular stent across the recurrent stenosis inflow obstruction. A significant systemic to resulted in complete relief ofthe obstruc- pulmonary venous chamber baffle leak mea- tion with prompt resolution ofthe clinical suring 5 mm x 4 mm with right to left shunting signs. The delivery system was modified was seen by Doppler colour flow mapping and to facilitate stent delivery. contributed to central cyanosis. Serial chest x ray films showed persistence of cardiomegaly (Br Heart 1994;72:85-88) with increasing evidence of pulmonary venous congestion. To avoid the risks of surgical repair in a Paediatric experience with transcatheter patient with impaired -

Mustard Operation
Mustard Operation William G. Williams The natural history of infants with complete transposi- desaturation. Mustard reasoned that both vena cavae tion (TGA) is rapid deterioration and death within the could be deliberately diverted to the left atrium while first few months of life. The few babies who do survive allowing the pulmonary return to enter the right atrium, beyond the first year of life usually have an associated thereby correcting the circulation in patients with TGA. ventricular septal defect (VSD) and subsequently dete- The Mustard baffle operation was a simple, reproduc- riorate with progressive pulmonary vascular disease. ible, and elegant technique of transposing venous re- Intervention to improve the outlook for newborns turn. It was easier to learn than the Senning operation, with TGA began with surgical resection of the atrial and became the standard repair in most of the world. septum.' The enlarged atrial defect improves mixing of the pulmonary and systemic circulations, thereby in- creasing the systemic oxygen saturation. Balloon atrial Indications for the Mustard Operation in 1998 septostomy, as described by Rashkind and Miller in The atrial repair of TGA has been almost entirely 1966,2 replaced surgical septectomy. The balloon cath- replaced by the arterial switch operation. However, eter technique continues to provide effective emergency there are three situations were the Mustard operation palliation for the newborn with TGA. may be indicated: In the early 1950s, a number of surgeons, including 1. For infants with isolated TGA who first present M~stard,~attempted arterial repair of TGA in infants, after the neonatal period, the Mustard operation is an all without success until Jatene's report in 1978.4 In alternative to the two-stage arterial switch operation, 1954, Albert5 proposed a surgical technique to trans- ie, a preliminary pulmonary artery banding to prepare pose the venous inflow within the atria to correct TGA. -

Real-Time 3-Dimensional Echocardiography of the Heart 13 Years After Partial Left Ventriculectomy
IMAGES IN CARDIOVASCULAR MEDICINE Print ISSN 1738-5520 / On-line ISSN 1738-5555 DOI 10.4070 / kcj.2010.40.6.295 Copyright ⓒ 2010 The Korean Society of Cardiology Open Access Real-Time 3-Dimensional Echocardiography of the Heart 13 Years After Partial Left Ventriculectomy Mi-Seung Shin, MD1, Tae Hoon Ahn, MD1, Ok Ryun Kim, RDCS1, Wook-Jin Chung, MD1, Woong Chol Kang, MD1, Kyoung Hoon Lee, MD1, Chan Il Moon, MD1, In Suck Choi, MD1, Eak Kyun Shin, MD1 and Chang Young Lim, MD2 1Division of Cardiology, Department of Internal Medicine, Gachon University, Gil Hospital, Incheon, 2Department of Thoracic and Cardiovascular Surgery, CHA University, Bundang CHA Hospital, Seongnam, Korea A 69-year-old woman diagnosed as having end-stage ure.2) Resection of the myocardium not only decreases dilated cardiomyopathy had undergone partial left ven- wall stress according to Laplace’s law, but may improve triculectomy (PLV) in 1996. This is the first reported stroke volume for sufficiently dilated and depressed ven- case of PLV (Batista procedure) in Korea.1) She was do- tricles. Using these operative techniques to alter the ing well under the New York Heart Association class II shape of the LV, in combination with optimal medical diagnosis in November 2009 and had received 3-dimen- management for heart failure, improves survival.3) Al- sional (3D) echocardiography for the evaluation of car- though a favorable outcome has been reported in se- diac function. lected patients, this method is currently not recommend- Full volume 3D echocardiography (Philips Medical, ed for treatment of heart failure because of high surgical IE33, Bothell, WA, USA) of the heart showed a dilated failure rates.4)5) Here, we report 3D echocardiographic left ventricle (LV) and gave a more accurate LV ejection findings of long-term survival of a patient who had un- fraction and time-volume curve during one cardiac cycle dergone a Batista procedure 13 years ago. -

Relation of Biventricular Function Quantified by Stress
Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, Tim S. Hornung, Darrel P. Francis, Christine O’Sullivan, Alison Duncan, Michael Gatzoulis and Michael Henein Circulation 2004;110;1380-1386; originally published online Aug 23, 2004; DOI: 10.1161/01.CIR.0000141370.18560.D1 Circulation is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX 72514 Copyright © 2005 American Heart Association. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/cgi/content/full/110/11/1380 Subscriptions: Information about subscribing to Circulation is online at http://circ.ahajournals.org/subsriptions/ Permissions: Permissions & Rights Desk, Lippincott Williams & Wilkins, 351 West Camden Street, Baltimore, MD 21202-2436. Phone 410-5280-4050. Fax: 410-528-8550. Email: [email protected] Reprints: Information about reprints can be found online at http://www.lww.com/static/html/reprints.html Downloaded from circ.ahajournals.org at NHLI - Royal Brompton on January 29, 2006 Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, MD, PhD; Tim S. Hornung, MD; Darrel P. Francis, MRCP; Christine O’Sullivan, BSc; Alison Duncan, MRCP; Michael Gatzoulis, MD, PhD; Michael Henein, MD, PhD Background—Mustard repair for transposition of the great arteries (TGA) is frequently associated with impaired systemic (right) ventricular function and sometimes exercise intolerance. -

Medicare National Coverage Determinations Manual, Part 1
Medicare National Coverage Determinations Manual Chapter 1, Part 1 (Sections 10 – 80.12) Coverage Determinations Table of Contents (Rev. 10838, 06-08-21) Transmittals for Chapter 1, Part 1 Foreword - Purpose for National Coverage Determinations (NCD) Manual 10 - Anesthesia and Pain Management 10.1 - Use of Visual Tests Prior to and General Anesthesia During Cataract Surgery 10.2 - Transcutaneous Electrical Nerve Stimulation (TENS) for Acute Post- Operative Pain 10.3 - Inpatient Hospital Pain Rehabilitation Programs 10.4 - Outpatient Hospital Pain Rehabilitation Programs 10.5 - Autogenous Epidural Blood Graft 10.6 - Anesthesia in Cardiac Pacemaker Surgery 20 - Cardiovascular System 20.1 - Vertebral Artery Surgery 20.2 - Extracranial - Intracranial (EC-IC) Arterial Bypass Surgery 20.3 - Thoracic Duct Drainage (TDD) in Renal Transplants 20.4 – Implantable Cardioverter Defibrillators (ICDs) 20.5 - Extracorporeal Immunoadsorption (ECI) Using Protein A Columns 20.6 - Transmyocardial Revascularization (TMR) 20.7 - Percutaneous Transluminal Angioplasty (PTA) (Various Effective Dates Below) 20.8 - Cardiac Pacemakers (Various Effective Dates Below) 20.8.1 - Cardiac Pacemaker Evaluation Services 20.8.1.1 - Transtelephonic Monitoring of Cardiac Pacemakers 20.8.2 - Self-Contained Pacemaker Monitors 20.8.3 – Single Chamber and Dual Chamber Permanent Cardiac Pacemakers 20.8.4 Leadless Pacemakers 20.9 - Artificial Hearts And Related Devices – (Various Effective Dates Below) 20.9.1 - Ventricular Assist Devices (Various Effective Dates Below) 20.10 - Cardiac -

Glenn Surgery: a Safe Procedure in the Path of Univentricular Correction
Boletín Médico del Hospital Infantil de México RESEARCH ARTICLE Glenn surgery: a safe procedure in the path of univentricular correction Guadalupe Hernández-Morales1*, Alejandro Bolio-Cerdán2, Sergio Ruiz-González2, Patricia Romero-Cárdenas2, and Miguel A. Villasís-Keever3 1Departamento de Cirugía Cardiaca en Pediatría, Hospital Militar de Especialidades de la Mujer y Neonatología; 2Departamento de Cirugía Cardiovascular, Hospital Infantil de México Federico Gómez; 3Unidad de Investigación en Epidemiología Clínica, Unidad Médica de Alta Especialidad, Hospital de Pediatría, Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social. Mexico City, Mexico Abstract Background: This study describes 35 years of experience in a tertiary care level hospital that treats cardiac patients with univentricular heart physiology who underwent Glenn surgery. Methods: The study consisted of a retrospective analysis of patients who underwent Glenn surgery, including variables related to pre-operative, intra-operative, and post-operative mor- bidity and mortality. Results: From 1980 to 2015, 204 Glenn surgeries were performed. The most common heart disease was tricuspid atresia IB (19.2%). In 48.1% of the cases, the procedure was performed with antegrade flow. A bilateral Glenn procedure was performed in 12.5% of the cases and 10.3% were carried out without using a cardiopulmonary bypass pump. Reported complications included infections, bleeding, arrhythmias, chylothorax, neurological alterations, and pleural effusion. The mortality rate was 2.9%. Conclusions: Glenn surgery is a palliative surgery with good results. It significantly improves patient quality of life over a long period until a total cavopulmonary shunt is performed. The complications observed are few, and the mortality rate is low.