Dermatopathology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lessons from the African Teledermatology Project
Report The role of dermatopathology in conjunction with teledermatology in resource-limited settings: lessons from the African Teledermatology Project Matthew W. Tsang1, MD, MSt, and Carrie L. Kovarik2, MD 1Department of Dermatology, University Abstract of Minnesota, Minneapolis, MN, USA, Background Access to dermatology and dermatopathology services is scarce in 2 and, Departments of Dermatology and sub-Saharan Africa. Teledermatology provides consultations for healthcare providers in Internal Medicine, University of resource-limited settings where specialty medical services are difficult to obtain, and the Pennsylvania, Division of Infectious Diseases, Philadelphia, PA, USA African Teledermatology Project has helped to bridge the gap in dermatological care in Africa. This program also allows for biopsy specimens to be sent to the USA for processing Correspondence in cases where the clinical diagnosis is difficult and definitive diagnosis has implications for Carrie Kovarik, MD patient management. This study characterizes conditions diagnosed through clinicopatho- Assistant Professor logical correlation in conjunction with photos and tissue submitted to the African Dermatology, Dermatopathology, and Infectious Diseases Teledermatology Project. University of Pennsylvania Materials and methods Retrospective case review of tissue specimens submitted over 2 Maloney Building three years. 3600 Spruce Street Results Fifty-five biopsy specimens met inclusion criteria and represent cases of Philadelphia, PA 19104 malignancy (35%), infection (7%), suspected infection (15%), lichenoid tissue reaction E-mail: [email protected] (5%), dermatitis (15%), and other various conditions (18%). Three biopsy specimens were Funding sources: None. non-diagnostic (5%). Clinicopathological concordance between submitting clinician and Disclosures: The authors have no biopsy results occurred in 32 out of 55 cases (58%). -

Artificial Intelligence in Dermatopathology
Review Artificial Intelligence in Dermatopathology: New Insights and Perspectives Gerardo Cazzato 1,* , Anna Colagrande 1, Antonietta Cimmino 1, Francesca Arezzo 2, Vera Loizzi 2 , Concetta Caporusso 1, Marco Marangio 3, Caterina Foti 4, Paolo Romita 4, Lucia Lospalluti 4, Francesco Mazzotta 5, Sebastiano Cicco 6 , Gennaro Cormio 2 , Teresa Lettini 1 , Leonardo Resta 1 , Angelo Vacca 6 and Giuseppe Ingravallo 1,* 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (A.C.); [email protected] (A.C.); [email protected] (C.C.); [email protected] (T.L.); [email protected] (L.R.) 2 Section of Ginecology and Obstetrics, Department of Biomedical Sciences and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (F.A.); [email protected] (V.L.); [email protected] (G.C.) 3 Section of Informatics, University of Salento, 73100 Lecce, Italy; [email protected] 4 Section of Dermatology, Department of Biomedical Science and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (C.F.); [email protected] (P.R.); [email protected] (L.L.) 5 Pediatric Dermatology and Surgery Outpatients Department, Azienda Sanitaria Locale Barletta-Andria-Trani, 76123 Andria, Italy; [email protected] 6 Section of Internal Medicine, Department of Biomedical Sciences and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (S.C.); [email protected] (A.V.) * Correspondence: [email protected] (G.C.); [email protected] (G.I.) Citation: Cazzato, G.; Colagrande, A.; Abstract: In recent years, an increasing enthusiasm has been observed towards artificial intelligence Cimmino, A.; Arezzo, F.; Loizzi, V.; and machine learning, involving different areas of medicine. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Adenomatoid Tumor of the Skin: Differential Diagnosis of an Umbilical Erythematous Plaque
Title: Adenomatoid tumor of the skin: differential diagnosis of an umbilical erythematous plaque Keywords: Adenomatoid tumor, skin, umbilicus Short title: Adenomatoid tumor of the skin Authors: Ingrid Ferreira1, Olivier De Lathouwer2, Hugues Fierens3, Anne Theunis1, Josette André1, Nicolas de Saint Aubain3 1Dermatopathology laboratory, Department of Dermatology, Saint-Pierre University Hospital, Université Libre de Bruxelles, Brussels, Belgium. 2Department of Plastic surgery, Centre Hospitalier Interrégional Edith Cavell, Waterloo, Belgium. 3Department of Dermatology, Saint-Jean Hospital, Brussels, Belgium. 4Department of Pathology, Jules Bordet Institute, Université Libre de Bruxelles, Brussels, Belgium. Acknowledgements: None Corresponding author: Ingrid Ferreira This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/cup.13872 This article is protected by copyright. All rights reserved. Abstract Adenomatoid tumors are benign tumors of mesothelial origin that are usually encountered in the genital tract. Although they have been observed in other organs, the skin appears to be a very rare location with only one case reported in the literature to our knowledge. We report a second case of an adenomatoid tumor, arising in the umbilicus of a 44-year-old woman. The patient presented with an 8 months old erythematous and firm plaque under the umbilicus. A skin biopsy showed numerous microcystic spaces dissecting a fibrous stroma and being lined by flattened to cuboidal cells with focal intraluminal papillary formation. This poorly known diagnosis constitutes a diagnostic pitfall for dermatopathologists and dermatologists, and could be misdiagnosed as other benign or malignant entities. -
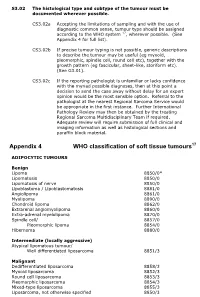
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

The Dermatopathology Milestone Project
The Dermatopathology Milestone Project A Joint Initiative of The Accreditation Council for Graduate Medical Education, The American Board of Dermatology, and The American Board of Pathology July 2015 The Dermatopathology Milestone Project The Milestones are designed only for use in evaluation of fellows in the context of their participation in ACGME- accredited residency or fellowship programs. The Milestones provide a framework for the assessment of the development of the fellow in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the six domains of physician competency, nor are they designed to be relevant in any other context. i Dermatopathology Milestones Chair: James W. Patterson, MD Working Group Advisory Group Laura Edgar, EdD, CAE C. Bruce Alexander, MD Tammie Ferringer, MD Julia C. Iezzoni, MD Jessica Kozel, MD Rebecca Johnson, MD Mary Stone, MD Wesley Y. Naritoku, MD, PhD Sharon Weiss, MD ii Milestone Reporting This document presents Milestones designed for programs to use in semi-annual review of fellow performance and reporting to the ACGME. Milestones are knowledge, skills, attitudes, and other attributes for each of the ACGME competencies organized in a developmental framework from less to more advanced. They are descriptors and targets for fellow performance as a fellow moves from entry into fellowship through graduation. In the initial years of implementation, the Review Committee will examine Milestone performance data for each program’s fellows as one element in the Next Accreditation System (NAS) to determine whether fellows overall are progressing. For each period, review and reporting will involve selecting milestone levels that best describe each fellow’s current performance and attributes. -

Dermatofibrosarcoma Protuberans in a Male Infant
Pediatric Case Reports Dermatofibrosarcoma Protuberans in a Male Infant Leslie Peard, Nicholas G. Cost, and Amanda F. Saltzman Dermtofibrosarcoma protuberans is a rare cutaneous malignancy known to be locally aggressive. It is uncommonly seen in the pediatric population and can be difficult to distinguish from other benign skin lesions. We present a case of dermatofi- brosarcoma protuberans of the penis in a 6-month-old child managed with surgical resection. This case highlights the challenges of diagnosis of genital lesions in children and the complexities of genitourinary reconstruction following surgical resection. UROLOGY 129: 206−209, 2019. © 2018 Elsevier Inc. ermatofibrosarcoma protuberans (DFSP) is a and no frozen section was sent intraoperatively. The rare cutaneous malignancy with reported foreskin was not sent to pathology per institutional D annual incidence of 4.2 per million (0.3 to practice. 1.3 per million in pediatric patients) in the United Pathologic evaluation by a dermatopathologist revealed States. Patients are typically 20-50 years old. DFSP a CD34+ spindle cell neoplasm, favoring DFSP, with most commonly occurs on the trunk, and is very rarely involvement of deep and “lateral” margins (again, the found on the genitalia.1 To our knowledge, only four specimen was not orientated). FISH for the chromosomal cases of penile DFSP have been reported.2-4 The tumor translocation t(17,22) was negative. CT chest obtained is locally aggressive, with few reported cases of metas- for staging was negative for metastasis. After discussion at tasis.1 There is a paucity of data concerning character- multidisciplinary tumor board, options for management istics of disease and treatment strategies with only 2 proposed included Mohs surgery under local anesthesia by published guidelines available to guide management.5,6 dermatology versus wide local excision with frozen section We present a case of DFSP of the penis in an infant, under general anesthesia by urology. -

Epssg NRSTS 2005
EpSSG NRSTS 2005 a protocol for Localized Non-Rhabdomyosarcoma Soft Tissue Sarcomas VERSION 1.1 SEPTEMBER 2009 EpSSG NRSTS 2005 protocol Version 1.1 Contents 1. Administrative organisation p. 3 1.1 Protocol sponsor p. 3 1.2 Protocol coordination p. 3 1.3 EpSSG and NRSTS 2005 structure p. 4 2. Abbreviations p.10 3. Summary p.11 3.1. Objectives p.12 3.2. Patients eligibility p.12 3.3. Patients stratification p.13 3.4. Pathology and Biology p.13 3.5. Statistical consideration p.13 3.6. Organisation of the study p.14 3.7. Datamanagement and analysis p.14 3.8. Ethical consideration p.14 4. Background p.16 4.1. References p.20 5. Study structure p.22 6. Patient eligibility p.22 7. Pre-treatment investigation p.23 7.1. Histological diagnosis p.23 7.2. Clinical assessment p.23 7.3. Laboratory investigations p.23 7.4. Radiological investigations p.24 7.5. Tumour measurements p.25 7.6. Lung lesions p.25 8. Staging system p.26 8.1. References p.26 9. Surgical guidelines p.27 9.1. Definitions p.27 9.2. Biopsy p.28 9.3. Primary resection p.29 9.4. Primary re-operation p.30 9.5. Secondary re-operation p.30 9.6. Reconstructive surgery and local control p.31 9.7. Lymph nodes p.31 9.8. Specific sites p.32 9.9. Surgery for relapse p.34 9.10. Marker clips p.34 9.11. Histology p.34 9.12. References p.34 10. -
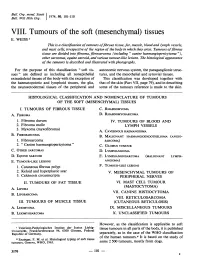
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

DERMATOPATHOLOGY Resident Training in Dermatopathology
1 DERMATOPATHOLOGY Resident training in dermatopathology includes a monthly glass slide conference at UMMC and a required one-month rotation at Dermatopathology Associates PLLC, both taught by Drs. Billy Walker and Jennifer Schulmeier, board-certified dermatopathologists. In addition, residents will sign out skin cases with the surgical pathology faculty when rotating on general surgical pathology at UMMC. Elective rotations at the senior level are also available with Drs. Walker and Schulmeier. Objectives for Six General Competencies Skill level 1 1. Patient Care A. Understand proper collection and processing of skin specimens. B. Be familiar with various methods of cutting skin specimens, with particular attention to surgical margins and how to best represent the gross lesion. C. Correlate clinical information with gross/microscopic findings. D. Know circumstances in which the clinician should be contacted for additional information. E. Know when and how to order special stains F. Familiarity with various fixatives G. Know the indications for, and be able to manage, frozen sections on skin specimens. 2. Medical Knowledge A. As part of the monthly unknown skin slide conference, read each chapter in Lever’s Histopathology of the Skin B. Thoroughly evaluate unknown glass slides prior to the monthly conference, to include differential diagnosis, clinical presentation, prognosis, and treatment. C. Recognize and diagnose common skin conditions on skin biopsies D. Recognize a biopsy as representing an uncommon skin condition which might merit subspecialty referral. Obtain consultation from Drs. Walker and Schulmeier E. Discuss the etiology, pathogenesis and treatment of common skin neoplasms, including melanoma, SCC of skin, basal cell carcinoma, etc. -

Adenomatoid Tumour of the Adrenal Gland: a Case Report and Literature Review
CORE Metadata, citation and similar papers at core.ac.uk Provided by Jagiellonian Univeristy Repository POL J PATHOL 2010; 2: 97–102 ADENOMATOID TUMOUR OF THE ADRENAL GLAND: A CASE REPORT AND LITERATURE REVIEW MAGDALENA BIAŁAS1, WOJCIECH SZCZEPAŃSKI1, JOANNA SZPOR1, KRZYSZTOF OKOŃ1, MARTA KOSTECKA-MATYJA2, ALICJA HUBALEWSKA-DYDEJCZYK2, ROMANA TOMASZEWSKA1 1Chair and Department of Pathomorphology, Jagiellonian University Medical College, Kraków 2Chair and Department of Endocrinology, Jagiellonian University Medical College, Kraków Adenomatoid tumour (AT) is a rare, benign neoplasm of mesothelial origin, which usually occurs in the genital tract of both sexes. Occasionally these tumours are found in extra genital locations such as heart, pancreas, skin, pleura, omentum, lymph nodes, retroperitoneum, intestinal mesentery and adrenal gland. Histologically ATs show a mixture of solid and cystic patterns usually with focal presence of signet-ring like cells and scattered lymphoid infiltration. The most important thing about these tumours is not to misdiagnose them as primary malignant or metastatic neoplasms. We present a case of an adrenal AT in a 29-year-old asymptomatic male. The tumour was an incidental finding during abdominal CT-scan for an unrelated condition. We also present a review of the literature concerning adrenal gland AT and give possible differential diagnosis. Key words: adenomatoid tumour, adrenal gland, immunophenotype. Introduction histopathological examination. Additional sections were made for immunohistochemical analysis (for Adenomatoid tumour (AT) is a benign neoplasm details see Table I). of mesothelial origin [1-3]. The usual place of its Proliferative activity of the tumour was deter- appearance is the male and female genital tract, most mined using immunohistochemical staining for often epididymis in men and fallopian tube in women nuclear protein MIB-1 (Ki-67).