Unprotected Left Main Stenting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Service Setting Briefing Social Work in Medical Setting (MSS& MSP) Rundown
Service Setting Briefing Social Work in Medical Setting (MSS& MSP) Rundown 3:30-4:30 • Mutual Introduction • Brief Overview of Social Work Services in Hong Kong Medical Settings • Exercise 4:30-4:45 • Do’s and don’ts in medical settings 4:45-5:00 • Useful Resources • Related Training and Orientation • Mid-Placement Sharing Where are you posted? • Adolescent Medical Centre, QEH • Patient Resource • Ap Lei Chau Clinic Centre, QEH • CancerCare & Support, • MSSU (HA), KH (+HK QMH Eye Hospital) • Community & Patient • MSSU (Psy.), PYH Resource Department, • MSSU (Psy.), YFSPC PYH • Health Resource Centre, YCH Where are you posted? Implication? Clustering of HA Service Hong Kong West Cluster • Grantham Hospital • MacLehose Medical Rehabilitation Centre • Queen Mary Hospital • The Duchess of Kent Children's Hospital at Sandy Bay • Tsan Yuk Hospital • Tung Wah Group of Hospitals Fung Yiu King Hospital • Tung Wah Hospital • Why should I be bothered by things happening in HA? • I’m a social worker doing social work in a medical setting only HA Strategic Plan 2017-2022 • Provide patient-centred care: ensuring patients have timely access to high quality and responsive services which place patients firmly at the heart of their care 1. Improving Service Quality 2. Optimizing Demand Management Hospital/Clinic = Secondary Setting => Meaning to me?? Improving Service Quality • Promote day services to reduce reliance on inpatient care • Strengthening service coordination and collaboration through the development of cluster/network-based service • Enhancing community-based care • Promote partnership with patients by empowering patients for self-care, engaging patients in shared decision-making about their care… Optimizing Demand Management • Raise the capacity of priority services of HA, particularly for high demand services having regard to the projected demand arising from a growing and ageing population… • Share out the demand with community partners, such as through public-private partnerships C.R.1 24/8/2018 Pt’s e. -

Application to Become a Member of the Alliance for Healthy Cities Southern District, Hong Kong Special Administrative Region People’S Republic of China
Application to become a Member of The Alliance for Healthy Cities Southern District, Hong Kong Special Administrative Region People’s Republic of China The Healthy Cities initiatives employ the overall strategy of making use of “intersectoral action and community participation to integrate health protection and health promotion activities and transform health determinants for the better”1, health determinants referring to the different factors that determine the health status of people. The Southern District fully agrees with this approach and is committed to employing this strategy to improve the physical and social environments in a sustainable manner, and to fully utilize those community resources which encourage residents to support each other in improving their health and quality of life and in developing toward their full potential, so as to transform the Southern District into a healthy city. In view of the above, the Southern District would like to apply for membership of The Alliance for Healthy Cities. District Profile 2. There are a total of 18 districts in the Hong Kong Special Administrative Region (HKSAR) distributed in the New Territories, Kowloon and Hong Kong Island. Amongst the four districts situated on Hong Kong Island, the Southern District occupies the most space, with an area of around 4000 hectares which is nearly half of the Island’s area, and enjoys the lowest population density. 3. The Southern District is as varied and interesting as it is vast. It is home to the University of Hong Kong Faculty of Medicine, one of only two medical schools in Hong Kong, as well as Cyberport, Hong Kong’s IT flagship. -

Thank You to Our Referees from 2010
Thank you to our referees from 2010 Dr OA Ajani, Hamad Hospital, Doha, Qatar Dr MR Kirkpatrick, Ninewells Hospital, Dundee, UK Dr SG Allan, Palmerston North Hospital, New Zealand Professor EC Klawiter, Washington University, St Louis, USA Dr RJ Allcock, Queen Elizabeth Hospital, Gateshead, UK Dr KP Klugman, Rollins School of Public Health, Atlanta, USA Dr JM Armitage, Clinical Trial Service Unit, Oxford, UK Dr H Knoop, Nijmegen Medical Centre, Netherlands Dr WL Au, Tan Tock Seng Hospital, Singapore Dr YC Kon, Tan Tock Seng Hospital, Singapore Dr PP Aylin, Imperial College, London, UK Dr UV Kulkarni, Robert Gordon University, Aberdeen, UK Dr P Baker, University of Kent, Canterbury, UK Professor IH Kunkler, Western General Hospital, Edinburgh, UK Dr S Barker-Collo, The University of Auckland, New Zealand Dr LC Lack, Flinders University of South Australia, Australia Dr DE Bateman, Sunderland Royal Hospital, Tyne and Wear, UK Dr FA Lateef, Singapore General Hospital, Singapore Professor DN Bateman, Royal Infirmary of Edinburgh, UK Professor CJ Lawrence, London Dr AW Beasley, Wellington, New Zealand Professor JH Lazarus, University Hospital of Wales, Cardiff, UK Professor D Bell, Chelsea & Westminster Hospital, London Dr IM Lennox, Victoria Infirmary, Glasgow Dr AW Beveridge, Queen Margaret Hospital, Dunfermline, UK Dr PA Levack, Ninewells Hospital, Dundee, UK Dr S Bhandari, Hull Royal Infirmary, UK Professor BJ Lipworth, Ninewells Hospital, Dundee, UK DN Bhattacharyya, Victoria Hospital, Kirkcaldy, UK Dr LM Loh, Singapore General Hospital, -

A General Brief About the Hospital Authority
Mission Statement 4. In keeping with its role, the Mission of the Hospital Authority is: · to meet the different needs of patients for public hospital services, and to improve the hospital environment for the benefit of patients; · to serve the public with care, dedication and efficiency, and to encourage community participation in the system, resulting in better care and more direct accountability to the public; · to provide rewarding, fair and challenging employment to all its staff, in an environment conducive to attracting, motivating and retaining well-qualified staff; · to advise the Government of the needs of the community for public hospital services and of the resources required to meet these needs, in order to provide adequate, efficient, effective and value for money public hospital services of the highest standards recognised internationally within the resources obtainable; and · to collaborate with other agencies and bodies in the healthcare and related fields both locally and overseas to provide the greatest benefit to the local community. Corporate Vision and Strategies 5. To realise its mission, the Hospital Authority has developed the following Corporate Vision: “The Hospital Authority will collaborate with other healthcare providers and carers in the community to create a seamless healthcare environment which will maximise healthcare benefits and meet community expectations.” 6. The Authority achieves this corporate vision by formulating a set of strategic directions every year through an extensive annual planning process, taking into account the funding position, societal expectations, Government’s healthcare policy, and the challenges in the internal and external environment. The 2 corporate vision and mission are turned into operational targets to meet the community needs for healthcare services. -

Birth Record
eHR Sharable Data - Birth Record May 2018 © HKSAR Government eHR Sharable Data - Birth Record Form Category 1 Entity Name Entity ID Definition Data Type Data Type Validation Rule Repeated Code Table Remark Data requirement Data requirement Data requirement Example (Certified Example (Certified Example (Certified (code) (description) Data (Certified Level 1) (Certified Level 2) (Certified Level 3) Level 1) Level 2) Level 3) Birth Birth datetime 100310 The birth date or birth datetime of a patient TS Time stamp M M M 11/02/2012 20/12/2011 21:22 09/12/2001 23:59 Record Birth Birth Birth institution code 1003346 [eHR value] of the "Birth institution" code table, to define CE Coded Birth institution NA NA M PMH Record Institution the healthcare institution who reported the birth data to element the Immigration Department Birth Birth Birth institution description 1003107 [eHR description] of the "Birth institution" code table, it ST String Birth institution NA NA M Princess Margaret Record Institution should be the corresponding description of the selected Hospital [Birth institution code]. Birth institution description is to define the healthcare institution who reported the birth data to the Immigration Department. Birth Birth Birth institution local description 1003108 The local description of the healthcare institution who ST String M M M St. Paul Hospital St. Paul Hospital Princess Margaret Record Institution reported the birth data to the Immigration Department. Hospital Birth Birth Birth location code 1003102 [eHR value] of the "Birth location" code table, to define CE Coded Birth location NA NA O BBA Record Location the location where the patient was born element Birth Birth Birth location description 1003103 [eHR description] of the "Birth location" code table, it ST String Birth location NA NA M if [Birth location code] Born before arrival Record Location should be the corresponding description of the selected is given [Birth location code]. -

Prospective Assessment of the Hong Kong Hospital Authority Universal
Prospective assessment of the Hong Kong Hospital ORIGINAL ARTICLE Authority universal Down syndrome screening programme Daljit S Sahota 邵浩達 WC Leung 梁永昌 Objective To evaluate the performance of the locally developed universal WP Chan 陳運鵬 Down syndrome screening programme. William WK To 杜榮基 Elizabeth T Lau 劉嚴德光 Design Population-based cohort study in the period July 2010 to June 2011 inclusive. TY Leung 梁德楊 Setting Four Hong Kong Hospital Authority Departments of Obstetrics and Gynaecology and a central university-based laboratory for maternal serum processing and risk determination. Participants Women were offered either a first-trimester combined test (nuchal translucency, free beta human chorionic gonadotropin, and pregnancy-associated plasma protein-A) or nuchal- translucency-only test, or a second-trimester double test (alpha-fetoprotein and total human chorionic gonadotropin) for detection of Down syndrome according to their gestational age. Those with a trisomy 21 term risk of 1:250 or higher were offered a diagnostic test. Results A total of 16 205 pregnancies were screened of which 13 331 (82.3%) had a first-trimester combined test, 125 (0.8%) had a nuchal-translucency test only, and 2749 (17.0%) had a second- trimester double test. There were 38 pregnancies affected by Down syndrome. The first-trimester screening tests had a 91.2% (31/34) detection rate with a screen-positive rate of 5.1% (690/13 Key words 456). The second-trimester test had a 100% (4/4) detection rate Down syndrome; First trimester with a screen-positive rate of 6.3% (172/2749). There were screening; Second trimester screening; seven (0.9%) pregnancies that miscarried following an invasive Nuchal translucency; Quality control diagnostic test. -

Palliative Care Nursing Support in the Community
Palliative Care Nursing Support in the Community Ko Po Shan, Polly Nurse Consultant (Palliative Care), KEC Hong Kong Hospital Authority Strategic Service Framework Palliative Care (2017) (Hong Kong Hospital Authority) : All patients facing life-threatening and life-limiting conditions and their families/carers receive timely, coordinated and holistic palliative care to address their physical, psychosocial and spiritual needs, and are given the opportunities to participate in the planning of their care, so as to improve quality of life till the end of the patients’ life journey. 2 Strategic Service Framework for Adult Palliative Care 2017 Enhance Promote care Enhance Strengthen governance collaboration palliative care performance collaboration between in the monitoring of medical & palliative care ambulatory for oncology & non and continuous palliative care palliative care community quality specialist specialist settings to improvement through support shared care patients model 3 Service Model of Adult Palliative Care in HK Hospital Authority (HA) Cluster-based service with enhanced governance and collaboration between medical and oncology palliative care specialists Identification Coordinate Care in place of patients Advance palliative care with palliative with support care through care needs by from hospital to planning shared care parent teams community approach Palliative care as an integral part of the care continuum to support patients and their families/carers Underpinned by strengthened performance monitoring Strategic Direction -

Hospital Authority Special Visiting Arrangement in Hospitals/Units with Non-Acute Settings Under Emergency Response Level Notes to Visitors
Hospital Authority Special Visiting Arrangement in Hospitals/Units with Non-acute Settings under Emergency Response Level Notes to Visitors 1. Hospital Authority implemented special visiting arrangement in four phases on 21 April 2021, 29 May 2021, 25 June 2021 and 23 July 2021 respectively (as appended table). Cluster Hospitals/Units with non-acute settings Cheshire Home, Chung Hom Kok Ruttonjee Hospital Hong Kong East Mixed Infirmary and Convalescent Wards Cluster Tung Wah Eastern Hospital Wong Chuk Hang Hospital Grantham Hospital MacLehose Medical Rehabilitation Centre Hong Kong West The Duchess of Kent Children’s Hospital at Sandy Bay Cluster Tung Wah Group of Hospitals Fung Yiu King Hospital Tung Wah Hospital Kowloon East Haven of Hope Hospital Cluster Hong Kong Buddhist Hospital Kowloon Central Kowloon Hospital (Except Psychiatric Wards) Cluster Our Lady of Maryknoll Hospital Tung Wah Group of Hospitals Wong Tai Sin Hospital Caritas Medical Centre Developmental Disabilities Unit, Wai Yee Block Medical and Geriatrics/Orthopaedics Rehabilitation Wards and Palliative Care Ward, Wai Ming Block North Lantau Hospital Kowloon West Extended Care Wards Cluster Princess Margaret Hospital Lai King Building Yan Chai Hospital Orthopaedics and Traumatology Rehabilitation Ward and Medical Extended Care Unit (Rehabilitation and Infirmary Wards), Multi-services Complex New Territories Bradbury Hospice East Cluster Cheshire Home, Shatin North District Hospital 4B Convalescent Rehabilitation Ward Shatin Hospital (Except Psychiatric Wards) Tai Po Hospital (Except Psychiatric Wards) Pok Oi Hospital Tin Ka Ping Infirmary New Territories Siu Lam Hospital West Cluster Tuen Mun Hospital Rehabilitation Block (Except Day Wards) H1 Palliative Ward 2. Hospital staff will contact patients’ family members for explanation of special visiting arrangement and scheduling the visits. -
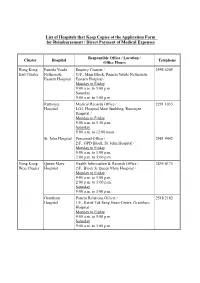
List of Hospitals That Keep Copies of the Application Form for Reimbursement / Direct Payment of Medical Expenses
List of Hospitals that Keep Copies of the Application Form for Reimbursement / Direct Payment of Medical Expenses Responsible Office / Location / Cluster Hospital Telephone Office Hours Hong Kong Pamela Youde Enquiry Counter / 2595 6205 East Cluster Nethersole G/F., Main Block, Pamela Youde Nethersole Eastern Hospital Eastern Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Ruttonjee Medical Records Office / 2291 1035 Hospital LG1, Hospital Main Building, Ruttonjee Hospital / Monday to Friday 9:00 a.m. to 5:30 p.m. Saturday 9:00 a.m. to 12:00 noon St. John Hospital Personnel Office / 2981 9442 2/F., OPD Block, St. John Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Hong Kong Queen Mary Health Information & Records Office / 2855 4175 West Cluster Hospital 2/F., Block S, Queen Mary Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Grantham Patient Relations Officer / 2518 2182 Hospital 1/F., Kwok Tak Seng Heart Centre, Grantham Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. - 2 - Responsible Office / Location / Cluster Hospital Telephone Office Hours Kowloon Kwong Wah Medical Report Office / 3517 5216 West Cluster Hospital 1/F., Central Stack, Kwong Wah Hospital / Monday to Friday 9:00 a.m. -

Hospital Authority List of Medical Social Services Units (January 2019)
Hospital Authority List of Medical Social Services Units (January 2019) Name of Hospital Address Tel No. Fax No. 1. Alice Ho Miu Ling Nethersole 11 Chuen On Road, Tai Po, N.T. 2689 2020 2662 3152 Hospital (Non- psychiatric medical social service) 2. Bradbury Hospital 17 A Kung Kok Shan Road, 2645 8832 2762 1518 Shatin, N.T. 3. Caritas Medical Centre 111 Wing Hong Street, 3408 7709 2785 3192 Shamshuipo, Kowloon 4. Cheshire Home 128 Chung Hom Kok Road, 2899 1391 2813 8752 (Chung Hom Kok) Hong Kong 5. Cheshire Home (Shatin) 30 A Kung Kok Shan Road, 2636 7269 2636 7242 Shatin, N.T. 6. TWGHs Fung Yiu King Hospital 9 Sandy Bay Road, Hong Kong 2855 6236 2904 9021 7. Grantham Hospital 125 Wong Chuk Hang Road, 2518 2678 2580 7629 Aberdeen, Hong Kong 8. Haven of Hope Hospital 8 Haven of Hope Road, 2703 8227 2703 8230 Tseung Kwan O, Kowloon 9. Hong Kong Buddhist Hospital 10 Heng Lam Road, Lok Fu, 2339 6253 2339 6298 Kowloon 10. Kowloon Hospital Mezzanine Floor, Kowloon 3129 7806/ 3129 7838 (Ward 2B at Rehabilitation Hospital Rehabilitation Building, 3129 7831 Building ) 147A, Argyle Street, Kowloon 11. Kwong Wah Hospital 25 Waterloo Road, Kowloon 3517 2900 3517 2959 12. MacLehose Medical 7 Sha Wan Drive, 2872 7131 2872 7909 Rehabilitation Centre Pokfulam, Hong Kong Name of Hospital Address Tel No. Fax No. 13. Our Lady of Maryknoll Hospital 118 Shatin Pass Road, 2354 2285 2324 8719 Wong Tai Sin, Kowloon 14. Pok Oi Hospital Au Tau, Yuen Long, N.T. 2486 8140 2486 8095 2486 8141 15. -

Reimbursement Forms in Designated Site
List of Hospitals that Keep Copies of Application FORM A and Application FORM B Responsible Office / Location / Cluster Hospital Telephone Office Hours Hong Kong Pamela Youde Enquiry Counter / 2595 6205 East Cluster Nethersole G/F., Main Block, Pamela Youde Nethersole Eastern Hospital Eastern Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Ruttonjee Medical Records Office / 2291 1035 Hospital LG1, Hospital Main Building, Ruttonjee Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:30 p.m. Saturday 9:00 a.m. to 12:00 noon St. John Hospital Personnel Office / 2981 9442 2/F., Out-Patients Block, St. John Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Hong Kong Queen Mary Health Information & Records Office / 2855 4175 West Cluster Hospital 2/F., Block S, Queen Mary Hospital / Monday to Friday 9:00 a.m. to 1:00 p.m. 2:00 p.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. Grantham Medical Records Office / 2518 2201 Hospital G/F., Main Block, Grantham Hospital / Monday to Friday 9:00 a.m. to 5:00 p.m. Saturday 9:00 a.m. to 1:00 p.m. - 2 - Responsible Office / Location / Cluster Hospital Telephone Office Hours Kowloon Kwong Wah Medical Report Office / 3517 5216 West Cluster Hospital 3B, Administration Building, Kwong Wah Hospital / Monday to Friday 8:45 a.m. -

List of Medical Social Services Units Under Social Welfare Department
List of Medical Social Services Units Under Social Welfare Department Hong Kong Name of Hospital/Clinic Tel. No. Email Address 1. Queen Mary Hospital 2255 3762 [email protected] 2255 3764 2. Wong Chuk Hang Hospital 2873 7201 [email protected] 3. Pamela Youde Nethersole Eastern 2595 6262 [email protected] Hospital 4. Pamela Youde Nethersole Eastern 2595 6773 [email protected] Hospital (Psychiatric Department) Kowloon Name of Hospital/Clinic Tel. No. Email Address 5. Tseung Kwan O Hospital 2208 0335 [email protected] 2208 0327 6. United Christian Hospital 3949 5178 [email protected] (Psychiatry) 7. Queen Elizabeth Hospital 3506 7021 [email protected] 3506 7027 3506 5499 3506 4021 8. Hong Kong Eye Hospital 2762 3069 [email protected] 9. Kowloon Hospital Rehabilitation 3129 7857 [email protected] Building 10. Kowloon Hospital 3129 6193 [email protected] 11. Kowloon Hospital 2768 8534 [email protected] (Psychiatric Department) 1 The New Territories Name of Hospital/Clinic Tel. No. Email Address 12. Prince of Wales Hospital 3505 2400 [email protected] 13. Shatin Hospital 3919 7521 [email protected] 14. Tai Po Hospital 2607 6304 [email protected] Sub-office Tai Po Hospital (Child and Adolescent 2689 2486 [email protected] Mental Health Centre) 15. North District Hospital 2683 7750 [email protected] 16. Tin Shui Wai Hospital 3513 5391 [email protected] 17. Castle Peak Hospital 2456 7401 [email protected] 18. Siu Lam Hospital 2456 7186 [email protected] 19.