Bicuspid Aortic Valve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Severe Aortic Stenosis and the Valve Replacement Procedure
Severe Aortic Stenosis and the Valve Replacement Procedure A Guide for Patients and their Families If you’ve been diagnosed with severe aortic stenosis, you probably have a lot of questions and concerns. The information in this booklet will help you learn more about your heart, severe aortic stenosis, and treatment options. Your heart team will recommend which treatment option is best for you. Please talk with them about any questions you have. Table of Contents 4 About Your Heart 5 What Is Severe Aortic Stenosis? 5 What Causes Severe Aortic Stenosis? 7 What Are the Symptoms of Severe Aortic Stenosis? 8 Treatment Options for Severe Aortic Stenosis 10 Before a TAVR Procedure 12 What Are the Risks of TAVR? 2 3 About Your Heart What Is Severe See the difference between healthy and The heart is a muscle about the size of your fist. It is a pump that works nonstop to Aortic Stenosis? diseased valves send oxygen-rich blood throughout your entire body. The heart is made up of four The aortic valve is made up of two or three chambers and four valves. The contractions (heartbeats) of the four chambers push Healthy Valve the blood through the valves and out to your body. tissue flaps, called leaflets. Healthy valves open at every heart contraction, allowing blood to flow forward to the next chamber, and then close tightly to prevent blood from backing Pulmonic controls the flow of Aortic controls the flow of blood up. Blood flows in one direction only. This is Valve blood to the lungs Valve out of your heart to the important for a healthy heart. -

Blood Vessels
BLOOD VESSELS Blood vessels are how blood travels through the body. Whole blood is a fluid made up of red blood cells (erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma. It supplies the body with oxygen. SUPERIOR AORTA (AORTIC ARCH) VEINS & VENA CAVA ARTERIES There are two basic types of blood vessels: veins and arteries. Veins carry blood back to the heart and arteries carry blood from the heart out to the rest of the body. Factoid! The smallest blood vessel is five micrometers wide. To put into perspective how small that is, a strand of hair is 17 micrometers wide! 2 BASIC (ARTERY) BLOOD VESSEL TUNICA EXTERNA TUNICA MEDIA (ELASTIC MEMBRANE) STRUCTURE TUNICA MEDIA (SMOOTH MUSCLE) Blood vessels have walls composed of TUNICA INTIMA three layers. (SUBENDOTHELIAL LAYER) The tunica externa is the outermost layer, primarily composed of stretchy collagen fibers. It also contains nerves. The tunica media is the middle layer. It contains smooth muscle and elastic fiber. TUNICA INTIMA (ELASTIC The tunica intima is the innermost layer. MEMBRANE) It contains endothelial cells, which TUNICA INTIMA manage substances passing in and out (ENDOTHELIUM) of the bloodstream. 3 VEINS Blood carries CO2 and waste into venules (super tiny veins). The venules empty into larger veins and these eventually empty into the heart. The walls of veins are not as thick as those of arteries. Some veins have flaps of tissue called valves in order to prevent backflow. Factoid! Valves are found mainly in veins of the limbs where gravity and blood pressure VALVE combine to make venous return more 4 difficult. -

Having an Echocardiogram to Screen for a Bicuspid Aortic Valve
Having an echocardiogram to screen for a bicuspid aortic valve UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is a bicuspid aortic valve? The aortic valve sits between the main chamber of the heart (the left ventricle) and the aorta. Its function is to ensure that blood flows correctly forward from the left ventricle into the aorta. Normally it has three thin leaflets which open as the heart contracts and then close to prevent back-flow of blood towards the ventricle. Aortic valve Tricuspid aortic valve (normal) Bicuspid aortic valve (abnormal) Some people may be born with an aortic valve made up of only 2 leaflets. The valve is then called bicuspid. This may cause problems with the functioning of the valve in that it may be more prone to gradually becoming narrowed or leaky. Sometimes a bicuspid valve may be associated with widening of the portion of the aorta that is connected to it. Widening of the aorta may occur in some relatives even if they have an aortic valve with 3 leaflets. If this widening is significant it is known as an aortic aneurysm. Is a bicuspid valve a common problem? Studies have suggested that this is not an uncommon valve problem and may occur in up to 1 in 200 people. 2 | PI18_1443_03 Having an echocardiogram to screen for a bicuspid aortic valve Recently there has been evidence that this condition may be genetic and thus have a tendency to run in a family. -
Echo in Asymptomatic Mitral and Aortic Regurgitation
2017 ASE Florida | Orlando, FL October 9, 2017 | 10:40 – 11:00 PM | 20 min | Grand Harbor Ballroom South Echo in Asymptomatic Mitral and Aortic Regurgitation Muhamed Sarić MD, PhD, MPA Director of Noninvasive Cardiology | Echo Lab Associate Professor of Medicine Disclosures Speakers Bureau (Philips, Medtronic) Advisory Board (Siemens) Regurgitation Axioms ▪Typically, regurgitation is NOT symptomatic unless severe ▪The opposite is not true: Severe regurgitation may be asymptomatic ▪ Chronic regurgitation leads to chamber dilatation on either side of the regurgitant valve Regurgitation Discovery ▪ Regurgitation as a anatomic entity was recognized in the 17th century ▪ Regurgitation was first clinically diagnosed by auscultation in the 19th century, well before the advent of echocardiography First Use of Regurgitation Term in English 1683 W. Charleton Three Anat. Lect. i. 18 Those [valves] that are placed in the inlet and outlet of the left Ventricle, to obviate the regurgitation of the bloud into the arteria venosa, and out of the aorta into the left Ventricle. Walter Charleton (1619 – 1707) English Physician Heart Murmur OXFORD ENGLISH DICTIONARY DEFINITION ▪ Any of various auscultatory sounds ▪ Adventitious sounds of cardiac or vascular origin [that is, separate from standard heart sounds: S1, S2, S3, S4] ▪ Sometimes of no significance ▪ But sometimes caused by valvular lesions of the heart or other diseases of the Στῆθος : Stēthos = chest circulatory system René Laënnec Stethoscope (1781 – 1826) (‘Chest examiner’) French Physician Hollow wooden cylinder Inventor of stethoscope in 1816 Laënnec Performing Auscultation Painted by Robert Alan Thom (1915 – 1979), American illustrator Commissioned by Parke, Davis & Co. 1816 1832 René Laënnec, James Hope French physician British physician Invents MONAURAL stethoscope separates MS from MR murmur 1852 1862 George Cammann Austin Flint Sr. -

Heart and Circulatory System Heart Chambers
160 Allen Street Rutland, Vermont 05701 www.rrmc.org 802.775.7111 Anatomy of the Heart Overview The heart is a muscular organ that pumps blood HEART AND throughout your body. It is positioned behind the CIRCULATORY SYSTEM lungs, slightly to the left side of the chest. Your heart is a bit larger than the size of your fist. Let's examine the structures of the heart and learn how blood travels through this complex organ. Right Side The heart is divided into two sides and four chambers. On the right side, blood that has already circulated through the body enters the heart through the superior vena cava and the inferior vena cava. The blood flows into the right atrium. When this chamber is full, the heart pushes the blood through the tricuspid valve and into the the next chamber - the right ventricle. From there, the blood is pushed out of the heart through the pulmonary valve. The blood travels through the pulmonary artery to the lungs, where it will pick up oxygen and give up carbon dioxide. HEART CHAMBERS Left Side On the left side of the heart, blood that has received oxygen from the lungs enters the heart through the pulmonary veins. The blood flows into the left atrium. It is pushed through the mitral valve into the left ventricle. Finally, it is pushed through the aortic valve and into the aorta. The aorta is the body's largest artery. It helps distribute the oxygen-rich Right Left blood throughout the body. Valves Now let's take a closer look at the valves. -

Avalus™ Pericardial Aortic Surgical Valve System
FACT SHEET Avalus™ Pericardial Aortic Surgical Valve System Aortic stenosis is a common heart problem caused by a narrowing of the heart’s aortic valve due to excessive calcium deposited on the valve leaflets. When the valve narrows, it does not open or close properly, making the heart work harder to pump blood throughout the body. Eventually, this causes the heart to weaken and function poorly, which may lead to heart failure and increased risk for sudden cardiac death. Disease The standard treatment for patients with aortic valve disease is surgical aortic valve Overview: replacement (SAVR). During this procedure, a surgeon will make an incision in the sternum to open the chest and expose the heart. The diseased native valve is then Aortic removed and a new artificial valve is inserted. Once in place, the device is sewn into Stenosis the aorta and takes over the original valve’s function to enable oxygen-rich blood to flow efficiently out of the heart. For patients that are unable to undergo surgical aortic valve replacement, or prefer a minimally-invasive therapy option, an alternative procedure to treat severe aortic stenosis is called transcatheter aortic valve replacement (TAVR). The Avalus Pericardial Aortic Surgical Valve System is a next- generation aortic surgical valve from Medtronic, offering advanced design concepts and unique features for the millions of patients with severe aortic stenosis who are candidates for open- heart surgery. The Avalus Surgical Valve The Avalus valve, made of bovine tissue, is also the only stented surgical aortic valve on the market that is MRI-safe (without restrictions) enabling patients with severe aortic stenosis who have the Avalus valve to undergo screening procedures for potential co-morbidities. -

Congenital Mitral Incompetence and Coarctation Ofaorta
Thorax: first published as 10.1136/thx.27.6.729 on 1 November 1972. Downloaded from Thorax (1972), 27, 729. Congenital mitral incompetence and coarctation of aorta Report of two cases treated surgically' ABDEL K. TERZAKI2, ROBERT D. LEACHMAN3, M. KHALIL ALI, GRADY L. HALLMAN, and DENTON A. COOLEY Department of Medicine and the Cora and Webb Mading Department of Surgery, Baylor University College of Medicine, and the Cardiology and Surgical Sections of the Texas Heart Institute of St. Luke's Episcopal and Texas Children's Hospitals, Houston, Texas, U.S.A. Two patients with congenital mitral incompetence and coarctation of the aorta are presented. One patient had associated patent ductus arteriosus, bicuspid aortic valve, and endocardial fibro- elastosis. The diagnosis in the two patients presented is well established by clinical, laboratory, and surgical findings and also by necropsy examination in one case. It is proposed that the rarity of reported cases in the literature may have resulted from the frequent diagnosis of left ventricular failure in infancy secondary to coarctation, leading to the assumption that a mitral insufficiency murmur, when present, is due to functional regurgitation. Likewise, the murmur may be mistakenly thought to originate from a ventricular septal defect. The diagnosis of coarctation of the aorta presented no problem in either patient, while detection of the mitral incompetence was difficult. Coarctation of the aorta complicated by copyright. pulmonary hypertension in the absence of intracardiac shunt should draw attention to the possi- bility of associated mitral incompetence. Congestive heart failure, especially after correction of coarctation, was also an indication of possible associated mitral insufficiency. -

Transcatheter Aortic Valve Replacement
What is TAVR? Cardiac Catheterization: Important things to know that will help you get ready Transcatheter Aortic Valve Replacement (TAVR) is a procedure Your doctor will tell if you need to stop eating or drinking to fix the aortic valve without taking out the old valve. A TAVR before your procedure. Your doctor also will tell you if you does not need open heart surgery and the heart does not need must stop taking any medications before the procedure. to be stopped. Catheterization Lab In the Pre-Operative (Pre-Op) Room before your The surgeon puts a catheter (thin tube) into an artery in your Cardiac Catheterization upper leg or through a small cut in your chest. The catheter will • You will wear a hospital gown. We will ask you to take off all Transcatheter Aortic Valve carry a new valve to your heart. your clothing (even underwear), jewelry, dentures, glasses, Replacement (TAVR) hearing aids, etc. • An intravenous line (IV) may be put into a vein in your arm • We will prepare and clean the catheter site (where the catheter goes into your body). We will clean your skin with a special wash that kills germs. We may need to trim body hair. • We will ask you to empty your bladder (pee) before your procedure After Your Cardiac Catheterization • You may be on bed rest (lying flat) for 2 to 6 hours. To lower the risk of bleeding, we do not want you to bend your body at the catheter site (where the catheter went into your body) • Your nurse will often check your vital signs (blood pressure, heart rate, temperature) and catheter site • You must use a urinal or bed pan until you can safely stand and walk to the bathroom • While you are healing, do not do strenuous exercise (such as running or lifting weights). -
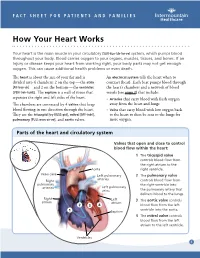
How Your Heart Works
FACT SHEET FOR PATIENTS AND FAMILIES How Your Heart Works Your heart is the main muscle in your circulatory [SUR-kue-luh-tor-ee] system, which pumps blood throughout your body. Blood carries oxygen to your organs, muscles, tissues, and bones. If an injury or disease keeps your heart from working right, your body parts may not get enough oxygen. This can cause additional health problems or even death. The heart is about the size of your fist and is An electrical system tells the heart when to divided into 4 chambers: 2 on the top — the atria contract (beat). Each beat pumps blood through [AY-tree-uh] — and 2 on the bottom — the ventricles the heart’s chambers and a network of blood [VEN-treh-kuhlz]. The septum is a wall of tissue that vessels (see page 2) that include: separates the right and left sides of the heart. • Arteries that carry blood with fresh oxygen The chambers are connected by 4 valves that keep away from the heart and lungs blood flowing in one direction through the heart. • Veins that carry blood with low oxygen back They are the tricuspid [try-KUSS-pid], mitral [MY-truhl], to the heart to then be sent to the lungs for pulmonary [PULL-mon-air-ee], and aortic valves. more oxygen. Parts of the heart and circulatory system Valves that open and close to control blood flow within the heart: 1 The tricuspid valve controls blood flow from the right atrium to the Aorta right ventricle. Vena cava Left pulmonary 2 The pulmonary valve arteries Right controls blood flow from pulmonary the right ventricle into arteries Left pulmonary veins the pulmonary artery that delivers blood to the lungs. -

Prevalence of Migraine Headaches in Patients with Congenital Heart Disease
Prevalence of Migraine Headaches in Patients With Congenital Heart Disease Tam Truong, MD, Leo Slavin, MD, Ramin Kashani, BA, James Higgins, MD, Aarti Puri, BS, Malika Chowdhry, BS, Philip Cheung, BS, Adam Tanious, BA, John S. Child, MD, FAHA, Joseph K. Perloff, MD, and Jonathan M. Tobis, MD* The prevalence of migraine headaches (MH) is 12% in the general population and increases to 40% in patients with patent foramen ovale. This study evaluated the prevalence of MH in patients with congenital heart disease (CHD). Of 466 patients contacted from the UCLA Adult Congenital Heart Disease Center, 395 (85%) completed a questionnaire to determine the prevalence of MH. Patients were stratified by diagnosis of right-to-left, left-to-right, or no shunt. A group of 252 sex-matched patients with acquired cardiovascular disease served as controls. The prevalence of MH was 45% in adults with CHD compared to 11% in the controls (p <0.001). Of the 179 patients with MH, 143 (80%) had migraines with aura and 36 (20%) had migraines without aura versus 36% and 64% observed in the controls (p <0.001). The frequency of MH was 52% in the right-to-left shunt group, 44% in the left-to-right, and 38% in the no ,NS). In patients with a right-to-left shunt who underwent surgical repair ؍ shunt group (p 47% had complete resolution of MH, whereas 76% experienced >50% reduction in headache days per month. In conclusion, the prevalence of MH in all groups of adults with CHD is 3 to 4 times more than a sex-matched control population, with increasing prevalence of MH in patients with no shunt, left-to-right, and right-to-left shunt. -

How Not to Miss a Bicuspid Aortic Valve in the Echocardiography Laboratory
ECHO ROUNDS Section Editor: E. Kenneth Kerut, M.D. How Not to Miss a Bicuspid Aortic Valve in the Echocardiography Laboratory Salvatore J. Tirrito, M.D.∗ and Edmund Kenneth Kerut, M.D.∗,† ∗Section of Cardiology, Tulane University Health Sciences Center, New Orleans, Louisiana †Heart Clinic of Louisiana, Marrero, Louisiana bicuspid aortic valve, echocardiography, congenital heart disease Diagnosis of bicuspid aortic valve (BAV) Address for correspondence and reprint requests: in the busy echocardiography laboratory is Salvatore J. Tirrito, M.D., Tulane University Health Sci- important, as it is a relatively common cardiac ences Center, Section of Cardiology SL-48, 1430 Tulane Av- enue, New Orleans, LA 71112. Fax: 504 529-9649; E-mail: congenital defect (up to 3% of the popula- 1 [email protected] tion), and requires a recommendation for Figure 1. M-mode and two-dimensional (2D) diastolic frame in the parasternal long-axis view of a bicuspid aortic valve with eccentric closure (arrows). Although not diagnostic, an eccentric line of closure should prompt one to evaluate the aortic valve closely for BAV. LA = left atrium. (Modified with permission from: Kerut EK, McIlwain, Plotnick: Handbook of Echo-Doppler Interpretation 2nd Ed, Blackwell Publishing, Elmsford, New York, 2004, p. 84) Vol. 22, No. 1, 2005 ECHOCARDIOGRAPHY: A Jrnl. of CV Ultrasound & Allied Tech. 53 TIRRITO AND KERUT Figure 2. Diastolic (left panel) and systolic (right panel) two-dimensional (2D) short-axis image of a BAV. In diastole the raphe may appear as a commissure (arrow), appearing to be a normal tri-leaflet valve. However,the systolic frame has a typical “fish-mouth” appearance. -

Symptomatic Presentations of Severe Aortic Stenosis
Precision and Future Medicine 2017;1(3):122-128 REVIEW https://doi.org/10.23838/pfm.2017.00156 ARTICLE pISSN: 2508-7940 · eISSN: 2508-7959 Symptomatic presentations of severe aortic stenosis Sung-Ji Park Division of Cardiology, Department of Internal Medicine, Cardiovascular Imaging Center, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea Received: August 2, 2017 Revised: September 12, 2017 Accepted: September 19, 2017 ABSTRACT Aortic stenosis (AS) is the most common type of valvular heart disease. A manifestation Corresponding author: Sung-Ji Park of ageing, the disorder is becoming more frequent as the average age of the population Division of Cardiology, increases. Onset of cardinal manifestation of AS—angina, syncope, and heart failure— Department of Internal remains the major demarcation point in the disease’s course. It has been well described Medicine, Cardiovascular that patients’ survival is limited once they develop symptoms from AS and survival after Imaging Center, Heart Vascular the onset of a symptom depends on what type of symptom a patient develops. Know- Stroke Institute, Samsung ing how the pathophysiology of AS causes typical symptoms and death is paramount to Medical Center, Sungkyunkwan understanding the disease. We discuss these issues in this review. University School of Medicine, 81 Irwon-ro, Gangnam-gu, Keywords: Aortic valve stenosis, Chest pain, Dyspnea, Echocardiography, syncope Seoul 06351, Korea Tel: +82-2-3410-3419 E-mail: [email protected] INTRODUCTION Aortic stenosis (AS) is the most common valvular heart disease in the elderly characterized by fixed aortic valve narrowing, left ventricular (LV) remodeling with hypertrophy, and progressive diastolic dysfunction [1].