Dermatopathology Laboratory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
July 2020 Goal the Goal of the Residency Program Is to Develop Future Leaders in Both Research and Clinical Medicine
Residency Training Program July 2020 Goal The goal of the Residency Program is to develop future leaders in both research and clinical medicine. Flexibility within the program allows for the acquisition of fundamental working knowledge in all subspecialties of dermatology. All residents are taught a scholarly approach to patient care, aimed at integrating clinicopathologic observation with an understanding of the basic pathophysiologic processes of normal and abnormal skin. Penn’s Residency Program consists of conferences, seminars, clinical rotations, research, and an opportunity to participate in the teaching of medical students. An extensive introduction into the department and the William D. James, M.D. Director of Residency Program clinic/patient care service is given to first-year residents. A distinguished clinical faculty and research faculty, coupled with the clinical and laboratory facilities, provides residents with comprehensive training. An appreciation of and participation in the investigative process is an integral part of our residency. Graduates frequently earn clinical or basic science fellowship appointments at universities across the country. Examples of these include: pediatric dermatology, dermatopathology, dermatologic surgery, dermatoepidemiology, postdoctoral and Clinical Educator fellowships. Additional post graduate training has occurred at the NIH and CDC. Graduates of our program populate the faculty at Harvard, Penn, Johns Hopkins, MD Anderson, Dartmouth, Penn State, Washington University, and the Universities of Washington, Pittsburgh, Vermont, South Carolina, Massachusetts, Wisconsin, and the University of California San Francisco. Additionally, some enter private practice to become pillars of community medicine. Misha A. Rosenbach, M.D. Associate Director of Residency Program History The first medical school in America, founded in 1765, was named the College of Philadelphia. -

Lessons from the African Teledermatology Project
Report The role of dermatopathology in conjunction with teledermatology in resource-limited settings: lessons from the African Teledermatology Project Matthew W. Tsang1, MD, MSt, and Carrie L. Kovarik2, MD 1Department of Dermatology, University Abstract of Minnesota, Minneapolis, MN, USA, Background Access to dermatology and dermatopathology services is scarce in 2 and, Departments of Dermatology and sub-Saharan Africa. Teledermatology provides consultations for healthcare providers in Internal Medicine, University of resource-limited settings where specialty medical services are difficult to obtain, and the Pennsylvania, Division of Infectious Diseases, Philadelphia, PA, USA African Teledermatology Project has helped to bridge the gap in dermatological care in Africa. This program also allows for biopsy specimens to be sent to the USA for processing Correspondence in cases where the clinical diagnosis is difficult and definitive diagnosis has implications for Carrie Kovarik, MD patient management. This study characterizes conditions diagnosed through clinicopatho- Assistant Professor logical correlation in conjunction with photos and tissue submitted to the African Dermatology, Dermatopathology, and Infectious Diseases Teledermatology Project. University of Pennsylvania Materials and methods Retrospective case review of tissue specimens submitted over 2 Maloney Building three years. 3600 Spruce Street Results Fifty-five biopsy specimens met inclusion criteria and represent cases of Philadelphia, PA 19104 malignancy (35%), infection (7%), suspected infection (15%), lichenoid tissue reaction E-mail: [email protected] (5%), dermatitis (15%), and other various conditions (18%). Three biopsy specimens were Funding sources: None. non-diagnostic (5%). Clinicopathological concordance between submitting clinician and Disclosures: The authors have no biopsy results occurred in 32 out of 55 cases (58%). -

Artificial Intelligence in Dermatopathology
Review Artificial Intelligence in Dermatopathology: New Insights and Perspectives Gerardo Cazzato 1,* , Anna Colagrande 1, Antonietta Cimmino 1, Francesca Arezzo 2, Vera Loizzi 2 , Concetta Caporusso 1, Marco Marangio 3, Caterina Foti 4, Paolo Romita 4, Lucia Lospalluti 4, Francesco Mazzotta 5, Sebastiano Cicco 6 , Gennaro Cormio 2 , Teresa Lettini 1 , Leonardo Resta 1 , Angelo Vacca 6 and Giuseppe Ingravallo 1,* 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (A.C.); [email protected] (A.C.); [email protected] (C.C.); [email protected] (T.L.); [email protected] (L.R.) 2 Section of Ginecology and Obstetrics, Department of Biomedical Sciences and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (F.A.); [email protected] (V.L.); [email protected] (G.C.) 3 Section of Informatics, University of Salento, 73100 Lecce, Italy; [email protected] 4 Section of Dermatology, Department of Biomedical Science and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (C.F.); [email protected] (P.R.); [email protected] (L.L.) 5 Pediatric Dermatology and Surgery Outpatients Department, Azienda Sanitaria Locale Barletta-Andria-Trani, 76123 Andria, Italy; [email protected] 6 Section of Internal Medicine, Department of Biomedical Sciences and Human Oncology, University of Bari Aldo Moro, 70124 Bari, Italy; [email protected] (S.C.); [email protected] (A.V.) * Correspondence: [email protected] (G.C.); [email protected] (G.I.) Citation: Cazzato, G.; Colagrande, A.; Abstract: In recent years, an increasing enthusiasm has been observed towards artificial intelligence Cimmino, A.; Arezzo, F.; Loizzi, V.; and machine learning, involving different areas of medicine. -

The Dermatopathology Milestone Project
The Dermatopathology Milestone Project A Joint Initiative of The Accreditation Council for Graduate Medical Education, The American Board of Dermatology, and The American Board of Pathology July 2015 The Dermatopathology Milestone Project The Milestones are designed only for use in evaluation of fellows in the context of their participation in ACGME- accredited residency or fellowship programs. The Milestones provide a framework for the assessment of the development of the fellow in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the six domains of physician competency, nor are they designed to be relevant in any other context. i Dermatopathology Milestones Chair: James W. Patterson, MD Working Group Advisory Group Laura Edgar, EdD, CAE C. Bruce Alexander, MD Tammie Ferringer, MD Julia C. Iezzoni, MD Jessica Kozel, MD Rebecca Johnson, MD Mary Stone, MD Wesley Y. Naritoku, MD, PhD Sharon Weiss, MD ii Milestone Reporting This document presents Milestones designed for programs to use in semi-annual review of fellow performance and reporting to the ACGME. Milestones are knowledge, skills, attitudes, and other attributes for each of the ACGME competencies organized in a developmental framework from less to more advanced. They are descriptors and targets for fellow performance as a fellow moves from entry into fellowship through graduation. In the initial years of implementation, the Review Committee will examine Milestone performance data for each program’s fellows as one element in the Next Accreditation System (NAS) to determine whether fellows overall are progressing. For each period, review and reporting will involve selecting milestone levels that best describe each fellow’s current performance and attributes. -

General Dermatology Practice Brochure
Appointments Our Providers David A. Cowan, MD, FAAD We are currently accepting • Fellow, American Academy of Dermatology new patients. • Associate, American College of Call today to schedule your appointment Mohs Micrographic Surgery Monday - Friday, 8:00am to 4:30pm Rebecca G. Pomerantz, MD 1-877-661-3376 • Board Certified, American Academy of Cancellations & “No Show” Policy Dermatology If you are unable to keep your scheduled Lisa L. Ellis, MPAS, PA-C appointment, please call the office and we will • Member, American Academy of Physician be more than happy to reschedule for you. Assistants Failure to notify us at least 48 hours prior to your • Member, PA Society of Physician Assistants Medical and appointment may result in a cancellation fee. • Member, Society of Dermatology Physician Prescription Refills Assistants Surgical Refill requests are handled during normal office Sheri L. Rolewski, MSN, CRNP-BC hours when our staff has full access to medical • National Board Certification, Family Nurse Dermatology records. Refills cannot be called in on holidays, Practitioner Specialty weekends or more than twelve months after your • Member, Dermatology Nurse Association last exam. Please have your pharmacy contact our office directly. Test Results SMy Dermatology Appointment You will be notified when we receive your Date/Day _____________________________________ pathology or other test results, usually within two weeks from the date of your procedure. If you Time _________________________________________ do not hear from us within three -

Dermatology at the Berkeley Outpatient Center
Dermatology Berkeley Outpatient Center Overview Encompassing both medical and cosmetic dermatology, our experts at the Berkeley Outpatient Center offer a full range of diagnostic, treatment and surgical services for patients with cutaneous conditions. Surgical Dermatology • Fellowship-trained expertise in • Close coordination with Plastic Surgery Mohs micrographic surgery for at the Berkeley Outpatient Center, treatment of skin cancers including allowing for streamlined treatment for basal cell carcinomas and squamous related procedures in one location cell carcinomas, as well as treatment of • Outpatient surgery for removal of melanoma in situ with MART-1 staining benign skin growths and skin cancers Medical Dermatology - Conditions Treated/Services Offered • Acne, rosacea and related conditions • Mole/Atypical nevus/Melanoma • Sun-damaged skin surveillance • Aesthetic/Cosmetic dermatology • Non-melanoma skin cancers • Eczema and atopic dermatitis • Pigmentation disorders • HIV/AIDS-related skin conditions • Psoriasis • Lumps under the skin • Rashes • Infections of the skin (bacterial, viral, • Skin checks for patients with fungal and other) concerning lesions • Melanoma • Warts When to see a Dermatologist For more information, please call Dermatology Services at (510) 985-5200. Dermatology Services Providing integrated care in the community. Our Dermatology Team Erin Amerson, MD Drew Saylor, MD, MPH UCSF Health UCSF Health Dermatologist Dermatologic surgeon To learn more about our doctors, visit ucsfhealth.org/find_a_doctor. Office location: Berkeley Outpatient Center 3100 San Pablo Avenue Berkeley, CA 94702 (510) 985-5200 To learn more about our Berkeley Outpatient Center, Adeline St visit johnmuirhealth.com/ September 2020 berkeleyopc.. -
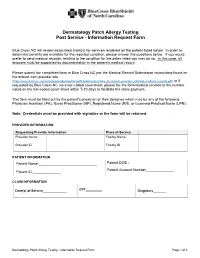
Dermatology Patch Allergy Testing Post Service - Information Request Form
Dermatology Patch Allergy Testing Post Service - Information Request Form Blue Cross NC will review associated claim(s) for services rendered on the patient listed below. In order to determine benefits are available for the reported condition, please answer the questions below. If you would prefer to send medical records, relating to the condition for the dates listed you may do so. In this case, all answers must be supported by documentation in the patient's medical record. Please submit the completed form to Blue Cross NC per the Medical Record Submission instructions found on the bcbsnc.com provider site (https://www.bcbsnc.com/assets/providers/public/pdfs/submissions/how_to_submit_provider_initiated_medical_records.pdf) or if requested by Blue Cross NC via a bar-coded coversheet, please fax the form/medical records to the number noted on the bar-coded cover sheet within 7-10 days to facilitate the claim payment. This form must be filled out by the patient's physician or their designee which may be any of the following: Physician Assistant (PA), Nurse Practitioner (NP), Registered Nurse (RN), or Licensed Practical Nurse (LPN). Note: Credentials must be provided with signature or the form will be returned. PROVIDER INFORMATION Requesting Provider Information Place of Service Provider Name Facility Name Provider ID Facility ID PATIENT INFORMATION Patient Name:_____________________________ Patient DOB :_____________ Patient Account Number______________ Patient ID:______________ CLAIM INFORMATION Date(s) of Service_____________ CPT_________ Diagnosis_______ Dermatology Patch Allergy Testing - Information Request Form Page 1 of 3 CLINICAL INFORMATION Did the patient have direct skin testing (for immediate hypersensitivity) by: Percutaneous or epicutaneous (scratch, prick, or puncture)? ________________ Intradermal testing? ___________________________________ Inhalant allergy evaluation? _________________ Did the patient have patch (application) testing (most commonly used: T.R.U.E. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. -

DERMATOPATHOLOGY Resident Training in Dermatopathology
1 DERMATOPATHOLOGY Resident training in dermatopathology includes a monthly glass slide conference at UMMC and a required one-month rotation at Dermatopathology Associates PLLC, both taught by Drs. Billy Walker and Jennifer Schulmeier, board-certified dermatopathologists. In addition, residents will sign out skin cases with the surgical pathology faculty when rotating on general surgical pathology at UMMC. Elective rotations at the senior level are also available with Drs. Walker and Schulmeier. Objectives for Six General Competencies Skill level 1 1. Patient Care A. Understand proper collection and processing of skin specimens. B. Be familiar with various methods of cutting skin specimens, with particular attention to surgical margins and how to best represent the gross lesion. C. Correlate clinical information with gross/microscopic findings. D. Know circumstances in which the clinician should be contacted for additional information. E. Know when and how to order special stains F. Familiarity with various fixatives G. Know the indications for, and be able to manage, frozen sections on skin specimens. 2. Medical Knowledge A. As part of the monthly unknown skin slide conference, read each chapter in Lever’s Histopathology of the Skin B. Thoroughly evaluate unknown glass slides prior to the monthly conference, to include differential diagnosis, clinical presentation, prognosis, and treatment. C. Recognize and diagnose common skin conditions on skin biopsies D. Recognize a biopsy as representing an uncommon skin condition which might merit subspecialty referral. Obtain consultation from Drs. Walker and Schulmeier E. Discuss the etiology, pathogenesis and treatment of common skin neoplasms, including melanoma, SCC of skin, basal cell carcinoma, etc. -
Concepts of Sliding and Lifting Tissue Movement in Flap Reconstruction
HOW I DO IT/BACK TO BASICS This new feature will emphasize innovative and better ways to perform dermatologic surgery procedures. This ar- ticle should be based on some evidence-based literature, but may describe the author’s experience with a particular procedure without being a typical clinical research article. The Editor will consider ideas for topics. Any author who is considering writing an article should submit the title to Ronald L. Moy, MD, Editor-in-Chief, 100 UCLA Medical Plaza, Suite 590, Los Angeles, CA 90024. Concepts of Sliding and Lifting Tissue Movement in Flap Reconstruction Timothy M. Johnson, MD,*†‡ Neil Swanson, MD,§ and Shan R. Baker, MD† Departments of *Dermatology, †Otorhinolaryngology, and ‡Surgery, University of Michigan Medical Center, Ann Arbor, Michigan, and §Department of Dermatology and Otolaryngology, Oregon Health Sciences, Portland Oregon background. The optimal design of a skin flap requires an the answer to three predictable events that result from tissue understanding of the concepts of tissue movement. transfer: Where is the tension? Where are the final incision objective. The purpose of this manuscript was to demon- lines? Where is the redundant tissue? strate concepts of sliding and lifting tissue movement for flap conclusion. A mental exercise assessing all available recon- reconstruction. struction options should be performed for each individual pa- methods. Six similar defects located in the forehead–temple– tient and defect. Both patient and defect considerations need to eyebrow region were repaired using a different skin flap. be assessed. A thorough understanding of both anatomy and tis- results. The specific flap design for a given defect is based on sue movement is necessary for optimal skin flap reconstruction. -

Surgical Treatment Options for Lower Eyelid Aging Joe Niamtu III, DMD
COSMETIC TECHNIQUE Surgical Treatment Options for Lower Eyelid Aging Joe Niamtu III, DMD The lower eyelid and associated anatomy represent a complex structure that is key in facial aging and rejuvenation. There are numerous ways to address this region and some of the more common treat- ment options are discussed in this article. A review is presented of the diagnosis and popular treatment options to address the most common aspects of eyelid aging. The author has performed cosmetic lower eyelid surgery using transconjunctival blepharoplasty with skin resurfacing for the past 12 years, with pleasing results and low complications. Lower eyelid rejuvenation is one of the most commonly requested procedures in a cosmetic surgery practice. A firm understanding of the complex anatomy of this region is paramount to successful treatment. Although many methods exist for addressing this region, some techniques are more prone to postoperative complications. The author has had continued success with hundreds of patients by performing transconjunctival lower eyelid blepharoplasty with CO2 laser resurfacing, chemicalCOS peels, or skin-pinch DERM procedures. These procedures are safe, predictable, and have a place in theDo armamentarium Not of contemporary Copy cosmetic surgeons. ermatochalasis is the crepey, wrinkled, The basis of this article concerns skin aging and its loose, and sun damaged skin of the eye- surgical correction, but discussion of the periorbital fat is lids. Because age-associated changes to germane to the understanding of the aging process and its the upper face often present earlier than correction. The periorbital fat is an essential evolutionary age-associated changes to the lower face, system that serves in part to cushion the globe within its itD is not uncommon for the cosmetic surgery practitioner bony orbit.