Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Diastolic Clicks After the Fontan Procedure for Double
304 Br Heart J 1990;63:304-7 Early diastolic clicks after the Fontan procedure for double inlet left ventricle: anatomical and physiological correlates Br Heart J: first published as 10.1136/hrt.63.5.304 on 1 May 1990. Downloaded from Andrew N Redlngton, Kit-Yee Chan, Julene S Carvalho, Elliot A Shinebourne Abstract inlet ventricle with two atrioventricular M mode echocardiograms and simultan- valves. All had previously undergone a Fontan eous phonocardiograms were recorded type procedure with direct atriopulmonary in four patients with early diastolic anastomosis. In two patients a valved clicks on auscultation. All had double homograft was interposed between the right inlet left ventricle and had undergone atrium and pulmonary artery. Each patient the Fontan procedure with closure of the had the right atrioventricular valve closed by right atrioventricular valve orifice by an either a single or double layer of Dacron cloth artifical patch. The phonocardiogram sewn into the floor of the right atrium. The confirmed a high frequency sound main pulmonary artery was tied off in all. occurring 60-90 ms after aortic valve Cross sectional, M mode, and pulsed wave closure and coinciding with the time of Doppler echocardiograms with simultaneous maximal excursion of the atrioven- electrocardiogram and phonocardiogram were tricular valve patch towards the ven- recorded on a Hewlett-Packard 77020A tricular mass. One patient had coexist- ultrasound system. The phonocardiogram was ing congenital complete heart block. recorded over the point on the chest where the The M mode echocardiogram showed diastolic click was best heart on auscultation, i'reversed") motion of the patch towards usually in the fourth left intercostal space the right atrium during atrial contrac- close to the sternum. -
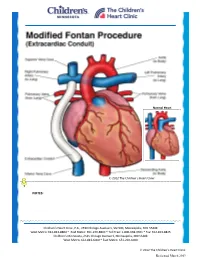
Modified Fontan Procedure: Extracardiac Conduit
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Modified Fontan Procedure: Extracardiac Conduit The Fontan procedure is usually the third procedure done in a series of surgeries to complete palliation of single ventricle patients. This procedure separates the “blue,” deoxygenated blood from the “red,” oxygenated blood circuit. Once the Fontan is done, deoxygenated blood drains passively to the pulmonary arteries, then to the lungs. Blood receives oxygen from the lungs and returns to the heart, where it is actively pumped out to the body. This procedure is usually done between 2-4 years of age. During surgery, the chest is opened through the previous incision, using a median sternotomy. The operation may or may not involve the use of cardiopulmonary bypass (heart-lung machine), depending on the surgical plan. A Gore-tex® tube graft (Gore) is cut to the appropriate length. An incision is made on the pulmonary artery near the area of the existing bidirectional Glenn shunt (cavopulmonary anastomosis) and the tube graft is sutured to the artery. Once that is complete, the inferior vena cava is divided from the atrium. The lower end of the Gore-tex® tube graft (Gore) is then sutured to the inferior vena cava. -

Median Sternotomy - Gold Standard Incision for Cardiac Surgeons
J Clin Invest Surg. 2016; 1(1): 33-40 doi: 10.25083/2559.5555.11.3340 Technique Median sternotomy - gold standard incision for cardiac surgeons Radu Matache1,2, Mihai Dumitrescu2, Andrei Bobocea2, Ioan Cordoș1,2 1Carol Davila University, Department of Thoracic Surgery, Bucharest, Romania 2Marius Nasta Clinical Hospital, Department of Thoracic Surgery, Bucharest, Romania Abstract Sternotomy is the gold standard incision for cardiac surgeons but it is also used in thoracic surgery especially for mediastinal, tracheal and main stem bronchus surgery. The surgical technique is well established and identification of the correct anatomic landmarks, midline tissue preparation, osteotomy and bleeding control are important steps of the procedure. Correct sternal closure is vital for avoiding short- and long-term morbidity and mortality. The two sternal halves have to be well approximated to facilitate healing of the bone and to avoid instability, which is a risk factor for wound infection. New suture materials and techniques would be expected to be developed to further improve the patients evolution, in respect to both immediate postoperative period and long-term morbidity and mortality Keywords: median sternotomy, cardiac surgeons, thoracic surgery, technique Acne conglobata is a rare, severe form of acne vulgaris characterized by the presence of comedones, papules, pustules, nodules and sometimes hematic or meliceric crusts, located on the face, trunk, neck, arms and buttocks.Correspondence should be addressed to: Mihai Dumitrescu; e-mail: [email protected] Case Report We report the case of a 16 year old Caucasian female patient from the urban area who addressed our dermatology department for erythematous, edematous plaques covered by pustules and crusts, located on the Radu Matache et al. -

The Physiology of the Fontan Circulation ⁎ Andrew Redington
Progress in Pediatric Cardiology 22 (2006) 179–186 www.elsevier.com/locate/ppedcard The physiology of the Fontan circulation ⁎ Andrew Redington Division of Cardiology, The Department of Pediatrics, The Hospital for Sick Children, University of Toronto School of Medicine, Toronto, Ontario, Canada Available online 8 September 2006 Abstract The Fontan circulation, no matter which of its various iterations, is abnormal in virtually every aspect of its performance. Some of these abnormalities are primarily the result of the procedure itself, and others are secondary to the fundamental disturbances of circulatory performance imposed by the ‘single’ ventricle circulation. The physiology of ventricular, systemic arterial and venopulmonary function will be described in this review. © 2006 Elsevier Ireland Ltd. All rights reserved. Keywords: palliation; Fontan circulation; Cavopulmonary anastomosis; Antriopulmonary anastomosis 1. Introduction has the profound consequences for the systemic ventricle that will discussed below. At the same time as the bidirectional In this personal overview, I will discuss the physiology of the cavopulmonary anastomosis was becoming almost uniformly Fontan circulation. Bob Freedom's contribution to our under- adopted, there was abandonment of the ‘classical’ atriopulmon- standing of complex congenital heart disease has meant that ary anastomosis, in favour of the total cavopulmonary con- many more of these patients are surviving with this physiology nection (TCPC). The ‘lateral wall’ TCPC, popularised by Marc than could have been contemplated 30 years ago. Nonetheless, deLeval [1], was shown experimentally and clinically to be they represent a very difficult group of patients and we continue haemodynamically more efficient [1,2] and set the scene for the to learn more about this unique circulation. -
Severe Aortic Stenosis and the Valve Replacement Procedure
Severe Aortic Stenosis and the Valve Replacement Procedure A Guide for Patients and their Families If you’ve been diagnosed with severe aortic stenosis, you probably have a lot of questions and concerns. The information in this booklet will help you learn more about your heart, severe aortic stenosis, and treatment options. Your heart team will recommend which treatment option is best for you. Please talk with them about any questions you have. Table of Contents 4 About Your Heart 5 What Is Severe Aortic Stenosis? 5 What Causes Severe Aortic Stenosis? 7 What Are the Symptoms of Severe Aortic Stenosis? 8 Treatment Options for Severe Aortic Stenosis 10 Before a TAVR Procedure 12 What Are the Risks of TAVR? 2 3 About Your Heart What Is Severe See the difference between healthy and The heart is a muscle about the size of your fist. It is a pump that works nonstop to Aortic Stenosis? diseased valves send oxygen-rich blood throughout your entire body. The heart is made up of four The aortic valve is made up of two or three chambers and four valves. The contractions (heartbeats) of the four chambers push Healthy Valve the blood through the valves and out to your body. tissue flaps, called leaflets. Healthy valves open at every heart contraction, allowing blood to flow forward to the next chamber, and then close tightly to prevent blood from backing Pulmonic controls the flow of Aortic controls the flow of blood up. Blood flows in one direction only. This is Valve blood to the lungs Valve out of your heart to the important for a healthy heart. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

A Common Occurrence After Coronary Bypass Surgery
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector lACC Vol. 15, No.6 1261 May 1990:1261-9 Acute Myocardial Dysfunction and Recovery: A Common Occurrence After Coronary Bypass Surgery WARREN M. BREISBLATT, MD, FACC, KEITH L. STEIN, MD, CYNTHIA J. WOLFE, RN, WILLIAM P. FOLLANSBEE, MD, FACC, JOHN CAPOZZI, CNMT, JOHN M. ARMITAGE, MD, ROBERT L. HARDESTY, MD, FACC Pittsburgh, Pennsylvania To evaluate whether acute myocardial dysfunction was min after coronary bypass and showed complete recovery common in the early postoperative period, serial hemody• within 48 h. Left ventricular end-systolic and end-diastolic namic measurements and radionuclide evaluation of ven• volume index increased significantly postoperatively, but tricular function were performed before and after opera• recovery in left ventricular ejection fraction was mostly due tion in 24 patients undergoing elective coronary bypass to decreases in end-systolic volume index (50 ± 22 ml at surgery. All patients had uncomplicated surgery, and no trough and 32 ± 16 ml at recovery). Depressed myocardial patient sustained an intraoperative infarction. In 96% of function was independent of bypass time, number of grafts patients, significant depression in right and left ventricular placed, preoperative medications or core temperatures ejection fraction was seen postoperatively, reaching a nadir postoperatively. Postoperative therapy with pressors or at 262 ± 116 min after coronary bypass. Left ventricular inotropic agents delayed but did -

Cardiopulmonary Bypass During Pregnancy: a Case Report
Cardiopulmonary Bypass During Pregnancy: A Case Report Robin G. Sutton and James P. Dearing Medical University of South Carolina Charleston, South Carolina Keywords: case report; pregnancy; technique, cardiopulmonary bypass Abstract _______________ diac operations in pregnant women. II% of the surveys returned included the use of cardiopulmonary bypass. (/. Extra-Corpor. Techno/ 20(2):67-71, 39 refer Our recent experience at the Medical University of ences) Reported cases of the pregnant patient dur South Carolina with a 21-year-old woman, with congen ing cardiopulmonary bypass are rare but not unique. ital aortic stenosis, who was in her second trimester of This case report of the pregnant patient during car pregnancy led us to this investigation of the literature. diopulmonary bypass is unique for two reasons. First, the patient was also a Jehovah's Witness and refused Normal Pregnancy blood products. Secondly, this case report provides Even in normal pregnancy there is an increased stress a literature review and specific cardiopulmonary on the heart. Starting from the 8th week of gestation, the bypass considerations pertinent to the perfusionist. blood volume begins to expand. By the 36th week, blood Recent literature reports that heart surgery is rel volume is increased to 35 percent above the non-preg atively safe during pregnancy. It is important to nant level. The plasma volume is increased by 40 percent monitor fetal heart rate during the procedure not whereas the red blood cell volume has only increased by 2 only to determine fetal distress but also to further 20 percent. By the end of the first trimester, the cardiac knowledge in the area by documenting effects. -

Closed Mitral Commissurotomy—A Cheap, Reproducible and Successful Way to Treat Mitral Stenosis
149 Editorial Closed mitral commissurotomy—a cheap, reproducible and successful way to treat mitral stenosis Manuel J. Antunes Clinic of Cardiothoracic Surgery, Faculty of Medicine, University of Coimbra, Coimbra, Portugal Correspondence to: Prof. Manuel J. Antunes. Faculty of Medicine, University of Coimbra, 3000-075 Coimbra, Portugal. Email: [email protected]. Provenance and Peer Review: This article was commissioned by the Editorial Office, Journal of Thoracic Disease. The article did not undergo external peer review. Comment on: Xu A, Jin J, Li X, et al. Mitral valve restenosis after closed mitral commissurotomy: case discussion. J Thorac Dis 2019;11:3659-71. Submitted Oct 23, 2019. Accepted for publication Nov 29, 2019. doi: 10.21037/jtd.2019.12.118 View this article at: http://dx.doi.org/10.21037/jtd.2019.12.118 In the August issue of the Journal, Xu et al. (1), from Bayley (4,5) and then became widely accepted. Subsequently, China, discuss the case of a patient who had a successful the technique of CMC suffered several modifications, both reoperation for restenosis of the mitral valve performed in the way the mitral valve was accessed and split. Several 30 years after closed mitral commissurotomy (CMC). instruments were created to facilitate the opening of the The specific aspects of this case were most appropriately commissures, culminating with the development of the commented by several experienced surgeons from different Tubbs dilator, which became the standard instrument for parts of the world. I was now invited by the Editor of this the procedure (Figure 1). Journal to write a Comment on this paper and its subject. -

Norwood/Batista Operation for a Newborn with Dilated Myopathy of the Left Ventricle
612 Brief communications The Journal of Thoracic and Cardiovascular Surgery September 2000 NORWOOD/BATISTA OPERATION FOR A NEWBORN WITH DILATED MYOPATHY OF THE LEFT VENTRICLE Richard D. Mainwaring, MD, Regina M. Healy, BS, John D. Murphy, MD, and William I. Norwood, MD, PhD, Wilmington, Del Partial left ventriculectomy for dilated cardiomyopathy was contractile function. The variable results that have been first reported by Batista and associates1 in 1996. The rationale reported in the adult literature may reflect patient selection for this procedure is the increase in left ventricular cavity size according to the reversibility or recoverability of the underly- in the absence of compensatory left ventricular wall thickness ing disease process. that is observed in dilated cardiomyopathy. This combination Despite the substantial worldwide experience with the of factors results in an increase in wall stress per unit muscle Batista procedure in adult patients, there is limited experience mass, as predicted by the LaPlace equation. As wall stress with this procedure in children. The current case report increases, mechanical load eventually becomes nonsustain- describes the treatment of a patient in whom the diagnosis of able and contributes to further dilation of the ventricle. Partial dilated cardiomyopathy was made in utero. left ventriculectomy has been advocated as a method of Clinical summary. A female infant was recognized in restoring the balance between cavity size and wall thickness. utero as having a dilated, poorly functioning left ventricle. Fundamental to this concept is the assumption that the left Labor was induced at 36 weeks’ gestation, and she was deliv- ventricular muscle is intrinsically normal or has recoverable ered by normal, spontaneous, vaginal delivery. -

Anomalies of the Aorta and Pulmonary Arteries Complicating Ventricular Septal Defect
Br Heart J: first published as 10.1136/hrt.24.3.279 on 1 May 1962. Downloaded from ANOMALIES OF THE AORTA AND PULMONARY ARTERIES COMPLICATING VENTRICULAR SEPTAL DEFECT BY J. MORGAN, R. PITMAN, J. F. GOODWIN, R. E. STEINER, AND A. HOLLMAN From the Departments of Medicine and Radiodiagnosis, Postgraduate Medical School and Hammersmith Hospital Received August 15, 1961 Ventricular septal defect is not always a simple lesion, but may be associated with other congenital cardiac disorders. The object of this paper is to present anomalies of the great vessels that have been found on angiocardiography or at operation in a series of patients with a ventricular septal defect investigated and treated at Hammersmith Hospital. During the last three years selective angiocardiography has been performed on 165 patients diagnosed as having ventricular septal defect. In 24 of them associated anomalies of the aorta and pulmonary arteries have been found. These patients will be presented in three groups according to the type of anomalies found; Group 1, corrected transposition of the great vessels, Group 2, double outlet right ventricle, Group 3, anomalies of the pulmonary arteries. 1. CORRECTED OF THE GREAT VESSELS GROUP TRANSPOSITION http://heart.bmj.com/ In this anomaly there is anatomical transposition. Viewed from above the aorta is anterior and to the left and the pulmonary trunk posterior and to the right. This is corrected functionally by bulboventricular inversion. Corrected transposition is usually associated with other defects, but the circulation is normal, for venous blood enters the pulmonary circulation and arterial blood the systemic circulation. The systemic ventricle from which the aorta arises has the anatomical features of a right ventricle, and the venous ventricle, from which the pulmonary artery arises, has the anatomical characteristics of a left ventricle. -

The Arterial Switch Operation for Transposition of the Great Arteries
The Arterial Switch Operation for Transposition of the Great Arteries Richard A. Jonas Transposition of the great arteries, together with tetral- Ijased on the fact that (luring fetal life hoth ventricles ogy of Fallot, is one of the most common congenital are exposed to the same pressure load. Thus, the left cardiac anomalies resulting in cyanosis. It is hardly ventricle is prepared at birth. However, hecause pulnio- surprising, therefore, that shortly after the introduc- nary resistance falls ra1)idlj within 6 to 8 weeks ancl tion of cardiopulmonary hypass in the early 195Os, perhaps as quicltly as within 2 to 4 weeks, the left attempts were made at anatomical correction of transpo- ventricle is no longer prepared. Iiitroduction of an sition, ie, the arterial switch procedure. These early essentially elective complex neonatal operation in 1983 attempts were uniformly unsuccessful for a number of initially met with consitlerahle resistance, particularly reasons : 1)ecause hy this time the surgical mortality for the atrial 1. Microvascular techniques were not adequately level procedures had reached very low levels. However, developed for delicate coronary artery transfer. a prospectivr study conducted Ijy the Congenital Heart 2. Pulmonary vascular disease is common in transpo- Surgeons Society‘ showed that the overall survival of an sition beyond the first year of life. entire population of patients with transposition en- 3. Surgeons failed to appreciate that in the presence rolled in the neonatal period was superior with the of an intact ventricular septum, the left ventricle was neonatal arterial switch approach because of the previ- inadequately prepared to acntely take over the pressure ously uncaptured deaths that occurred before atrial load of the systemic circulation.