Comprehensive Inherited Cancer Precision Panel Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -
Fanconi Anemia: Guidelines for Diagnosis and Management
Fanconi Anemia: Guidelines for Diagnosis and Management Fourth Edition • 2014 We are deeply grateful to the following generous donors, who made this publication possible: Pat and Stephanie Kilkenny Phil and Penny Knight Disclaimer Information provided in this handbook about medications, treatments or products should not be construed as medical instruction or scientific endorsement. Always consult your physician before taking any action based on this information. copyright© 1999; second edition 2003; third edition 2008; fourth edition 2014 Fanconi Anemia: Guidelines for Diagnosis and Management Fourth Edition • 2014 Managing Editor: Laura Hays, PhD Editors: Dave Frohnmayer, JD, Lynn Frohnmayer, MSW, Eva Guinan, MD, Teresa Kennedy, MA, and Kim Larsen Scientific Writers: SciScripter, LLC These guidelines for the clinical care of Fanconi anemia (FA) were developed at a conference held April 5-6, 2013 in Herndon, VA. We owe a tremendous debt of gratitude to Eva Guinan, MD, for serving as moderator of the conference, as she did for the consensus conferences for the first three editions, and for her skill in helping the participants arrive at consensus. We would like to thank all the participants for donating their time and expertise to develop these guidelines. The names and contact information of all participants appear in the Appendix. These guidelines are posted on our Web site and are available from: Fanconi Anemia Research Fund, Inc. Phone: 541-687-4658 or 888-326-2664 (US only) 1801 Willamette Street, Suite 200 FAX: 541-687-0548 Eugene, Oregon 97401 E-mail: [email protected] Web site: www.fanconi.org Facebook: www.facebook.com/fanconianemiaresearchfund Twitter: https://twitter.com/FAresearchfund Material from this book may be reprinted with the permission of the Fanconi Anemia Research Fund, Inc. -

PTEN Mutations the PTEN Hamartoma Tumor Synd
Updated December 2019 (NCCN v1.2020) Cowden Syndrome/PTEN Hamartoma Tumor Syndrome: PTEN Mutations The PTEN Hamartoma Tumor Syndrome (PHTS) is a spectrum of highly variable conditions with overlapping features. This spectrum includes Cowden syndrome (CS), Bannayan-Riley-Ruvalcaba syndrome (BRRS), and PTEN-related autism spectrum disorder.1-3 The term PHTS describes any individual with a germline pathogenic PTEN mutation, regardless of their clinical presentation.4 PHTS is a multisystem syndrome primarily characterized by noncancerous (benign), tumor-like growths called hamartomas that can develop throughout the body. There is also an increased risk of adult-onset cancers.5 Cancer Risks and General Management Recommendations PTEN Mutation General Surveillance/Management Recommendations9 Carrier Cancer Population Risks2,4-8 Lifetime Cancer Risks Female Breast: 12.4% Surveillance Primary: 33-60% Breast awareness, including periodic, consistent breast self exams, Second Primary: starting at age 18 years 29% within 10 Clinical breast exam every 6-12 months starting at age 25 years, or 5- years10 10 years before the earliest breast cancer diagnosis in the family (whichever comes first) Annual mammogram with consideration of tomosynthesis and breast MRI with contrast at age 30-35 years, or 5-10 years before the earliest breast cancer diagnosis in the family (whichever comes first) Age >75 years: Management should be considered on an individual basis Surgery Discuss option of risk-reducing mastectomy, including degree of protection, reconstruction -

Review of Cancer Genetics
Review of Cancer Genetics Genes are pieces of information in the cells that make up the body. Cells are the basic units of life. Normally, cells grow, divide and make more cells in a controlled way as the body needs them to stay healthy. Cancer happens when a cell grows out of control in an abnormal way. All cancer is caused by a buildup of mutations (changes) in specific genes. Normally, these genes help the cell grow and divide in a controlled manner. The mutation in the gene damages this process and, as a result, the cell can grow out of control and become cancer. In most people who have cancer, the gene mutations that lead to their cancer cannot be passed on to their children. However, some families have a gene mutation that can get passed on from one generation to another. The differences between sporadic (non-hereditary) and hereditary forms of cancer are reviewed below. Additionally, some families have more cancer than would be expected by chance, but the cancer does not seem to be hereditary. This “familial” form of cancer is also discussed below. Sporadic Cancer Most cancer – 75% to 80% – is sporadic. In sporadic cancer, the gene mutations that cause the cancer are acquired (occur only in the tumor cells) and are not inherited. Risk for acquired gene mutations increases with age and is often influenced by environmental, lifestyle or medical factors. Cancer can sometimes happen by chance. Everyone has some risk of developing cancer in his or her lifetime. Because cancer is common, it is possible for a family to have more than one member who has cancer by chance. -

Piggybac Mutagenesis and Exome Sequencing Identify Genetic Driver
Noorani et al. Genome Biology (2020) 21:181 https://doi.org/10.1186/s13059-020-02092-2 RESEARCH Open Access PiggyBac mutagenesis and exome sequencing identify genetic driver landscapes and potential therapeutic targets of EGFR-mutant gliomas Imran Noorani1,2* , Jorge de la Rosa1†, Yoon Ha Choi1,3†, Alexander Strong1, Hannes Ponstingl1, M. S. Vijayabaskar1, Jusung Lee3, Eunmin Lee3, Angela Richard-Londt4, Mathias Friedrich1,5, Federica Furlanetto5, Rocio Fuente1, Ruby Banerjee1, Fengtang Yang1, Frances Law1, Colin Watts2,6, Roland Rad5, George Vassiliou1, Jong Kyoung Kim3, Thomas Santarius2, Sebastian Brandner4 and Allan Bradley1* * Correspondence: [email protected]; [email protected] Abstract †Jorge de la Rosa and Yoonha Choi contributed equally to this work. Background: Glioma is the most common intrinsic brain tumor and also occurs in 1The Wellcome Trust Sanger the spinal cord. Activating EGFR mutations are common in IDH1 wild-type gliomas. Institute, Wellcome Trust Genome However, the cooperative partners of EGFR driving gliomagenesis remain poorly Campus, Hinxton, Cambridgeshire CB10 1SA, UK understood. Full list of author information is Results: We explore EGFR-mutant glioma evolution in conditional mutant mice by available at the end of the article whole-exome sequencing, transposon mutagenesis forward genetic screening, and transcriptomics. We show mutant EGFR is sufficient to initiate gliomagenesis in vivo, both in the brain and spinal cord. We identify significantly recurrent somatic alterations in these gliomas including mutant EGFR amplifications and Sub1, Trp53, and Tead2 loss-of-function mutations. Comprehensive functional characterization of 96 gliomas by genome-wide piggyBac insertional mutagenesis in vivo identifies 281 known and novel EGFR-cooperating driver genes, including Cdkn2a, Nf1, Spred1, and Nav3. -

PIGMENT CELL & MELANOMA Research
The official journal of INTERNATIONAL FEDERATION OF PIGMENT CELL SOCIETIES · SOCIETY FOR MELANOMA RESEARCH PIGMENT CELL & MELANOMA Research Hearing dysfunction in heterozygous Mitf Mi-wh/+ mice, a model for Waardenburg syndrome type 2 and Tietz syndrome Christina Ni, Deming Zhang, Lisa A. Beyer, Karin E. Halsey, Hideto Fukui, Yehoash Raphael, David F. Dolan and Thomas J. Hornyak DOI: 10.1111/pcmr.12030 Volume 26, Issue 1, Pages 78-87 If you wish to order reprints of this article, please see the guidelines here Supporting Information for this article is freely available here EMAIL ALERTS Receive free email alerts and stay up-to-date on what is published in Pigment Cell & Melanoma Research – click here Submit your next paper to PCMR online at http://mc.manuscriptcentral.com/pcmr Subscribe to PCMR and stay up-to-date with the only journal committed to publishing basic research in melanoma and pigment cell biology As a member of the IFPCS or the SMR you automatically get online access to PCMR. Sign up as a member today at www.ifpcs.org or at www.societymelanomaresarch.org To take out a personal subscription, please click here More information about Pigment Cell & Melanoma Research at www.pigment.org Pigment Cell Melanoma Res. 26; 78–87 ORIGINAL ARTICLE Hearing dysfunction in heterozygous Mitf Mi-wh/+ mice, a model for Waardenburg syndrome type 2 and Tietz syndrome Christina Ni1, Deming Zhang1, Lisa A. Beyer2, Karin E. Halsey2, Hideto Fukui2, Yehoash Raphael2, David F. Dolan2 and Thomas J. Hornyak1,3,4 1 Dermatology Branch, Center for Cancer -

Hereditary Breast and Ovarian Cancer Syndrome
Page 1 of 4 Hereditary Breast and Ovarian Cancer Syndrome Hereditary breast and/or ovarian cancer (HBOC) is an autosomal dominant cancer susceptibility syndrome, most commonly associated with an inherited BRCA1 or BRCA2 gene mutation. Approximately 1 in 300 to 1 in 400 people in the general population are born with an inherited mutation in either the BRCA1 or BRCA2 genes. The frequency of BRCA1 or BRCA2 gene mutations is approximately 1 in 40 for people with Ashkenazi Jewish heritage. Other high-risk genes associated with hereditary breast and/or ovarian cancers include: PALB2, TP53, PTEN, STK11, CDH1. Additional genes may also be discussed in the context of Hereditary Cancer Program assessment. Confirmation of HBOC is important both for people with cancer, because of the associated risk for another cancer, and to inform appropriate cancer risk management for their adult family members. Note to oncologists/GPOs: if your regular practice includes women who are eligible for BRCA1/BRCA2 testing, we offer training to prepare you to initiate genetic testing for patients whose personal history meets specific criteria. Please contact the Hereditary Cancer Program’s Clinical Coordinator (604-877- 6000 local 672198) if you are interested in this oncology clinic based genetic testing (GENONC) process. Referral Criteria Notes: 1. breast cancer includes DCIS (ductal carcinoma in situ) and excludes LCIS (lobular carcinoma in situ) 2. ovarian cancer refers to invasive non-mucinous epithelial ovarian cancer; includes cancer of the fallopian tubes, primary peritoneal cancer and STIC (serous tubal intraepithelial carcinoma); excludes borderline/LMP ovarian tumours 3. close relatives include: children, brothers, sisters, parents, aunts, uncles, grandchildren & grandparents on the same side of the family. -

Genitourinary Pathology (Including Renal Tumors)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS GENITOURINARY PATHOLOGY (INCLUDING RENAL TUMORS) (776-992) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -
Homologous Recombination Deficiency: Exploiting the Fundamental Vulnerability of Ovarian Cancer
Published OnlineFirst October 13, 2015; DOI: 10.1158/2159-8290.CD-15-0714 Review Homologous Recombination Deficiency: Exploiting the Fundamental Vulnerability of Ovarian Cancer Panagiotis A. Konstantinopoulos1,2, Raphael Ceccaldi2,3, Geoffrey I. Shapiro2,4, and Alan D. D’Andrea2,3 AbstAt R c Approximately 50% of epithelial ovarian cancers (EOC) exhibit defective DNA repair via homologous recombination (HR) due to genetic and epigenetic alterations of HR pathway genes. Defective HR is an important therapeutic target in EOC as exemplified by the efficacy of platinum analogues in this disease, as well as the advent of PARP inhibitors, which exhibit synthetic lethality when applied to HR-deficient cells. Here, we describe the genotypic and phenotypic characteristics of HR-deficient EOCs, discuss current and emerging approaches for targeting these tumors, and present challenges associated with these approaches, focusing on development and over- coming resistance. Significance: Defective DNA repair via HR is a pivotal vulnerability of EOC, particularly of the high- grade serous histologic subtype. Targeting defective HR offers the unique opportunity of exploiting molecular differences between tumor and normal cells, thereby inducing cancer-specific synthetic lethality; the promise and challenges of these approaches in ovarian cancer are discussed in this review. Cancer Discov; 5(11); 1137–54. ©2015 AACR. iNtRODUctiON of achieving almost double the overall response rates and number of complete responses compared with nonplatinum Epithelial ovarian cancer (EOC) remains the most lethal agents (5, 6). Since then, platinum agents (initially cisplatin, gynecologic malignancy and the fifth most frequent cause then carboplatin, which is better tolerated but equally effec- of cancer-related mortality in women in the United States tive; ref. -

Dermatofibrosarcoma Protuberans in a Male Infant
Pediatric Case Reports Dermatofibrosarcoma Protuberans in a Male Infant Leslie Peard, Nicholas G. Cost, and Amanda F. Saltzman Dermtofibrosarcoma protuberans is a rare cutaneous malignancy known to be locally aggressive. It is uncommonly seen in the pediatric population and can be difficult to distinguish from other benign skin lesions. We present a case of dermatofi- brosarcoma protuberans of the penis in a 6-month-old child managed with surgical resection. This case highlights the challenges of diagnosis of genital lesions in children and the complexities of genitourinary reconstruction following surgical resection. UROLOGY 129: 206−209, 2019. © 2018 Elsevier Inc. ermatofibrosarcoma protuberans (DFSP) is a and no frozen section was sent intraoperatively. The rare cutaneous malignancy with reported foreskin was not sent to pathology per institutional D annual incidence of 4.2 per million (0.3 to practice. 1.3 per million in pediatric patients) in the United Pathologic evaluation by a dermatopathologist revealed States. Patients are typically 20-50 years old. DFSP a CD34+ spindle cell neoplasm, favoring DFSP, with most commonly occurs on the trunk, and is very rarely involvement of deep and “lateral” margins (again, the found on the genitalia.1 To our knowledge, only four specimen was not orientated). FISH for the chromosomal cases of penile DFSP have been reported.2-4 The tumor translocation t(17,22) was negative. CT chest obtained is locally aggressive, with few reported cases of metas- for staging was negative for metastasis. After discussion at tasis.1 There is a paucity of data concerning character- multidisciplinary tumor board, options for management istics of disease and treatment strategies with only 2 proposed included Mohs surgery under local anesthesia by published guidelines available to guide management.5,6 dermatology versus wide local excision with frozen section We present a case of DFSP of the penis in an infant, under general anesthesia by urology. -

E S P C R B U L L E T
E S P C R B U L L E T I N N° 54 April 2006 PUBLISHED BY THE EUROPEAN SOCIETY FOR PIGMENT CELL RESEARCH EDITOR: G. GHANEM (Brussels) INTERNATIONAL F. BEERMANN (Lausanne), J. BOROVANSKY (Prague), M. d’ISCHIA (Naples), JC GARCIA-BORRON (Murcia), , A. NAPOLITANO (Naples), M. PICARDO (Rome), N. SMIT (Leiden). EDITORIAL BOARD: R. MORANDINI (Brussels) Ed Ph In La stitu bor one ito 7. 3. 5. 2. 4. 8. 1. Review oftheliterature communications, ... Discussion, Letterstotheeditor,Reviews,Short CONTENTS Announcements andrelatedactivities 9. Melanomaexperime 6. ria at : t J.Bo 32 ory of Genetics, molecularand Neur Photobiology MSH, MCH,ot Melanosomes Tyrosinase, TRPs,otherenzymes l (DrA.Napolitano) Biology ofpigmentcells Chemistr Office (Dr M.Picardo) (Dr F.Beermann) (Prof JC.Garcia-Borron) - 2 - rdet, Ru 5 Onc 41 omel : .3 G. G o 2. l o 9 e Hég gy a 6 h y ofM a ani F n e n a e m d x: r-Bo Experi (Ed n (DrN.S 3 (Pro s 2 rd (ProfM.d'Ischia) - her hor ito 2 e et 1,B–10 - 5 r) me l a 41 , f J.Bo nt ni C. Meunier .3 al ntal 3. ns andot S 4 m mones u 9 rg 00 developmentalbiology , cellcult it) ery ro and pigmentarydisorders Bru , R. M ( van E-M L s sels, . O (DrR.Morandini) BULLETI R P S E her o .C a r sky i a . Belg l E : ndini g .) pi g ur , h ) ium. Uni a ( e gments n P e versi m ro @ duc u t é l t b Li i on Te . -
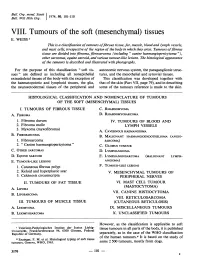
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI.