NYS Cancer Registry Facility Reporting Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rare Skin Cancers in General Practice
CLINICAL PRACTICE Skin cancer Rare skin cancers in series general practice Case study Anthony Dixon Mr LA has long been troubled with actinic damage to his skin, especially his face. He has had MBBS, FACRRM, is many squamous cell carcinomas (SCCs) removed and many solar keratoses managed. dermasurgeon and Director On this occasion Mr LA had two actinic lesions on his left cheek that failed to respond to of Research, Skin Alert cryotherapy (Figure 1). A biopsy of each site produced a surprise. Histology of the superior Skin Cancer Clinics and lesion revealed sebaceous carcinoma (Figure 2). This is an uncommon yet aggressive cutaneous Skincanceronly, Belmont, malignancy derived from sebaceous glands. The 5 year survival rate is 60–70%. Victoria. anthony@ The tumour was widely excised with a minimum 10 mm margin. A multidisciplinary approach skincanceronly.com resulted in a decision not to proceed to adjunctive radiotherapy. The wound was well healed by 8 weeks (Figure 3). Four years on there is no sign of local or regional recurrence (Figure 4). Many sebaceous carcinomas occur on the eyelids where the outcome is often poor;1 and some patients are prone to multiple other cutaneous SCCs. There is also a rare syndrome called Muir-torre of visceral neoplasms associated with sebaceous carcinoma on the skin.2 As this is an autosomal dominant condition, family history and counselling is an esssential part of management (enquire about family history of internal malignancies). A family member's diagnosis can be Figure 3. Satisfactory healing 8 weeks Figure 1. Two actinic lesions on the left face following wide excision of sebaceous important for other family members and offers screening have failed to respond to cryotherapy carcinoma for internal and cutaneous malignancies. -

Central Nervous System Cancers Panel Members Can Be Found on Page 1151
1114 NCCN David Tran, MD, PhD; Nam Tran, MD, PhD; Frank D. Vrionis, MD, MPH, PhD; Patrick Y. Wen, MD; Central Nervous Nicole McMillian, MS; and Maria Ho, PhD System Cancers Overview In 2013, an estimated 23,130 people in the United Clinical Practice Guidelines in Oncology States will be diagnosed with primary malignant brain Louis Burt Nabors, MD; Mario Ammirati, MD, MBA; and other central nervous system (CNS) neoplasms.1 Philip J. Bierman, MD; Henry Brem, MD; Nicholas Butowski, MD; These tumors will be responsible for approximately Marc C. Chamberlain, MD; Lisa M. DeAngelis, MD; 14,080 deaths. The incidence of primary brain tumors Robert A. Fenstermaker, MD; Allan Friedman, MD; Mark R. Gilbert, MD; Deneen Hesser, MSHSA, RN, OCN; has been increasing over the past 30 years, especially in Matthias Holdhoff, MD, PhD; Larry Junck, MD; elderly persons.2 Metastatic disease to the CNS occurs Ronald Lawson, MD; Jay S. Loeffler, MD; Moshe H. Maor, MD; much more frequently, with an estimated incidence ap- Paul L. Moots, MD; Tara Morrison, MD; proximately 10 times that of primary brain tumors. An Maciej M. Mrugala, MD, PhD, MPH; Herbert B. Newton, MD; Jana Portnow, MD; Jeffrey J. Raizer, MD; Lawrence Recht, MD; estimated 20% to 40% of patients with systemic cancer Dennis C. Shrieve, MD, PhD; Allen K. Sills Jr, MD; will develop brain metastases.3 Abstract Please Note Primary and metastatic tumors of the central nervous system are The NCCN Clinical Practice Guidelines in Oncology a heterogeneous group of neoplasms with varied outcomes and (NCCN Guidelines®) are a statement of consensus of the management strategies. -

Atypical Compound Nevus Arising in Mature Cystic Ovarian Teratoma
J Cutan Pathol 2005: 32: 71–123 Copyright # Blackwell Munksgaard 2005 Blackwell Munksgaard. Printed in Denmark Journal of Cutaneous Pathology Abstracts of the Papers Presented at the 41st Annual Meeting of The American Society of Dermatopathology Westin Copley Place Boston, Massachusetts, USA October 14–17, 2004 These abstracts were presented in oral or poster format at the 41st Annual Meeting of The American Society of Dermatopathology on October 14–17, 2004. They are listed on the following pages in alphabetical order by the first author’s last name. 71 Abstracts IN SITU HYBRIDIZATION IS A VALUABLE DIAGNOSTIC A 37-year-old woman with diagnosis of Sjogren’s syndrome (SS) TOOL IN CUTANEOUS DEEP FUNGAL INFECTIONS presented with asymptomatic non-palpable purpura of the lower J.J. Abbott1, K.L. Hamacher2,A.G.Bridges2 and I. Ahmed1,2 extremities. Biopsy of a purpuric macule revealed a perivascular Departments of Laboratory Medicine and Pathology1 and and focally nodular lymphocytic infiltrate with large numbers of Dermatology2, plasma cells, seemingly around eccrine glands. There was no vascu- litis. The histologic findings in the skin were strikingly similar to those Mayo Clinic and Mayo Foundation, Rochester, MN, USA of salivary, parotid, and other ‘‘secretory’’ glands affected in SS. The cutaneous manifestations of SS highlighted in textbooks include Dimorphic fungal infections (histoplasmosis, blastomycosis, coccidiomy- xerosis, annular erythema, small-vessel vasculitis, and pigmented cosis, and cryptococcosis) can occur in immunocompromised and purpura. This case illustrates that purpura in skin of patients with healthy individuals. Cutaneous involvement is often secondary and SS may be caused by a peri-eccrine plasma-rich infiltrate. -

Malignant Glioma Arising at the Site of an Excised Cerebellar Hemangioblastoma After Irradiation in a Von Hippel-Lindau Disease Patient
DOI 10.3349/ymj.2009.50.4.576 Case Report pISSN: 0513-5796, eISSN: 1976-2437 Yonsei Med J 50(4): 576-581, 2009 Malignant Glioma Arising at the Site of an Excised Cerebellar Hemangioblastoma after Irradiation in a von Hippel-Lindau Disease Patient Na-Hye Myong1 and Bong-Jin Park2 1Department of Pathology, Dankook University College of Medicine, Cheonan; 2Department of Neurosurgery, Kyunghee University Hospital, Seoul, Korea. We describe herein a malignant glioma arising at the site of the resected hemangioblastoma after irradiation in a patient with von Hippel-Lindau disease (VHL). The patient was a 25 year-old male with multiple heman- gioblastomas at the cerebellum and spinal cord, multiple pancreatic cysts and a renal cell carcinoma; he was diagnosed as having VHL disease. The largest hemangioblastoma at the right cerebellar hemisphere was completely removed, and he received high-dose irradiation postoperatively. The tumor recurred at the same site 7 years later, which was a malignant glioma with no evidence of hemangioblastoma. The malignant glioma showed molecular genetic profiles of radiation-induced tumors because of its diffuse p53 immunostaining and the loss of p16 immunoreactivity. The genetic study to find the loss of heterozygosity (LOH) of VHL gene revealed that only the cerebellar hemangioblastoma showed allelic losses for the gene. To the best of our knowledge, this report is the first to show a malignant glioma that developed in a patient with VHL disease after radiation therapy at the site of an excised hemangioblastoma. This report also suggests that radiation therapy should be performed very carefully in VHL patients with hemangioblastomas. -

Mixed Hepatoblastoma in the Adult: Case Report and Review of the Literature
J Clin Pathol: first published as 10.1136/jcp.33.11.1058 on 1 November 1980. Downloaded from J Clin Pathol 1980;33:1058-1063 Mixed hepatoblastoma in the adult: case report and review of the literature RP HONAN AND MT HAQQANI From the Department of Pathology, Walton Hospital, Rice Lane, Liverpool L9 JAE, UK SUMMARY A case of mixed hepatoblastoma in a woman is described. A survey of the English literature reveals 13 cases acceptable as mixed hepatoblastoma; these have been described and published under a variety of names. Difficulties in nomenclature and the histology of these cases are discussed. Diagnosis depends on the identification of both malignant mesenchymal and malignant epithelial elements. The former include myxoid connective tissue resembling primitive mesenchyme and areas resembling adult fibrosarcoma. Mature fibrous tissue with calcification and bone for- mation may be seen. Epithelial areas show tissue resembling fetal liver, poorly differentiated epithelial cells, and/or areas of adenocarcinoma. The current view on histogenesis is also given. Most hepatoblastomas occur in children under the mixedtumour,6carcino-osteochondromyxosarcoma,5 copyright. age of 2 years.' Hepatoblastoma in adults is ex- and rhabdomyosarcohepatoma.7 tremely rare, and the prognosis is much worse than in the mixed hepatoblastoma of childhood. Case report The literature of mixed hepatoblastoma in adults has until recently been confused, and the true inci- CLINICAL PRESENTATION dence of the tumour obscured, owing to the various A Chinese woman aged 27 had been resident in names used by different authors to describe their England for eight years. She gave a history of cases. The commonest pseudonym is 'mixed malig- 18 months' intermittent right-sided chest pain http://jcp.bmj.com/ nant tumour',2-4 an ambivalent term which merely and upper abdominal discomfort. -

Combined Goblet Cellcarcinoid and Mucinous Cystadenoma of The
I Clin Pathol 1995;48:869-870 869 Combined goblet cell carcinoid and mucinous cystadenoma of the appendix J Clin Pathol: first published as 10.1136/jcp.48.9.869 on 1 September 1995. Downloaded from R K Al-Talib, C H Mason, J M Theaker Abstract Case reports Two cases of combined goblet cell car- CASE ONE cinoid and mucinous cystadenoma oc- An adherent pelvic appendix was resected with curring in the appendix are reported. The difficulty from a 54 year old woman admitted histogenesis of the goblet cell carcinoid for an interval appendicectomy, two months remains one of its most controversial as- after an attack of appendicitis. The appendix pects and the occurrence of both of these measured 60 x 15 mm and was irregular, dis- relatively uncommon tumours in the same torted and showed serosal fibrosis. On sec- organ may lend support to the unitary tioning, the tip of the appendix was distended stem cell hypothesis on the origin of this and a mucus containing diverticulum pen- tumour. Alternatively, this occurrence etrating the muscular wall of the appendix was may represent an example ofthe adenoma/ identified. carcinoma sequence. ( Clin Pathol 1995;48:869-870) Department of CASE TWO Histopathology, Keywords: Goblet cell carcinoid, mucinous cyst- A 64 year old woman was a Southampton adenoma, appendix, histogenesis. admitted with four University Hospitals month history of a dull ache in the right iliac NHS Trust, fossa which had become increasingly severe Southampton S09 4XY R K Al-Talib Goblet cell carcinoid is an uncommon tumour over the last week. -
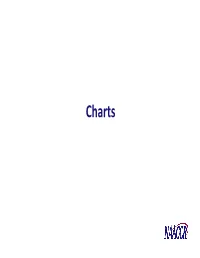
Charts Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart
Charts Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart Glial Tumor Neuronal and Neuronal‐ Ependymomas glial Neoplasms Subependymoma Subependymal Giant (9383/1) Cell Astrocytoma(9384/1) Myyppxopapillar y Desmoplastic Infantile Ependymoma Astrocytoma (9412/1) (9394/1) Chart 1: Benign and Borderline Intracranial and CNS Tumors Chart Glial Tumor Neuronal and Neuronal‐ Ependymomas glial Neoplasms Subependymoma Subependymal Giant (9383/1) Cell Astrocytoma(9384/1) Myyppxopapillar y Desmoplastic Infantile Ependymoma Astrocytoma (9412/1) (9394/1) Use this chart to code histology. The tree is arranged Chart Instructions: Neuroepithelial in descending order. Each branch is a histology group, starting at the top (9503) with the least specific terms and descending into more specific terms. Ependymal Embryonal Pineal Choro id plexus Neuronal and mixed Neuroblastic Glial Oligodendroglial tumors tumors tumors tumors neuronal-glial tumors tumors tumors tumors Pineoblastoma Ependymoma, Choroid plexus Olfactory neuroblastoma Oligodendroglioma NOS (9391) (9362) carcinoma Ganglioglioma, anaplastic (9522) NOS (9450) Oligodendroglioma (9390) (9505 Olfactory neurocytoma Ganglioglioma, malignant (()9521) anaplastic (()9451) Anasplastic ependymoma (9505) Olfactory neuroepithlioma Oligodendroblastoma (9392) (9523) (9460) Papillary ependymoma (9393) Glioma, NOS (9380) Supratentorial primitive Atypical EdEpendymo bltblastoma MdllMedulloep ithliithelioma Medulloblastoma neuroectodermal tumor tetratoid/rhabdoid (9392) (9501) (9470) (PNET) (9473) tumor -

Central Nervous System Tumors General ~1% of Tumors in Adults, but ~25% of Malignancies in Children (Only 2Nd to Leukemia)
Last updated: 3/4/2021 Prepared by Kurt Schaberg Central Nervous System Tumors General ~1% of tumors in adults, but ~25% of malignancies in children (only 2nd to leukemia). Significant increase in incidence in primary brain tumors in elderly. Metastases to the brain far outnumber primary CNS tumors→ multiple cerebral tumors. One can develop a very good DDX by just location, age, and imaging. Differential Diagnosis by clinical information: Location Pediatric/Young Adult Older Adult Cerebral/ Ganglioglioma, DNET, PXA, Glioblastoma Multiforme (GBM) Supratentorial Ependymoma, AT/RT Infiltrating Astrocytoma (grades II-III), CNS Embryonal Neoplasms Oligodendroglioma, Metastases, Lymphoma, Infection Cerebellar/ PA, Medulloblastoma, Ependymoma, Metastases, Hemangioblastoma, Infratentorial/ Choroid plexus papilloma, AT/RT Choroid plexus papilloma, Subependymoma Fourth ventricle Brainstem PA, DMG Astrocytoma, Glioblastoma, DMG, Metastases Spinal cord Ependymoma, PA, DMG, MPE, Drop Ependymoma, Astrocytoma, DMG, MPE (filum), (intramedullary) metastases Paraganglioma (filum), Spinal cord Meningioma, Schwannoma, Schwannoma, Meningioma, (extramedullary) Metastases, Melanocytoma/melanoma Melanocytoma/melanoma, MPNST Spinal cord Bone tumor, Meningioma, Abscess, Herniated disk, Lymphoma, Abscess, (extradural) Vascular malformation, Metastases, Extra-axial/Dural/ Leukemia/lymphoma, Ewing Sarcoma, Meningioma, SFT, Metastases, Lymphoma, Leptomeningeal Rhabdomyosarcoma, Disseminated medulloblastoma, DLGNT, Sellar/infundibular Pituitary adenoma, Pituitary adenoma, -

PROPOSED REGULATION of the STATE BOARD of HEALTH LCB File No. R057-16
PROPOSED REGULATION OF THE STATE BOARD OF HEALTH LCB File No. R057-16 Section 1. Chapter 457 of NAC is hereby amended by adding thereto the following provision: 1. The Division may impose an administrative penalty of $5,000 against any person or organization who is responsible for reporting information on cancer who violates the provisions of NRS 457. 230 and 457.250. 2. The Division shall give notice in the manner set forth in NAC 439.345 before imposing any administrative penalty 3. Any person or organization upon whom the Division imposes an administrative penalty pursuant to this section may appeal the action pursuant to the procedures set forth in NAC 439.300 to 439. 395, inclusive. Section 2. NAC 457.010 is here by amended to read as follows: As used in NAC 457.010 to 457.150, inclusive, unless the context otherwise requires: 1. “Cancer” has the meaning ascribed to it in NRS 457.020. 2. “Division” means the Division of Public and Behavioral Health of the Department of Health and Human Services. 3. “Health care facility” has the meaning ascribed to it in NRS 457.020. 4. “[Malignant neoplasm” means a virulent or potentially virulent tumor, regardless of the tissue of origin. [4] “Medical laboratory” has the meaning ascribed to it in NRS 652.060. 5. “Neoplasm” means a virulent or potentially virulent tumor, regardless of the tissue of origin. 6. “[Physician] Provider of health care” means a [physician] provider of health care licensed pursuant to chapter [630 or 633] 629.031 of NRS. 7. “Registry” means the office in which the Chief Medical Officer conducts the program for reporting information on cancer and maintains records containing that information. -

Life Expectancy and Incidence of Malignant Disease Iv
LIFE EXPECTANCY AND INCIDENCE OF MALIGNANT DISEASE IV. CARCINOMAOF THE GENITO-URINARYTRACT CLAUDE E. WELCH,' M.D., AND IRA T. NATHANSON,? MS., M.D. (Front the Collis P. Huntington Memorial Hospital of Harvard University, and the Pondville State Hospitul, Wre~ztham,Mass.) In previous communications the life expectancy of patients with cancer of the breast (I), oral cavity (2), and gastro-intestinal tract (3) has been discussed. In the present paper the life expectancy of patients with carci- noma of the genito-urinary tract will be considered. The discussion will include cancer of the vulva, vagina, cervix and fundus uteri, ovary, penis, testicle, prostate, bladder, and kidney. All cases of cancer of these organs admitted to the Collis P. Huntington Memorial and Pondville Hospitals in the years 1912-1933 have been reviewed personally. It must again be stressed that these hospitals are organized strictly for the care of cancer patients. All those with cancer that apply are admitted for treatment; many of them have only terminal care. Only those cases in which a definite history of the date of onset could not be determined or in which the diagnosis was uncertain have been omitted in the present study. In compiling statistics on age and sex incidence all cases entering the hospitals before Jan. 1, 1936, have been included. The method of calculation of the life expectancy curves was fully described in the first paper (1). No at- tempt to evaluate the number of five-year survivals has been made, since many of the patients did not receive their initial treatment in these hospitals. -

Germline Fumarate Hydratase Mutations in Patients with Ovarian Mucinous Cystadenoma
European Journal of Human Genetics (2006) 14, 880–883 & 2006 Nature Publishing Group All rights reserved 1018-4813/06 $30.00 www.nature.com/ejhg SHORT REPORT Germline fumarate hydratase mutations in patients with ovarian mucinous cystadenoma Sanna K Ylisaukko-oja1, Cezary Cybulski2, Rainer Lehtonen1, Maija Kiuru1, Joanna Matyjasik2, Anna Szyman˜ska2, Jolanta Szyman˜ska-Pasternak2, Lars Dyrskjot3, Ralf Butzow4, Torben F Orntoft3, Virpi Launonen1, Jan Lubin˜ski2 and Lauri A Aaltonen*,1 1Department of Medical Genetics, Biomedicum Helsinki, University of Helsinki, Helsinki, Finland; 2International Hereditary Cancer Center, Department of Genetics and Pathology, Pomeranian Medical University, Szczecin, Poland; 3Department of Clinical Biochemistry, Aarhus University Hospital, Skejby, Denmark; 4Pathology and Obstetrics and Gynecology, University of Helsinki, Helsinki, Finland Germline mutations in the fumarate hydratase (FH) gene were recently shown to predispose to the dominantly inherited syndrome, hereditary leiomyomatosis and renal cell cancer (HLRCC). HLRCC is characterized by benign leiomyomas of the skin and the uterus, renal cell carcinoma, and uterine leiomyosarcoma. The aim of this study was to identify new families with FH mutations, and to further examine the tumor spectrum associated with FH mutations. FH germline mutations were screened from 89 patients with RCC, skin leiomyomas or ovarian tumors. Subsequently, 13 ovarian and 48 bladder carcinomas were analyzed for somatic FH mutations. Two patients diagnosed with ovarian mucinous cystadenoma (two out of 33, 6%) were found to be FH germline mutation carriers. One of the changes was a novel mutation (Ala231Thr) and the other one (435insAAA) was previously described in FH deficiency families. These results suggest that benign ovarian tumors may be associated with HLRCC. -

Human Anatomy As Related to Tumor Formation Book Four
SEER Program Self Instructional Manual for Cancer Registrars Human Anatomy as Related to Tumor Formation Book Four Second Edition U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutesof Health SEER PROGRAM SELF-INSTRUCTIONAL MANUAL FOR CANCER REGISTRARS Book 4 - Human Anatomy as Related to Tumor Formation Second Edition Prepared by: SEER Program Cancer Statistics Branch National Cancer Institute Editor in Chief: Evelyn M. Shambaugh, M.A., CTR Cancer Statistics Branch National Cancer Institute Assisted by Self-Instructional Manual Committee: Dr. Robert F. Ryan, Emeritus Professor of Surgery Tulane University School of Medicine New Orleans, Louisiana Mildred A. Weiss Los Angeles, California Mary A. Kruse Bethesda, Maryland Jean Cicero, ART, CTR Health Data Systems Professional Services Riverdale, Maryland Pat Kenny Medical Illustrator for Division of Research Services National Institutes of Health CONTENTS BOOK 4: HUMAN ANATOMY AS RELATED TO TUMOR FORMATION Page Section A--Objectives and Content of Book 4 ............................... 1 Section B--Terms Used to Indicate Body Location and Position .................. 5 Section C--The Integumentary System ..................................... 19 Section D--The Lymphatic System ....................................... 51 Section E--The Cardiovascular System ..................................... 97 Section F--The Respiratory System ....................................... 129 Section G--The Digestive System ......................................... 163 Section