Severe Aortic Stenosis and the Valve Replacement Procedure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Transcatheter Heart Valves
Corporate Medical Policy Surgical Management of Transcatheter Heart Valves File Name: surgica l_management_of_transcatheter_heart_valves Origination: 1/2011 Last CAP Review: 6/2021 Next CAP Review: 6/2022 Last Review: 6/2021 Description of Procedure or Service As the proportion of older adults increases in the U.S. population, the incidence of degenerative heart valve disease also increases. Aortic stenosis and mitra l regurgita tion are the most common valvular disorders in adults aged 70 years and older. For patients with severe valve disease, heart valve repair or replacement involving open heart surgery can improve functional status and qua lity of life. A variety of conventional mechanical and bioprosthetic heart valves are readily available. However, some individuals, due to advanced age or co-morbidities, are considered too high risk for open heart surgery. Alternatives to the open heart approach to heart valve replacement are currently being explored. Transcatheter heart valve replacement and repair are relatively new interventional procedures involving the insertion of an artificial heart valve or repair device using a catheter, rather than through open heart surgery, or surgical valve replacement (SAVR). The point of entry is typically either the femoral vein (antegrade) or femora l artery (retrograde), or directly through the myocardium via the apical region of the heart. For pulmonic and aortic valve replacement surgery, an expandable prosthetic heart valve is crimped onto a catheter and then delivered and deployed at the site of the diseased native valve. For valve repair, a small device is delivered by catheter to the mitral valve where the faulty leaflets are clipped together to reduce regurgitation. -

Blood Vessels
BLOOD VESSELS Blood vessels are how blood travels through the body. Whole blood is a fluid made up of red blood cells (erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma. It supplies the body with oxygen. SUPERIOR AORTA (AORTIC ARCH) VEINS & VENA CAVA ARTERIES There are two basic types of blood vessels: veins and arteries. Veins carry blood back to the heart and arteries carry blood from the heart out to the rest of the body. Factoid! The smallest blood vessel is five micrometers wide. To put into perspective how small that is, a strand of hair is 17 micrometers wide! 2 BASIC (ARTERY) BLOOD VESSEL TUNICA EXTERNA TUNICA MEDIA (ELASTIC MEMBRANE) STRUCTURE TUNICA MEDIA (SMOOTH MUSCLE) Blood vessels have walls composed of TUNICA INTIMA three layers. (SUBENDOTHELIAL LAYER) The tunica externa is the outermost layer, primarily composed of stretchy collagen fibers. It also contains nerves. The tunica media is the middle layer. It contains smooth muscle and elastic fiber. TUNICA INTIMA (ELASTIC The tunica intima is the innermost layer. MEMBRANE) It contains endothelial cells, which TUNICA INTIMA manage substances passing in and out (ENDOTHELIUM) of the bloodstream. 3 VEINS Blood carries CO2 and waste into venules (super tiny veins). The venules empty into larger veins and these eventually empty into the heart. The walls of veins are not as thick as those of arteries. Some veins have flaps of tissue called valves in order to prevent backflow. Factoid! Valves are found mainly in veins of the limbs where gravity and blood pressure VALVE combine to make venous return more 4 difficult. -

Surgery for Acquired Heart Disease
View metadata, citation and similar papers at core.ac.uk brought to you byCORE provided by Elsevier - Publisher Connector SURGERY FOR ACQUIRED HEART DISEASE EARLY RESULTS WITH PARTIAL LEFT VENTRICULECTOMY Patrick M. McCarthy, MD a Objective: We sought to determine the role of partial left ventriculectomy in Randall C. Starling, MD b patients with dilated cardiomyopathy. Methods: Since May 1996 we have James Wong, MBBS, PhD b performed partial left ventriculectomy in 53 patients, primarily (94%) in Gregory M. Scalia, MBBS b heart transplant candidates. The mean age of the patients was 53 years Tiffany Buda, RN a Rita L. Vargo, MSN, RN a (range 17 to 72 years); 60% were in class IV and 40% in class III. Marlene Goormastic, MPH c Preoperatively, 51 patients were thought to have idiopathic dilated cardio- James D. Thomas, MD b myopathy, one familial cardiomyopathy, and one valvular cardiomyopathy. Nicholas G. Smedira, MD a As our experience accrued we increased the extent of left ventriculectomy James B. Young, MD b and more complex mitral valve repairs. For two patients mitral valve replacement was performed. For 51 patients the anterior and posterior mitral valve leaflets were approximated (Alfieri repair); 47 patients also had ring posterior annuloplasty. In 27 patients (5!%) one or both papillary muscles were divided, additional left ventricular wall was resected, and the papillary muscle heads were reimplanted. Results: Echocardiography showed a significant decrease in left ventricular dimensions after resection (8.3 cm to 5.8 cm), reduction in mitral regurgitation (2.8+ to 0), and increase in forward ejection fraction (15.7% to 32.7%). -

Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Pediatric Cardiovascular Arterial Switch Operation Surgery Surgical Solutions to Complex Problems Tom R. Karl, MS, MD The arterial switch operation is appropriate treatment for most forms of transposition of Andrew Cochrane, FRACS the great arteries. In this review we analyze indications, techniques, and outcome for Christian P.R. Brizard, MD various subsets of patients with transposition of the great arteries, including those with an intact septum beyond 21 days of age, intramural coronary arteries, aortic arch ob- struction, the Taussig-Bing anomaly, discordant (corrected) transposition, transposition of the great arteries with left ventricular outflow tract obstruction, and univentricular hearts with transposition of the great arteries and subaortic stenosis. (Tex Heart Inst J 1997;24:322-33) T ransposition of the great arteries (TGA) is a prototypical lesion for pediat- ric cardiac surgeons, a lethal malformation that can often be converted (with a single operation) to a nearly normal heart. The arterial switch operation (ASO) has evolved to become the treatment of choice for most forms of TGA, and success with this operation has become a standard by which pediatric cardiac surgical units are judged. This is appropriate, because without expertise in neonatal anesthetic management, perfusion, intensive care, cardiology, and surgery, consistently good results are impossible to achieve. Surgical Anatomy of TGA In the broad sense, the term "TGA" describes any heart with a discordant ven- triculoatrial (VA) connection (aorta from right ventricle, pulmonary artery from left ventricle). The anatomic diagnosis is further defined by the intracardiac fea- tures. Most frequently, TGA is used to describe the solitus/concordant/discordant heart. -

Long-Term Outcomes of the Neoaorta After Arterial Switch Operation for Transposition of the Great Arteries Jennifer G
ORIGINAL ARTICLES: CONGENITAL HEART SURGERY CONGENITAL HEART SURGERY: The Annals of Thoracic Surgery CME Program is located online at http://cme.ctsnetjournals.org. To take the CME activity related to this article, you must have either an STS member or an individual non-member subscription to the journal. CONGENITAL HEART Long-Term Outcomes of the Neoaorta After Arterial Switch Operation for Transposition of the Great Arteries Jennifer G. Co-Vu, MD,* Salil Ginde, MD,* Peter J. Bartz, MD, Peter C. Frommelt, MD, James S. Tweddell, MD, and Michael G. Earing, MD Department of Pediatrics, Division of Pediatric Cardiology, and Department of Internal Medicine, Division of Cardiovascular Medicine, and Department of Cardiothoracic Surgery, Medical College of Wisconsin, Milwaukee, Wisconsin Background. After the arterial switch operation (ASO) score increased at an average rate of 0.08 per year over for transposition of the great arteries (TGA), the native time after ASO. Freedom from neoaortic root dilation at pulmonary root and valve function in the systemic posi- 1, 5, 10, and 15 years after ASO was 84%, 67%, 47%, and tion, and the long-term risk for neoaortic root dilation 32%, respectively. Risk factors for root dilation include -pre ,(0.003 ؍ and valve regurgitation is currently undefined. The aim history of double-outlet right ventricle (p and length of ,(0.01 ؍ of this study was to determine the prevalence and pro- vious pulmonary artery banding (p Neoaortic valve regurgitation of at .(0.04 ؍ gression of neoaortic root dilation and neoaortic valve follow-up (p regurgitation in patients with TGA repaired with the least moderate degree was present in 14%. -

Leapfrog Hospital Survey Hard Copy
Leapfrog Hospital Survey Hard Copy QUESTIONS & REPORTING PERIODS ENDNOTES MEASURE SPECIFICATIONS FAQS Table of Contents Welcome to the 2016 Leapfrog Hospital Survey........................................................................................... 6 Important Notes about the 2016 Survey ............................................................................................ 6 Overview of the 2016 Leapfrog Hospital Survey ................................................................................ 7 Pre-Submission Checklist .................................................................................................................. 9 Instructions for Submitting a Leapfrog Hospital Survey ................................................................... 10 Helpful Tips for Verifying Submission ......................................................................................... 11 Tips for updating or correcting a previously submitted Leapfrog Hospital Survey ...................... 11 Deadlines ......................................................................................................................................... 13 Deadlines for the 2016 Leapfrog Hospital Survey ...................................................................... 13 Deadlines Related to the Hospital Safety Score ......................................................................... 13 Technical Assistance....................................................................................................................... -

Evaluation of ECG Criteria for Left Ventricular Hypertrophy Before and After Aortic Valve Replacement Using Magnetic Resonance Imaging
MARCEL DEKKER, INC. • 270 MADISON AVENUE • NEW YORK, NY 10016 ©2003 Marcel Dekker, Inc. All rights reserved. This material may not be used or reproduced in any form without the express written permission of Marcel Dekker, Inc. JOURNAL OF CARDIOVASCULAR MAGNETIC RESONANCEw Vol. 5, No. 3, pp. 465–474, 2003 STRUCTURE AND FUNCTION Evaluation of ECG Criteria for Left Ventricular Hypertrophy Before and After Aortic Valve Replacement Using Magnetic Resonance Imaging Hugo P. Beyerbacht,1 Jeroen J. Bax,1,* Hildo J. Lamb,2 Arnoud van der Laarse,1 Hubert W. Vliegen,1 Albert de Roos,2 Aeilko H. Zwinderman,3 and Ernst E. van der Wall1 1Department of Cardiology, 2Department of Radiology, and 3Department of Medical Statistics, Leiden University Medical Centre, Leiden, The Netherlands ABSTRACT Purpose. Evaluation of different electrocardiographic criteria for left ventricular hypertrophy (ECG–LVH criteria) using left ventricular mass index (LVMI) determined by magnetic resonance imaging (MRI). In addition, the relation between LVMI regression after aortic valve replacement and corresponding ECG changes regarding LVH was studied. Methods. A group of 31 patients with severe aortic valve disease was studied to assess the presence of ECG–LVH and to measure LVMI and LV end-diastolic volume index (LVEDVI); 13 patients were restudied at 9.8 ^ 2.7 months after aortic valve replacement. Results. Three criteria had a sensitivity of 100% (SV1 þ RV5 or RV6 . 3.0 mV; SV1 or SV2 þ RV5 $ 3.5 mV; SV1 or SV2 þ RV5 or RV6 . 3.5 mV), at the cost of specificity (50%, 44.4% and 44.4%, respectively). -

Heart and Circulatory System Heart Chambers
160 Allen Street Rutland, Vermont 05701 www.rrmc.org 802.775.7111 Anatomy of the Heart Overview The heart is a muscular organ that pumps blood HEART AND throughout your body. It is positioned behind the CIRCULATORY SYSTEM lungs, slightly to the left side of the chest. Your heart is a bit larger than the size of your fist. Let's examine the structures of the heart and learn how blood travels through this complex organ. Right Side The heart is divided into two sides and four chambers. On the right side, blood that has already circulated through the body enters the heart through the superior vena cava and the inferior vena cava. The blood flows into the right atrium. When this chamber is full, the heart pushes the blood through the tricuspid valve and into the the next chamber - the right ventricle. From there, the blood is pushed out of the heart through the pulmonary valve. The blood travels through the pulmonary artery to the lungs, where it will pick up oxygen and give up carbon dioxide. HEART CHAMBERS Left Side On the left side of the heart, blood that has received oxygen from the lungs enters the heart through the pulmonary veins. The blood flows into the left atrium. It is pushed through the mitral valve into the left ventricle. Finally, it is pushed through the aortic valve and into the aorta. The aorta is the body's largest artery. It helps distribute the oxygen-rich Right Left blood throughout the body. Valves Now let's take a closer look at the valves. -

Avalus™ Pericardial Aortic Surgical Valve System
FACT SHEET Avalus™ Pericardial Aortic Surgical Valve System Aortic stenosis is a common heart problem caused by a narrowing of the heart’s aortic valve due to excessive calcium deposited on the valve leaflets. When the valve narrows, it does not open or close properly, making the heart work harder to pump blood throughout the body. Eventually, this causes the heart to weaken and function poorly, which may lead to heart failure and increased risk for sudden cardiac death. Disease The standard treatment for patients with aortic valve disease is surgical aortic valve Overview: replacement (SAVR). During this procedure, a surgeon will make an incision in the sternum to open the chest and expose the heart. The diseased native valve is then Aortic removed and a new artificial valve is inserted. Once in place, the device is sewn into Stenosis the aorta and takes over the original valve’s function to enable oxygen-rich blood to flow efficiently out of the heart. For patients that are unable to undergo surgical aortic valve replacement, or prefer a minimally-invasive therapy option, an alternative procedure to treat severe aortic stenosis is called transcatheter aortic valve replacement (TAVR). The Avalus Pericardial Aortic Surgical Valve System is a next- generation aortic surgical valve from Medtronic, offering advanced design concepts and unique features for the millions of patients with severe aortic stenosis who are candidates for open- heart surgery. The Avalus Surgical Valve The Avalus valve, made of bovine tissue, is also the only stented surgical aortic valve on the market that is MRI-safe (without restrictions) enabling patients with severe aortic stenosis who have the Avalus valve to undergo screening procedures for potential co-morbidities. -

Transcatheter Heart Valve Replacement
TRANSCATHETER ALI MASSUMI MD HEART VALVE NEIL E STRICKMAN MD REPLACEMENT 0 | P a g e Hall Garcia Cardiology Associates 6624 Fannin #2480 Houston, TX, USA 77030; +1-713-529-5530 ranscatheter Aortic Valve Replacement INTRODUCTION T The heart is a muscular organ located in your chest between your lungs which is designed to pump blood throughout the entire body. The right side of your heart pumps blood through the lungs, where the blood picks up oxygen. The left side of the heart receives this blood and pumps it to the rest of your body out through the AORTIC VALVE and into the circulation of the body. HEART CHAMBERS AND VALVES The heart is divided into four main areas, or chambers – two upper chambers (the left and right atrium) and two lower chambers (the left and right ventricle). These are the 4 valves which regulate the flow of blood through the heart, lungs and subsequently into the body’s circulation. They are called the aortic, mitral, pulmonary and tricuspid valves, whereas each is made of flaps of tissue called leaflets. See Figure 1 Figure 1 Hall Garcia Cardiology Associates 6624 Fannin #2480 Houston, TX, USA 77030; +1-713-529-5530 As the heart muscle contracts (squeezes), the valves open in one direction which allows the blood to circulate forward. When these valves close, the blood is prevented from flowing backward. There are 2 common problems that can develop in heart valves: VALVE STENOSIS This occurs when the valve is narrowed and does not completely open secondary to: o a build-up of calcium (mineral deposits) o high cholesterol (a waxy fat) o aging o genetics (such as a birth defect) VALVE INSUFFICIENCY / REGURGITATION This occurs when the valve does not fully close allowing blood to leak backward through the valve o Torn tendoniae (string-like architecture) o Ring dilation (degeneration like an automobile ring) AORTIC STENOSIS-(AS) Severe Aortic Valve Stenosis occurs when the narrowing of your aortic valve leaflets do not allow normal blood flow outward. -

Transcatheter Aortic Valve Replacement
What is TAVR? Cardiac Catheterization: Important things to know that will help you get ready Transcatheter Aortic Valve Replacement (TAVR) is a procedure Your doctor will tell if you need to stop eating or drinking to fix the aortic valve without taking out the old valve. A TAVR before your procedure. Your doctor also will tell you if you does not need open heart surgery and the heart does not need must stop taking any medications before the procedure. to be stopped. Catheterization Lab In the Pre-Operative (Pre-Op) Room before your The surgeon puts a catheter (thin tube) into an artery in your Cardiac Catheterization upper leg or through a small cut in your chest. The catheter will • You will wear a hospital gown. We will ask you to take off all Transcatheter Aortic Valve carry a new valve to your heart. your clothing (even underwear), jewelry, dentures, glasses, Replacement (TAVR) hearing aids, etc. • An intravenous line (IV) may be put into a vein in your arm • We will prepare and clean the catheter site (where the catheter goes into your body). We will clean your skin with a special wash that kills germs. We may need to trim body hair. • We will ask you to empty your bladder (pee) before your procedure After Your Cardiac Catheterization • You may be on bed rest (lying flat) for 2 to 6 hours. To lower the risk of bleeding, we do not want you to bend your body at the catheter site (where the catheter went into your body) • Your nurse will often check your vital signs (blood pressure, heart rate, temperature) and catheter site • You must use a urinal or bed pan until you can safely stand and walk to the bathroom • While you are healing, do not do strenuous exercise (such as running or lifting weights). -
How Your Heart Works
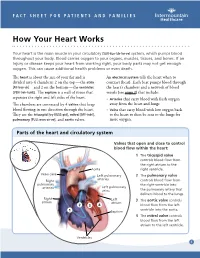
FACT SHEET FOR PATIENTS AND FAMILIES How Your Heart Works Your heart is the main muscle in your circulatory [SUR-kue-luh-tor-ee] system, which pumps blood throughout your body. Blood carries oxygen to your organs, muscles, tissues, and bones. If an injury or disease keeps your heart from working right, your body parts may not get enough oxygen. This can cause additional health problems or even death. The heart is about the size of your fist and is An electrical system tells the heart when to divided into 4 chambers: 2 on the top — the atria contract (beat). Each beat pumps blood through [AY-tree-uh] — and 2 on the bottom — the ventricles the heart’s chambers and a network of blood [VEN-treh-kuhlz]. The septum is a wall of tissue that vessels (see page 2) that include: separates the right and left sides of the heart. • Arteries that carry blood with fresh oxygen The chambers are connected by 4 valves that keep away from the heart and lungs blood flowing in one direction through the heart. • Veins that carry blood with low oxygen back They are the tricuspid [try-KUSS-pid], mitral [MY-truhl], to the heart to then be sent to the lungs for pulmonary [PULL-mon-air-ee], and aortic valves. more oxygen. Parts of the heart and circulatory system Valves that open and close to control blood flow within the heart: 1 The tricuspid valve controls blood flow from the right atrium to the Aorta right ventricle. Vena cava Left pulmonary 2 The pulmonary valve arteries Right controls blood flow from pulmonary the right ventricle into arteries Left pulmonary veins the pulmonary artery that delivers blood to the lungs.