Cutaneous Mastocytoma in Childhood: Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dermatofibrosarcoma Protuberans in a Male Infant
Pediatric Case Reports Dermatofibrosarcoma Protuberans in a Male Infant Leslie Peard, Nicholas G. Cost, and Amanda F. Saltzman Dermtofibrosarcoma protuberans is a rare cutaneous malignancy known to be locally aggressive. It is uncommonly seen in the pediatric population and can be difficult to distinguish from other benign skin lesions. We present a case of dermatofi- brosarcoma protuberans of the penis in a 6-month-old child managed with surgical resection. This case highlights the challenges of diagnosis of genital lesions in children and the complexities of genitourinary reconstruction following surgical resection. UROLOGY 129: 206−209, 2019. © 2018 Elsevier Inc. ermatofibrosarcoma protuberans (DFSP) is a and no frozen section was sent intraoperatively. The rare cutaneous malignancy with reported foreskin was not sent to pathology per institutional D annual incidence of 4.2 per million (0.3 to practice. 1.3 per million in pediatric patients) in the United Pathologic evaluation by a dermatopathologist revealed States. Patients are typically 20-50 years old. DFSP a CD34+ spindle cell neoplasm, favoring DFSP, with most commonly occurs on the trunk, and is very rarely involvement of deep and “lateral” margins (again, the found on the genitalia.1 To our knowledge, only four specimen was not orientated). FISH for the chromosomal cases of penile DFSP have been reported.2-4 The tumor translocation t(17,22) was negative. CT chest obtained is locally aggressive, with few reported cases of metas- for staging was negative for metastasis. After discussion at tasis.1 There is a paucity of data concerning character- multidisciplinary tumor board, options for management istics of disease and treatment strategies with only 2 proposed included Mohs surgery under local anesthesia by published guidelines available to guide management.5,6 dermatology versus wide local excision with frozen section We present a case of DFSP of the penis in an infant, under general anesthesia by urology. -
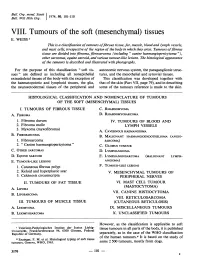
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Mast-Cell Tumors
Glendale Animal Hospital 623-934-7243 familyvet.com Mast-Cell Tumors Basics OVERVIEW • Cancerous (known as “malignant”) round cell tumor; round cell tumors are made up of cells that appear round or oval on microscopic examination; mast-cell tumors are one type of round cell tumor • Tumor arising from mast cells • “Cutaneous” refers to the skin • Mast cells are connective tissue cells that contain very dark granules; the granules contain various chemicals, including histamine; they are involved in immune reactions and inflammation; mast cells can be found in various tissues throughout the body • Mast-cell tumors in dogs are graded as well differentiated or low grade (Grade 1), intermediately differentiated (Grade 2), and poorly differentiated, undifferentiated or high grade (Grade 3); in general, the more differentiated the mast-cell tumor, the better the prognosis • Differentiation is a determination of how much a particular tumor cell looks like a normal cell; the more differentiated, the more like the normal cell • Mast-cell tumors of the skin in cats are classified as “compact” (more benign behavior) or “diffuse” (more undifferentiated and aggressive) • Mast-cell tumors are the most common cancerous (malignant) skin tumor in the dog • Mast-cell tumors also may be found in the tissue immediately beneath the skin (that is, the subcutis), spleen, liver, and intestines • Mast-cell tumors are the most common tumor found in the spleen of cats • Mast-cell tumors can release histamine, leading to the development of hives, reddening of the -

Dermatopathology
76A ANNUAL MEETING ABSTRACTS of the nodules aspirated was 1.8 (NNAN), 3.2 (HA), 3.0 (HCa) and 2.9 (PTC). The average numbers of nodules identified by US were 3.3 in NNAN, 2.0 in HA, 1.7 in HCa, Dermatopathology and 1.8 in PTC (p<0.05). Furthermore, 40% (4 of 10) and 20% (2 of 10) of HCa were vascularized and microcalcified on US, respectively; and 50% (7 of 14) of NNAN had 337 CD10 and Ep-CAM Expression in Basal Cell Carcinoma, Classical multiple (5) small nodules in the background thyroid. FNA Findings – the Hurthle cell Trichoepithelioma, and Desmoplastic Trichoepithelioma tumors had more cellular smears, discohesive Hurthle cells, few, if any, lymphocytes, TE Abbott, MD Cole, JW Patterson, MR Wick. University of Virginia Health System, and scarce or absent colloid in comparison to the smears from NNAN. Charlottesville, VA. Conclusions: Dominant thyroid nodules 2 cm or less on US without evidence of Background: The distinction between basal cell carcinoma (BCC) and increased vascularity or microcalcifications in combination with the background trichoepithelioma (TE) has historically been made on the basis of specific histologic thyroid containing multiple (3 or more) smaller nodules and the FNA smears containing criteria, but it may be difficult when the tumor sample is limited. Recent reports have some lymphoid aggregates with Hurthle cells in moderately sized sheets are likely to suggested a utility for CD10 and Ep-CAM immunostaining in recognizing BCC. be benign. Communication between clinician and pathologist correlating US and FNA Accordingly, this study was initiated in order to determine whether those markers findings in difficult cases may avoid unnecessary surgery. -

Serum Alpha-Fetoprotein Values in Dogs with Various Hepatic Diseases
Serum alpha-fetoprotein Values in Dogs with Various Hepatic Diseases Takatsugu YAMADA,1,2), Megumi FUJITA1), Satoshi KITAO3), Yoshinori ASHIDA1), Kazuya NISHIZONO1), Ryo TSUCHIYA1), Takuo SHIDA4), and Kousaku KOBAYASHI1) 1)Laboratory of Veterinary Internal Medicine and 4)Laboratory of Veterinary Radiology, School of Veterinary Medicine; 2)Research Institute of Bioscience, Azabu University, 1–17–71 Fuchinobe, Sagamihara, Kanagawa, 229–8501 and 3)Doubutsu Medical Center, 1–6–45 Nakahozumi, Ibaraki-shi, Osaka 567–0034, Japan (Received 2 December 1997/Accepted 10 February 1999) ABSTRACT. Serum alpha-fetoprotein (AFP) values were measured in hepatic diseased dogs with or without tumor and non-hepatic tumor bearing dogs by a sandwich ELISA using anti-dog AFP antiserum. Serum AFP values were less than 70 ng/ml in clinically healthy dogs. The values in dogs with hepatocellular carcinoma were higher than 1,400 ng/ml in 7 of 9 dogs, wherever those in two dogs with cholangiocarcinoma were in the normal range. Serum AFP values in hepatic diseased dogs without tumor were also high, however, the values were below 500 ng/ml in 90% of the dogs. In non-hepatic tumor dogs, serum AFP values were less than 500 ng/ml in 76% of the dogs. In the surgically removal cases with hepatocellular carcinoma, serum AFP values rapidly decreased. These results suggested that the sandwich ELISA using anti-dog AFP antiserum was an available method for diagnosis of hepatocellular carcinoma in dogs.—KEY WORDS: alpha-fetoprotein, canine, ELISA, tumor. J. Vet. Med. Sci. 61(6): 657–659, 1999 Serum alpha-fetoprotein (AFP) values have been used with hepatocellular carcinoma were also monitored AFP for the diagnosis of hepatocellular carcinoma [4, 5–6, 14] values after surgical removal of masses. -

Dermoscopic Features of Skin Lesions in Patients with Mastocytosis
STUDY Dermoscopic Features of Skin Lesions in Patients With Mastocytosis Sergio Vano-Galvan, MD, PhD; Iva´n A´ lvarez-Twose, MD; Elena De las Heras, MD, PhD; J. M. Morgado, Msc; Almudena Matito, MD; Laura Sa´nchez-Mun˜oz, MD, PhD; Maria N. Plana, MD, PhD; Pedro Jae´n, MD, PhD; Alberto Orfao, MD, PhD; Luis Escribano, MD, PhD Objectives: To evaluate dermoscopic features in a group factors for more symptomatic forms of the disease ac- of 127 patients with mastocytosis in the skin and to in- cording to the need for daily antimediator therapy. vestigate the relationship between different dermo- scopic patterns and other clinical and biological charac- Results: Four distinct dermoscopic patterns were ob- teristics of the disease. served: yellow-orange blot, pigment network, reticular vascular pattern, and (most frequently) light-brown blot. Design: Clinical and laboratory data were compared A reticular vascular pattern was identified in all telangi- among patients with mastocytosis grouped according to ectasia macular eruptiva and some maculopapular mas- the different dermoscopic patterns. tocytosis. In turn, all patients with mastocytoma dis- played the yellow-orange blot pattern. The reticular Setting: Patients were selected from the Instituto de Es- vascular dermoscopic pattern was associated with the need tudios de Mastocitosis de Castilla La Mancha and the De- for daily antimediator therapy; this pattern, together with partment of Dermatology of Hospital Universitario Ramo´n serum tryptase levels and plaque-type mastocytosis, rep- y Cajal from April 1 through September 30, 2009. resented the best combination of independent factors to predict the need for maintained antimediator therapy. -

The a Subunit of GTP-Binding Protein G0 in Neuroblastoma: Correlation with Advanced Disease Stage
[CANCER RESEARCH 54, 2334-2336, May 1, 19941 The a Subunit of GTP-binding Protein G0 in Neuroblastoma: Correlation with Advanced Disease Stage Yukio Ishiguro,' Kanefusa Kato, Tomiko Asano, Hiroshi Akatsuka, Hiroyuki Iwata, Fujio Ito, and Takahiro Ito Department ofSurgery, Branch Hospital ofNagoya University School ofMedicine, Daiko-minam4 Higashi-ku, Nagoya 461 [V. L, H. A., H. L, F. I., T. I.J, and Department of Biochemistry, Institute for Developmental Research, Aichi Prefectural Colony, Kamiya-cyo, Kasugai [K K, T. A.J, Japan ABSTRACT chemotherapy with cyclophosphamide and vincristine for 3 to 12 months. Stage III patients without recurrences (n = 5) had postoperative chemotherapy Tissue levels of the a subunit of G protein G0 (G0 a) were measured in for 2 years. Nine of 24 patients with distant metastases or recurrences had bone solid tumors from pediatric patients by immunoassay.G0 a concentra marrow transplants after complete clinical remissions. Survival time was tions were determined in the supernatant obtained by centrifugatlon of measured from the start of treatment. Diagnoses were confirmed histologically. tissue homogenates prepared in the presence (total G0 a) or absence of 2% Preparation of Tissue Extracts. Tissues were homogenized at 0°Cin 10 sodium cholate (soluble G0 a). Mean G0 a concentrations (total G0 a and volumes of 10 mM Tris-HCI (pH 7.5) containing 1 mM EDTA, using a soluble G0 a) in neuroblastomas (7 ganglioneuromas,13 ganglioneuro Polytron-type homogenizer. One-half of each homogenate was centrifuged at blastomas, and 50 neuroblastomas) were over 50-fold higher than those in 4°Cat 125,000 X g for 40 mm, and the supernatant was saved for G0 a other solidtumors from pediatric patients (n 13).Mean total G0a and analysis of the soluble fraction (soluble G0 a). -

Mast Cell Sarcoma: a Rare and Potentially Under
Modern Pathology (2013) 26, 533–543 & 2013 USCAP, Inc. All rights reserved 0893-3952/13 $32.00 533 Mast cell sarcoma: a rare and potentially under-recognized diagnostic entity with specific therapeutic implications Russell JH Ryan1, Cem Akin2,3, Mariana Castells2,3, Marcia Wills4, Martin K Selig1, G Petur Nielsen1, Judith A Ferry1 and Jason L Hornick2,5 1Pathology Service, Massachusetts General Hospital, and Harvard Medical School, Boston, MA, USA; 2Mastocytosis Center, Harvard Medical School, Boston, MA, USA; 3Department of Medicine, Harvard Medical School, Boston, MA, USA; 4Seacoast Pathology / Aurora Diagnostics, Exeter, NH and 5Department of Pathology, Brigham and Women’s Hospital, and Harvard Medical School, Boston, MA, USA Mast cell sarcoma is a rare, aggressive neoplasm composed of cytologically malignant mast cells presenting as a solitary mass. Previous descriptions of mast cell sarcoma have been limited to single case reports, and the pathologic features of this entity are not well known. Here, we report three new cases of mast cell sarcoma and review previously reported cases. Mast cell sarcoma has a characteristic morphology of medium-sized to large epithelioid cells, including bizarre multinucleated cells, and does not closely resemble either normal mast cells or the spindle cells of systemic mastocytosis. One of our three cases arose in a patient with a remote history of infantile cutaneous mastocytosis, an association also noted in one previous case report. None of our three cases were correctly diagnosed as mast cell neoplasms on initial pathological evaluation, suggesting that this entity may be under-recognized. Molecular testing of mast cell sarcoma has not thus far detected the imatinib- resistant KIT D816V mutation, suggesting that recognition of these cases may facilitate specific targeted therapy. -

Wt1 ペ プチドワクチン併用化学免疫療法とゲムシタビン+Cddp 治療の 第 I/Ii 相試験
第 29 回高度医療評価会議 資料1-3 平成 24 年2月3日 高度医療審査の照会事項(珠玖技術委員)に対する回答(1) 高度医療技術名:切除不能・再発胆道癌を対象としたゲムシタビン+CDDP+WT1 ペ プチドワクチン併用化学免疫療法とゲムシタビン+CDDP 治療の 第 I/II 相試験 2012/01/12 国立がん研究センター中央病院、奥坂 拓志 1.本臨床試験では、各症例での胆道癌に於ける WT1 抗原の発現の検討は行わ れないと理解します。 胆道癌に於ける WT1 抗原の発現増強症例の頻度について、これまでの自験 例、他験例のデータにつき示して下さい。 その際、既発表のものは、発表文献及び発現検討の手法についても記載し て下さい。 胆道がんにおける WT1 抗原の発現状況に関しては、Modern Pathology(2006)19,804-814 に記載されています。この中では、Polyclonal 抗 体(C-19)並びに単クローン抗体(6F-H2)を用いて、胆道がんにおける WT1 発 現を免疫組織化学的に解析しており、それぞれ 80%と 68%の症例で WT1 の発現 が確認されています。(参考文献1) 尚、WT1 の免疫染色方法・評価方法に関しては、標準化のための国際共同研究 が行われています。染色法・診断法の標準化が終われば、多施設間での客観的 評価が可能となると思われます。 2.胆道癌における HLA クラス 1 分子の発現消失及び減弱の頻度についての検 討及び報告につき、データと共に示して下さい。 胆道がんにおける HLA-ClassI の発現状態に関しては、Journal of Experimental & Clinical Cancer Research 2011,30:2 に記載されております。 この論文では、肝内胆管がんの 42.7%において HLA-ClassI の発現低下が認めら れたと報告されています。(参考文献2) 尚、この文献内の実験では、抗 HLA-ClassI 抗体として EMR8-5 が使用されて います。この抗体は、札幌医科大学にて開発されたものです。私どもは、同抗 体を用いた HLA-ClassI 免疫染色の標準化作業を進めており、ご指摘いただきま した質問に対する私ども独自の解析は、この標準化作業の中で実施する予定に していることを申し添えます。 第 29 回高度医療評価会議 資料1-3 平成 24 年2月3日 3.本臨床試験で用いられる WT1 ペプチド特異的なキラーT 細胞の胆道癌細胞に 対する反応性(細胞障害性を含む)の検討結果を示して下さい。 胆道がん細胞に対する WT1 ペプチド特異的なキラーT 細胞の反応性(細胞障害 活性)のデータは持ち合わせておりません。 同ペプチドを認識する、WT1 特異的 T 細胞からクローニングした TCR 遺伝子を 導入したリンパ球が、WT1 陽性膵がん細胞株に対する抗腫瘍効果をしめす結果は 報告されています。(参考文献3) また、今回使用する WT1 ペプチドにて培養した T リンパ球が、HLA 一致 WT1 陽 性造血器腫瘍株並びに肺がん細胞株に対して殺細胞効果を示すことも報告され ております。(参考文献4、5、6) ペプチド特異的リンパ球が、悪性腫瘍細胞を傷害するメカニズムは、基本的 には HLA-ClassI と 抗原の 発 現状況 に よると 考 えられ て いるこ と から、 HLA-ClassI を発現し WT1 を発現する胆道癌においても、同様の殺細胞効果が得 られると考えています。 4.WT1 抗原は、腫瘍化した腫瘍細胞に加えて、中皮細胞、腎蛸足細胞等の各種 -

Comprehensive Inherited Cancer Precision Panel Overview
Comprehensive Inherited Cancer Precision Panel Overview Hereditary cancer syndromes are encountered in all medical specialties. Although they account for about 5% of all malignancies, it is of special importance to identify these patients because, unlike patients with sporadic cancers, they require special, long-term care as their predisposition can cause them to develop certain tumors at a relatively early age. These cancers can arise in the lungs, kidneys, liver, pancreas, skin, eyes, heart. Most hereditary cancers are associated with a “germline mutation” that will be present in every cell of the human body. Identification of patients at risk of inherited cancer susceptibility is dependent upon the ability to characterize genes and alterations associated with increased cancer risk as well as gathering a detailed personal and family history aiding in the identification of the mode of inheritance as well as other family members at risk of suffering from this susceptibility. Most hereditary cancer syndromes follow an autosomal dominant inheritance, and the penetrance is high. The Igenomix Comprehensive Inherited Cancer Precision Panel provides a comprehensive analysis of the most common hereditary cancer syndromes using next-generation sequencing (NGS) to fully understand the spectrum of relevant cancer predisposition genes. Indications The Igenomix Comprehensive Inherited Caner Precision Panel is indicated as a screening and diagnostic test in those cases where there are: ‐ Multiple relatives on the same side of the family with the same or related forms of cancer ‐ Cancer at an early age ‐ Early presentation of an aggressive cancer type ‐ Multiple primary cancers in an individual 1 Clinical Utility The clinical utility of this panel is: ‐ Early and accurate genetic diagnosis allowing the most appropriate clinical management of a patient with personal or family history suggestive of a hereditary cancer syndrome. -

Tumour Antigens Recognized by T Lymphocytes: at the Core of Cancer Immunotherapy
PERSPECTIVES rejected by an immune response directed TIMELINE against new antigens that were different for every variant (tum– antigens). Remarkably, Tumour antigens recognized by mice that had rejected tum– variants were also protected against a subsequent injection of the parental tumour cells7, even though T lymphocytes: at the core of this teratocarcinoma was non-immunogenic, similar to the tumours that were described cancer immunotherapy by Hewitt. We concluded that an efficacious response against the tum– antigens had an Pierre G. Coulie, Benoît J. Van den Eynde, Pierre van der Bruggen additional effect: it triggered a response and Thierry Boon against antigens that were present on the original tumour but that were apparently Abstract | In this Timeline, we describe the characteristics of tumour antigens that non-immunogenic on their own. In col- are recognized by spontaneous T cell responses in cancer patients and the paths laboration with Hewitt, we treated cells from that led to their identification. We explain on what genetic basis most, but not all, spontaneous tumours with mutagens to – of these antigens are tumour specific: that is, present on tumour cells but not on obtain tum variants, and we observed that these variants were also capable of induc- normal cells. We also discuss how strategies that target these tumour-specific ing immune protection against the parental antigens can lead either to tumour-specific or to crossreactive T cell responses, tumours8. This showed that spontaneous which is an issue that has important safety implications in immunotherapy. mouse tumours do express tumour anti- These safety issues are even more of a concern for strategies targeting antigens gens, albeit poorly immunogenic ones. -

Canine Mast Cell Tumours: a Review of the Pathogenesis, Clinical Features, Pathology and Treatment
Welle, M M; Rohrer Bley, C; Howard, J; Rüfenacht, S (2008). Canine mast cell tumours: a review of the pathogenesis, clinical features, pathology and treatment. Veterinary Dermatology , (19):321-339. Postprint available at: http://www.zora.uzh.ch University of Zurich Posted at the Zurich Open Repository and Archive, University of Zurich. Zurich Open Repository and Archive http://www.zora.uzh.ch Originally published at: Veterinary Dermatology 2008, (19):321-339. Winterthurerstr. 190 CH-8057 Zurich http://www.zora.uzh.ch Year: 2008 Canine mast cell tumours: a review of the pathogenesis, clinical features, pathology and treatment Welle, M M; Rohrer Bley, C; Howard, J; Rüfenacht, S Welle, M M; Rohrer Bley, C; Howard, J; Rüfenacht, S (2008). Canine mast cell tumours: a review of the pathogenesis, clinical features, pathology and treatment. Veterinary Dermatology , (19):321-339. Postprint available at: http://www.zora.uzh.ch Posted at the Zurich Open Repository and Archive, University of Zurich. http://www.zora.uzh.ch Originally published at: Veterinary Dermatology 2008, (19):321-339. Canine mast cell tumours: a review of the pathogenesis, clinical features, pathology and treatment Abstract Mast cells (MCs) are well known for their neoplastic transformation in solitary and multiple cutaneous mast cell tumours (MCTs), as well as visceral and systemic mastocytosis. Dogs have an unique risk of developing cutaneous MCTs, and they account for 7% to 21% of all canine skin tumours. The aetiology of canine MCTs is unknown but is probably multi-factorial. This article reviews uptodate knowledge on the pathogenesis, the clinical presentation, the clinical prognostic factors, the diagnostic workup including clinical staging, cytological findings, histological findings and the various grading systems which have been evaluated based on morphology, the assessment of proliferation markers and other factors such as vessel density.