The Physiology of the Fontan Circulation ⁎ Andrew Redington
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Program PDF Saturday, March 28, 2020 Updated: 02-14-20
Program PDF Saturday, March 28, 2020 Updated: 02-14-20 Special ‐ Events and Meetings Congenital Heart Disease ‐ Scientific Session #5002 Session #602 Fellowship Administrators in Cardiovascular Education and ACHD Cases That Stumped Me Training Meeting, Day 2 Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. Saturday, March 28, 2020, 7:30 a.m. ‐ 5:30 p.m. Room S105b Marriott Marquis Chicago, Great Lakes Ballroom A CME Hours: 1.5 / CNE Hours: CME Hours: / CNE Hours: Co‐Chair: C. Huie Lin 7:30 a.m. Co‐Chair: Karen K. Stout Fellowship Administrators in Cardiovascular Education and Training Meeting, Day 2 8:00 a.m. LTGA, Severe AV Valve Regurgitation, Moderately Reduced EF, And Atrial Acute and Stable Ischemic Heart Disease ‐ Scientific Arrhythmia Session #601 Elizabeth Grier Treating Patients With STEMI: What They Didn't Teach You in Dallas, TX Fellowship! Saturday, March 28, 2020, 8:00 a.m. ‐ 9:30 a.m. 8:05 a.m. Room S505a ARS Questions (Pre‐Panel Discussion) CME Hours: 1.5 / CNE Hours: Elizabeth Grier Dallas, TX Co‐Chair: Frederick G. Kushner Co‐Chair: Alexandra J. Lansky 8:07 a.m. Panelist: Alvaro Avezum Panel Discussion: LTGA With AVVR And Reduced EF Panelist: William W. O'Neill Panelist: Jennifer Tremmel Panelist: Jonathan Nathan Menachem Panelist: Joseph A. Dearani 8:00 a.m. Panelist: Michelle Gurvitz Case of a Young Women With STEMI Panelist: David Bradley Jasjit Bhinder Valhalla, NY 8:27 a.m. ARS Questions (Post‐Panel Discussion) 8:05 a.m. Elizabeth Grier Young Women With STEMI: Something Doesn't Make Sense... -

Early Diastolic Clicks After the Fontan Procedure for Double
304 Br Heart J 1990;63:304-7 Early diastolic clicks after the Fontan procedure for double inlet left ventricle: anatomical and physiological correlates Br Heart J: first published as 10.1136/hrt.63.5.304 on 1 May 1990. Downloaded from Andrew N Redlngton, Kit-Yee Chan, Julene S Carvalho, Elliot A Shinebourne Abstract inlet ventricle with two atrioventricular M mode echocardiograms and simultan- valves. All had previously undergone a Fontan eous phonocardiograms were recorded type procedure with direct atriopulmonary in four patients with early diastolic anastomosis. In two patients a valved clicks on auscultation. All had double homograft was interposed between the right inlet left ventricle and had undergone atrium and pulmonary artery. Each patient the Fontan procedure with closure of the had the right atrioventricular valve closed by right atrioventricular valve orifice by an either a single or double layer of Dacron cloth artifical patch. The phonocardiogram sewn into the floor of the right atrium. The confirmed a high frequency sound main pulmonary artery was tied off in all. occurring 60-90 ms after aortic valve Cross sectional, M mode, and pulsed wave closure and coinciding with the time of Doppler echocardiograms with simultaneous maximal excursion of the atrioven- electrocardiogram and phonocardiogram were tricular valve patch towards the ven- recorded on a Hewlett-Packard 77020A tricular mass. One patient had coexist- ultrasound system. The phonocardiogram was ing congenital complete heart block. recorded over the point on the chest where the The M mode echocardiogram showed diastolic click was best heart on auscultation, i'reversed") motion of the patch towards usually in the fourth left intercostal space the right atrium during atrial contrac- close to the sternum. -
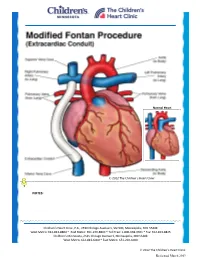
Modified Fontan Procedure: Extracardiac Conduit
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Modified Fontan Procedure: Extracardiac Conduit The Fontan procedure is usually the third procedure done in a series of surgeries to complete palliation of single ventricle patients. This procedure separates the “blue,” deoxygenated blood from the “red,” oxygenated blood circuit. Once the Fontan is done, deoxygenated blood drains passively to the pulmonary arteries, then to the lungs. Blood receives oxygen from the lungs and returns to the heart, where it is actively pumped out to the body. This procedure is usually done between 2-4 years of age. During surgery, the chest is opened through the previous incision, using a median sternotomy. The operation may or may not involve the use of cardiopulmonary bypass (heart-lung machine), depending on the surgical plan. A Gore-tex® tube graft (Gore) is cut to the appropriate length. An incision is made on the pulmonary artery near the area of the existing bidirectional Glenn shunt (cavopulmonary anastomosis) and the tube graft is sutured to the artery. Once that is complete, the inferior vena cava is divided from the atrium. The lower end of the Gore-tex® tube graft (Gore) is then sutured to the inferior vena cava. -

The Increase of the Pulmonary Blood Flow Inhigh-Risk Hypoxic Patients with a Bidirectional Glenn Anastomosis
ORIGINAL ARTICLE The increase of the pulmonary blood flow inhigh-risk hypoxic patients with a bidirectional Glenn anastomosis Jacek Kołcz1, Mirosława Dudyńska2, Aleksandra Morka3, Sebastian Góreczny4, Janusz Skalski1 1Department of Pediatric Cardiac Surgery, Jagiellonian University Medical College, Kraków, Poland 2Department of Pediatric Cardiac Surgery, University Children’s Hospital in Krakow, Kraków, Poland 3Faculty of Health Sciences, Jagiellonian University Medical College, Kraków, Poland 4Department of Pediatric Cardiology, Jagiellonian University Medical College, Kraków, Poland Correspondence to: Jacek Kołcz, MD, PhD, ABSTRACT FECTS, Department of Pediatric Background: An additional shunt in single ventricle patients with Glenn anastomosis may increase Cardiac Surgery, pulmonary flow at the expense of ventricle volume overloading. The performance of the modification Jagiellonian University depends on pulmonary resistance, indicating better results in favorable hemodynamic conditions. Medical College, Wielicka 265, Aims: The study aims at analyzing the influence of precisely adjusted pulsatile shunt in borderline 30–663 Kraków, Poland, phone: +40 12 658 20 11, high-risk Glenn patients on early and late results. e-mail: Methods: The study involved 99 patients (including 21 children) with the bidirectional Glenn and ac- [email protected] cessory pulsatile shunt (BDGS group), and 78 patients with the classic bidirectional Glenn anastomosis Copyright by the Author(s), 2021 (BDG group). Kardiol Pol. 2021; Results: There was 1 death in the BDGS group and 4 deaths in the BDG group. No difference in mortality 79 (6): 638–644; DOI: 10.33963/KP.15939 (P = 0.71) was found. The Fontan completion was achieved in 69 (88.5%) children in the BDG group and Received: 18 (85.7%) patients in the BDGS group, without fatalities. -

A Better Approach for Left Ventricular Training In
Received: 28 September 2018 | Revised: 7 November 2018 | Accepted: 29 December 2018 DOI: 10.1111/chd.12749 ORIGINAL ARTICLE A better approach for left ventricular training in transposition of the great arteries and intact interventricular septum: Bidirectional cavopulmonary anastomosis and pulmonary artery banding Mehmet Salih Bilal MD1 | Arda Özyüksel MD1,2 | Mustafa Kemal Avşar MD1 | Şener Demiroluk MD3 | Osman Küçükosmanoğlu MD4 | Yalım Yalçın MD5 1Department of Cardiovascular Surgery, Medicana International Hospital, Abstract Istanbul, Turkey Objective: Management of the patients with transposition of the great arteries and 2 Department of Cardiovascular intact ventricular septum may be challenging beyond the newborn period. Herein, we Surgery, Biruni University, Istanbul, Turkey would like to present our alternative strategy for training the left ventricle in these 3Department of Anesthesiology, Medicana International Hospital, Istanbul, Turkey patients. 4Department of Pediatric Methods: Six patients with transposition of the great arteries and intact ventricular Cardiology, Medicana International Hospital, Istanbul, Turkey septum were evaluated in our clinic. Two of them were palliated with Glenn proce- 5Department of Pediatric dure and pulmonary banding as a definitive treatment strategy at other centers. Four Cardiology, Florence Nightingale Hospital, patients were operated on and a bidirectional cavopulmonary anastomosis in combi- Istanbul, Turkey nation with pulmonary artery banding was performed (stage‐1: palliation and ven- Correspondence tricular training) in our center. In four out of these six patients, arterial switch Arda Özyüksel, Department of Cardiovascular Surgery, Medicana operation was performed with takedown and direct re‐anastomosis of the superior International Hospital, Beylikdüzü Caddesi, vena cava to right atrium after an interstage period of 21‐30 months (stage‐2: ana- No:3, Beylikdüzü, Istanbul, Turkey. -

Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Pediatric Cardiovascular Arterial Switch Operation Surgery Surgical Solutions to Complex Problems Tom R. Karl, MS, MD The arterial switch operation is appropriate treatment for most forms of transposition of Andrew Cochrane, FRACS the great arteries. In this review we analyze indications, techniques, and outcome for Christian P.R. Brizard, MD various subsets of patients with transposition of the great arteries, including those with an intact septum beyond 21 days of age, intramural coronary arteries, aortic arch ob- struction, the Taussig-Bing anomaly, discordant (corrected) transposition, transposition of the great arteries with left ventricular outflow tract obstruction, and univentricular hearts with transposition of the great arteries and subaortic stenosis. (Tex Heart Inst J 1997;24:322-33) T ransposition of the great arteries (TGA) is a prototypical lesion for pediat- ric cardiac surgeons, a lethal malformation that can often be converted (with a single operation) to a nearly normal heart. The arterial switch operation (ASO) has evolved to become the treatment of choice for most forms of TGA, and success with this operation has become a standard by which pediatric cardiac surgical units are judged. This is appropriate, because without expertise in neonatal anesthetic management, perfusion, intensive care, cardiology, and surgery, consistently good results are impossible to achieve. Surgical Anatomy of TGA In the broad sense, the term "TGA" describes any heart with a discordant ven- triculoatrial (VA) connection (aorta from right ventricle, pulmonary artery from left ventricle). The anatomic diagnosis is further defined by the intracardiac fea- tures. Most frequently, TGA is used to describe the solitus/concordant/discordant heart. -

Norwood/Batista Operation for a Newborn with Dilated Myopathy of the Left Ventricle
612 Brief communications The Journal of Thoracic and Cardiovascular Surgery September 2000 NORWOOD/BATISTA OPERATION FOR A NEWBORN WITH DILATED MYOPATHY OF THE LEFT VENTRICLE Richard D. Mainwaring, MD, Regina M. Healy, BS, John D. Murphy, MD, and William I. Norwood, MD, PhD, Wilmington, Del Partial left ventriculectomy for dilated cardiomyopathy was contractile function. The variable results that have been first reported by Batista and associates1 in 1996. The rationale reported in the adult literature may reflect patient selection for this procedure is the increase in left ventricular cavity size according to the reversibility or recoverability of the underly- in the absence of compensatory left ventricular wall thickness ing disease process. that is observed in dilated cardiomyopathy. This combination Despite the substantial worldwide experience with the of factors results in an increase in wall stress per unit muscle Batista procedure in adult patients, there is limited experience mass, as predicted by the LaPlace equation. As wall stress with this procedure in children. The current case report increases, mechanical load eventually becomes nonsustain- describes the treatment of a patient in whom the diagnosis of able and contributes to further dilation of the ventricle. Partial dilated cardiomyopathy was made in utero. left ventriculectomy has been advocated as a method of Clinical summary. A female infant was recognized in restoring the balance between cavity size and wall thickness. utero as having a dilated, poorly functioning left ventricle. Fundamental to this concept is the assumption that the left Labor was induced at 36 weeks’ gestation, and she was deliv- ventricular muscle is intrinsically normal or has recoverable ered by normal, spontaneous, vaginal delivery. -

The Clinical Spectrum of Fontan-Associated Liver Disease: Results from a Prospective Multimodality Screening Cohort
Edinburgh Research Explorer The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort Citation for published version: Munsterman, ID, Duijnhouwer, AL, Kendall, TJ, Bronkhorst, CM, Ronot, M, van Wettere, M, van Dijk, APJ, Drenth, JPH & Tjwa, ETTL 2019, 'The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort', European Heart Journal, vol. 40, no. 13, pp. 1057–1068. https://doi.org/10.1093/eurheartj/ehy620 Digital Object Identifier (DOI): 10.1093/eurheartj/ehy620 Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: European Heart Journal General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 25. Sep. 2021 Title: The clinical spectrum of Fontan-Associated Liver Disease: results from a prospective multimodality screening cohort. Authors: I.D. Munsterman1, A.L. Duijnhouwer2, T.J. Kendall3, C.M. Bronkhorst4, M. Ronot5, M. van Wettere5, A.P.J. van Dijk2, J.P.H. Drenth1, E.T.T.L. Tjwa1 On behalf of the Nijmegen Fontan Initiative (A.P.J. -

ICD-10 Coordination and Maintenance Committee Agenda
DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare & Medicaid Services 7500 Security Boulevard Baltimore, Maryland 21244-1850 Agenda ICD-10 Coordination and Maintenance Committee Department of Health and Human Services Centers for Medicare & Medicaid Services CMS Auditorium 7500 Security Boulevard Baltimore, MD 21244-1850 ICD-10-PCS Topics March 7, 2017 Pat Brooks, CMS – Co -Chairperson Webcast and Dial-In Information The meeting will begin promptly at 9am ET and will be webcast. Toll-free dial-in access is available for participants who cannot join the webcast: Phone: 1-844-396-8222; Meeting ID: 909 233 082. We encourage you to join early, as the number of phone lines is limited. If participating via the webcast or dialing in you do NOT need to register on-line for the meeting. This meeting is being webcast via CMS at http://www.cms.gov/live/. By your attendance, you are giving consent to the use and distribution of your name, likeness and voice during the meeting. You are also giving consent to the use and distribution of any personally identifiable information that you or others may disclose about you during the meeting. Please do not disclose personal health information. Note: Proposals for diagnosis code topics are scheduled for March 8, 2017 and will be led by the Centers for Disease Control (CDC). Please visit CDCs website for the Diagnosis agenda located at the following address: http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm 1 Introductions and Overview Pat Brooks ICD-10-PCS Topics: 1. Cerebral Embolic Protection During Michelle Joshua Transcatheter Aortic Valve Replacement Alexandra Lansky, MD Pages 10-11 Professor of Medicine, Section of Cardiology Yale School of Medicine 2. -

Title of Thesis
Heart rate variability and pacemaker treatment in children with Fontan circulation Jenny Alenius Dahlqvist Department of Clinical Sciences, Pediatrics Department of Radiation Sciences Umeå 2019 This work is protected by the Swedish Copyright Legislation (Act 1960:729) Dissertation for PhD ISBN: 978-91-7855-007-4 ISSN: 0346-6612 New series no: 2022 Cover illustration: Sigge Mårtensgård Klüft, 6 years. Layout cover: Inhousebyrån, Umeå universitet. Electronic version available at: http://umu.diva-portal.org/ Printed by: UmU Print Service Umeå, Sweden 2019 1 To children with Fontan circulation Table of Contents Abstract ............................................................................................. 4 Background ............................................................................................................... 4 Aim ............................................................................................................................. 4 Methods ...................................................................................................................... 4 Results ........................................................................................................................ 4 Conclusions ................................................................................................................. 5 Abbreviations .................................................................................... 6 Original papers ................................................................................ -

Glenn Surgery: a Safe Procedure in the Path of Univentricular Correction
Boletín Médico del Hospital Infantil de México RESEARCH ARTICLE Glenn surgery: a safe procedure in the path of univentricular correction Guadalupe Hernández-Morales1*, Alejandro Bolio-Cerdán2, Sergio Ruiz-González2, Patricia Romero-Cárdenas2, and Miguel A. Villasís-Keever3 1Departamento de Cirugía Cardiaca en Pediatría, Hospital Militar de Especialidades de la Mujer y Neonatología; 2Departamento de Cirugía Cardiovascular, Hospital Infantil de México Federico Gómez; 3Unidad de Investigación en Epidemiología Clínica, Unidad Médica de Alta Especialidad, Hospital de Pediatría, Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social. Mexico City, Mexico Abstract Background: This study describes 35 years of experience in a tertiary care level hospital that treats cardiac patients with univentricular heart physiology who underwent Glenn surgery. Methods: The study consisted of a retrospective analysis of patients who underwent Glenn surgery, including variables related to pre-operative, intra-operative, and post-operative mor- bidity and mortality. Results: From 1980 to 2015, 204 Glenn surgeries were performed. The most common heart disease was tricuspid atresia IB (19.2%). In 48.1% of the cases, the procedure was performed with antegrade flow. A bilateral Glenn procedure was performed in 12.5% of the cases and 10.3% were carried out without using a cardiopulmonary bypass pump. Reported complications included infections, bleeding, arrhythmias, chylothorax, neurological alterations, and pleural effusion. The mortality rate was 2.9%. Conclusions: Glenn surgery is a palliative surgery with good results. It significantly improves patient quality of life over a long period until a total cavopulmonary shunt is performed. The complications observed are few, and the mortality rate is low. -

Palliative Arterial Switch Operation As an Alternative for Selected Cases
PALLIATIVE ARTERIAL SWITCH OPERATION AS AN ALTERNATIVE FOR SELECTED CASES: SINGLE CENTERS‘ EXPERIENCE AND MID TERM RESULTS Okan Yurdak¨ok1, Murat ¸Ci¸cek1, Oktay Korun1, Firat Altin1, Mehmet Bi¸cer2, Yasemin Altuntas1, Emine Hekim Yilmaz1, Ahmet Sasmazel1, and Numan Aydemir1 1Dr Siyami Ersek Thoracic and Cardiovascular Surgery Training and Research Hospital 2Kartal Kosuyolu Training and Research Hospital June 10, 2020 Abstract ABSTRACT Introduction and Objective: There are various management options for newborns with single ventricle physiol- ogy, ventriculoarterial discordance and subaortic stenosis (SOS), classically involving the early pulmonary banding and aortic arch repair, the restricted bulboventriculer foramen(BVF) enlargement or the Norwood and the Damus Kaye Stansel (DKS) procedures. The aim of this study is to evaluate the midterm results of our clinical experience with palliative arterial switch operation (pASO) for this subset of patients. Method: We hereby retrospectively evaluate the charts of patients going through pASO, as initial palliation through Fontan pathway, starting from 2014 till today. Results: 10 patients underwent an initial palliative arterial switch procedure. 8 of 10 patients survived the operation and discharged. 7 of 10 patients completed stage II and 1 patient reached the Fontan completion stage and the other six of ten (6/10) patients are doing well and waiting for the next stage of palliation. There are two mortalities in the series (2/10) and one patient lost to follow-up (1/10). Conclusions: The pASO can be considered as an alternative palliation option for patients with single ventricle physiology, transposition of the great arteries and systemic outflow obstruction. It not only preserves systolic and diastolic ventricular function, but also provides a superior anatomic arrangement for following stages.