Correlation Between Iodine Status and Dysfunctional Parameters of the Thyroid Gland of Djidja Schoolchildren
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Palace Sculptures of Abomey
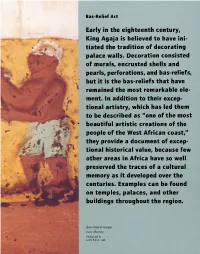
Bas-Relief Art Early in the eighteenth century, King Agaja is believed to have ini tiated the tradition of decorating palace walls. Decoration consisted of murals, encrusted shells and pearls, perfo rations, and bas-reliefs, , but it is the bas-reliefs that have remained the most remarkable ele ment. In addition to their excep tional artistry, which has led them to be described as "one of the most " beautiful artistic creations of the people of the West African coast, rr they provide a document of excep tional historical value, because few other areas in Africa have so well preserved the traces of a cultural · . memory as it developed over the centuries. Exa mples can be found on temples, palaces, and other buildings throughout the region. Bas-relief at temple near Abomey. Photograph by Leslie Railler, 1996. BAS-RELIEF ART 49 Commonly called noudide in Fon, from the root word meaning "to design" or "to portray," the bas-reliefs are three-dimensional, modeled- and painted earth pictograms. Early examples of the form, first in religious temples and then in the palaces, were more abstract than figurative. Gradually, figurative depictions became the prevalent style, illustrating the tales told by the kings' heralds and other Fon storytellers. Palace bas-reliefs were fashioned according to a long-standing tradition of The original earth architectural and sculptural renovation. used to make bas Ruling monarchs commissioned new palaces reliefs came from ter and artworks, as well as alterations of ear mite mounds such as lier ones, thereby glorifying the past while this one near Abomey. bringing its art and architecture up to date. -

B E N I N Benin
Birnin o Kebbi !( !( Kardi KANTCHARIKantchari !( !( Pékinga Niger Jega !( Diapaga FADA N'GOUMA o !( (! Fada Ngourma Gaya !( o TENKODOGO !( Guéné !( Madécali Tenkodogo !( Burkina Faso Tou l ou a (! Kende !( Founogo !( Alibori Gogue Kpara !( Bahindi !( TUGA Suroko o AIRSTRIP !( !( !( Yaobérégou Banikoara KANDI o o Koabagou !( PORGA !( Firou Boukoubrou !(Séozanbiani Batia !( !( Loaka !( Nansougou !( !( Simpassou !( Kankohoum-Dassari Tian Wassaka !( Kérou Hirou !( !( Nassoukou Diadia (! Tel e !( !( Tankonga Bin Kébérou !( Yauri Atakora !( Kpan Tanguiéta !( !( Daro-Tempobré Dammbouti !( !( !( Koyadi Guilmaro !( Gambaga Outianhou !( !( !( Borogou !( Tounkountouna Cabare Kountouri Datori !( !( Sécougourou Manta !( !( NATITINGOU o !( BEMBEREKE !( !( Kouandé o Sagbiabou Natitingou Kotoponga !(Makrou Gurai !( Bérasson !( !( Boukombé Niaro Naboulgou !( !( !( Nasso !( !( Kounounko Gbangbanrou !( Baré Borgou !( Nikki Wawa Nambiri Biro !( !( !( !( o !( !( Daroukparou KAINJI Copargo Péréré !( Chin NIAMTOUGOU(!o !( DJOUGOUo Djougou Benin !( Guerin-Kouka !( Babiré !( Afekaul Miassi !( !( !( !( Kounakouro Sheshe !( !( !( Partago Alafiarou Lama-Kara Sece Demon !( !( o Yendi (! Dabogou !( PARAKOU YENDI o !( Donga Aledjo-Koura !( Salamanga Yérémarou Bassari !( !( Jebba Tindou Kishi !( !( !( Sokodé Bassila !( Igbéré Ghana (! !( Tchaourou !( !(Olougbé Shaki Togo !( Nigeria !( !( Dadjo Kilibo Ilorin Ouessé Kalande !( !( !( Diagbalo Banté !( ILORIN (!o !( Kaboua Ajasse Akalanpa !( !( !( Ogbomosho Collines !( Offa !( SAVE Savé !( Koutago o !( Okio Ila Doumé !( -

S a Rd in Ia
M. Mandarino/Istituto Euromediterraneo, Tempio Pausania (Sardinia) Land07-1Book 1.indb 97 12-07-2007 16:30:59 Demarcation conflicts within and between communities in Benin: identity withdrawals and contested co-existence African urban development policy in the 1990s focused on raising municipal income from land. Population growth and a neoliberal environment weakened the control of clans and lineages over urban land ownership to the advantage of individuals, but without eradicating the importance of personal relationships in land transactions or of clans and lineages in the political structuring of urban space. The result, especially in rural peripheries, has been an increase in land aspirations and disputes and in their social costs, even in districts with the same territorial control and/or the same lines of nobility. Some authors view this simply as land “problems” and not as conflicts pitting locals against outsiders and degenerating into outright clashes. However, decentralization gives new dimensions to such problems and is the backdrop for clashes between differing perceptions of territorial control. This article looks at the ethnographic features of some of these clashes in the Dahoman historic region of lower Benin, where boundaries are disputed in a context of poorly managed urban development. Such disputes stem from land registries of the previous but surviving royal administration, against which the fragile institutions of the modern state seem to be poorly equipped. More than a simple problem of land tenure, these disputes express an internal rejection of the legitimacy of the state to engage in spatial structuring based on an ideal of co-existence; a contestation that is put forward with the de facto complicity of those acting on behalf of the state. -

The Geography of Welfare in Benin, Burkina Faso, Côte D'ivoire, and Togo
Public Disclosure Authorized Public Disclosure Authorized The Geography of Welfare in Benin, Burkina Faso, Côte d’Ivoire, and Togo Public Disclosure Authorized Nga Thi Viet Nguyen and Felipe F. Dizon Public Disclosure Authorized 00000_CVR_English.indd 1 12/6/17 2:29 PM November 2017 The Geography of Welfare in Benin, Burkina Faso, Côte d’Ivoire, and Togo Nga Thi Viet Nguyen and Felipe F. Dizon 00000_Geography_Welfare-English.indd 1 11/29/17 3:34 PM Photo Credits Cover page (top): © Georges Tadonki Cover page (center): © Curt Carnemark/World Bank Cover page (bottom): © Curt Carnemark/World Bank Page 1: © Adrian Turner/Flickr Page 7: © Arne Hoel/World Bank Page 15: © Adrian Turner/Flickr Page 32: © Dominic Chavez/World Bank Page 48: © Arne Hoel/World Bank Page 56: © Ami Vitale/World Bank 00000_Geography_Welfare-English.indd 2 12/6/17 3:27 PM Acknowledgments This study was prepared by Nga Thi Viet Nguyen The team greatly benefited from the valuable and Felipe F. Dizon. Additional contributions were support and feedback of Félicien Accrombessy, made by Brian Blankespoor, Michael Norton, and Prosper R. Backiny-Yetna, Roy Katayama, Rose Irvin Rojas. Marina Tolchinsky provided valuable Mungai, and Kané Youssouf. The team also thanks research assistance. Administrative support by Erick Herman Abiassi, Kathleen Beegle, Benjamin Siele Shifferaw Ketema is gratefully acknowledged. Billard, Luc Christiaensen, Quy-Toan Do, Kristen Himelein, Johannes Hoogeveen, Aparajita Goyal, Overall guidance for this report was received from Jacques Morisset, Elisée Ouedraogo, and Ashesh Andrew L. Dabalen. Prasann for their discussion and comments. Joanne Gaskell, Ayah Mahgoub, and Aly Sanoh pro- vided detailed and careful peer review comments. -

Monographie Des Communes Des Départements De L'atlantique Et Du Li
Spatialisation des cibles prioritaires des ODD au Bénin : Monographie des communes des départements de l’Atlantique et du Littoral Note synthèse sur l’actualisation du diagnostic et la priorisation des cibles des communes Monographie départementale _ Mission de spatialisation des cibles prioritaires des ODD au Bénin _ 2019 1 Une initiative de : Direction Générale de la Coordination et du Suivi des Objectifs de Développement Durable (DGCS-ODD) Avec l’appui financier de : Programme d’appui à la Décentralisation et Projet d’Appui aux Stratégies de Développement au Développement Communal (PDDC / GIZ) (PASD / PNUD) Fonds des Nations unies pour l'enfance Fonds des Nations unies pour la population (UNICEF) (UNFPA) Et l’appui technique du Cabinet Cosinus Conseils Monographie départementale _ Mission de spatialisation des cibles prioritaires des ODD au Bénin _ 2019 2 Tables des matières LISTE DES CARTES ..................................................................................................................................................... 4 SIGLES ET ABREVIATIONS ......................................................................................................................................... 5 1.1. BREF APERÇU SUR LES DEPARTEMENTS DE L’ATLANTIQUE ET DU LITTORAL ................................................ 7 1.1.1. INFORMATIONS SUR LE DEPARTEMENT DE L’ATLANTIQUE ........................................................................................ 7 1.1.1.1. Présentation du Département de l’Atlantique ...................................................................................... -

Water Supply and Waterbornes Diseases in the Population of Za- Kpota Commune (Benin, West Africa)
International Journal of Engineering Science Invention (IJESI) ISSN (Online): 2319 – 6734, ISSN (Print): 2319 – 6726 www.ijesi.org ||Volume 7 Issue 6 Ver II || June 2018 || PP 33-39 Water Supply and Waterbornes Diseases in the Population of Za- Kpota Commune (Benin, West Africa) Léocadie Odoulami, Brice S. Dansou & Nadège Kpoha Laboratoire Pierre PAGNEY, Climat, Eau, Ecosystème et Développement LACEEDE)/DGAT/FLASH/ Université d’Abomey-Calavi (UAC). 03BP: 1122 Cotonou, République du Bénin (Afrique de l’Ouest) Corresponding Auther: Léocadie Odoulami Summary :The population of the common Za-kpota is subjected to several difficulties bound at the access to the drinking water. This survey aims to identify and to analyze the problems of provision in drinking water and the risks on the human health in the township of Za-kpota. The data on the sources of provision in drinking water in the locality, the hydraulic infrastructures and the state of health of the populations of 2000 to 2012 have been collected then completed by information gotten by selected 198 households while taking into account the provision difficulties in water of consumption in the households. The analysis of the results gotten watch that 43 % of the investigation households consume the water of well, 47 % the water of cistern, 6 % the water of boring, 3% the water of the Soneb and 1% the water of marsh. However, the physic-chemical and bacteriological analyses of 11 samples of water of well and boring revealed that the physic-chemical and bacteriological parameters are superior to the norms admitted by Benin. The consumption of these waters exposes the health of the populations to the water illnesses as the gastroenteritis, the diarrheas, the affections dermatologic,.. -

Monographie Des Départements Du Zou Et Des Collines
Spatialisation des cibles prioritaires des ODD au Bénin : Monographie des départements du Zou et des Collines Note synthèse sur l’actualisation du diagnostic et la priorisation des cibles des communes du département de Zou Collines Une initiative de : Direction Générale de la Coordination et du Suivi des Objectifs de Développement Durable (DGCS-ODD) Avec l’appui financier de : Programme d’appui à la Décentralisation et Projet d’Appui aux Stratégies de Développement au Développement Communal (PDDC / GIZ) (PASD / PNUD) Fonds des Nations unies pour l'enfance Fonds des Nations unies pour la population (UNICEF) (UNFPA) Et l’appui technique du Cabinet Cosinus Conseils Tables des matières 1.1. BREF APERÇU SUR LE DEPARTEMENT ....................................................................................................... 6 1.1.1. INFORMATIONS SUR LES DEPARTEMENTS ZOU-COLLINES ...................................................................................... 6 1.1.1.1. Aperçu du département du Zou .......................................................................................................... 6 3.1.1. GRAPHIQUE 1: CARTE DU DEPARTEMENT DU ZOU ............................................................................................... 7 1.1.1.2. Aperçu du département des Collines .................................................................................................. 8 3.1.2. GRAPHIQUE 2: CARTE DU DEPARTEMENT DES COLLINES .................................................................................... 10 1.1.2. -

Socio-Demographic and Economic Characteristics, Crop-Livestock Production Systems and Issues for Rearing Improvement: a Review
Available online at http://www.ifgdg.org Int. J. Biol. Chem. Sci. 12(1): 519-541, February 2018 ISSN 1997-342X (Online), ISSN 1991-8631 (Print) Review Paper http://ajol.info/index.php/ijbcs http://indexmedicus.afro.who.int Socio-demographic and economic characteristics, crop-livestock production systems and issues for rearing improvement: A review Daniel Bignon Maxime HOUNDJO1, Sébastien ADJOLOHOUN1*, Basile GBENOU1, Aliou SAIDOU2, Léonard AHOTON2, Marcel HOUINATO1, Soumanou SEIBOU TOLEBA1 and Brice Augustin SINSIN3 1Département de Production Animale, Faculté des Sciences Agronomiques, Université d’Abomey-Calavi, 03 BP 2819 Jéricho, Cotonou, Benin. 2Département de Production Végétale, Faculté des Sciences Agronomiques, Université d’Abomey-Calavi, 03 BP 2819 Jéricho, Cotonou, Benin. 3Département de l’Aménagement et Gestion des Ressources Naturelles, Faculté des Sciences Agronomiques, Université d’Abomey-Calavi, 03 BP 2819 Jéricho, Cotonou, Benin. *Corresponding author; E-mail : [email protected]; Tél: (+229) 97 89 88 51 ABSTRACT This paper reviews some characteristics of crop-livestock production systems in Benin with a special focus on the issues for enhance pasture production and nutritive value which in turn will increase animal productivity. Benin is located in the Gulf of Guinea of the Atlantic Ocean in West Africa and covers 114,763 km2. The population estimated in 2017 is 10,900,000 inhabitants with an annual population growth rate of 3.5%. The country is primarily an agro-based economy, characterized by subsistence agricultural production that employs more than 70%. The climate ranges from the bimodal rainfall equatorial type in the south to the tropical unimodal monsoon type in the north. -

Rapport Définitif De La Sélection Des 70 Formations Sanitaires (FS) Témoins Pour Les FS Du Projet FBR Du Bénin Par Joseph FLENON, Consultant
Rapport définitif de la sélection des 70 formations sanitaires (FS) témoins pour les FS du Projet FBR du Bénin par Joseph FLENON, Consultant. Dans la première partie du point n°1 de ce contrat en cours d’exécution, j’ai sélectionné de manière aléatoire simple 8 Zones Sanitaires (ZS) témoins (au lieu de 5 ou 6) pour les 8 ZS du projet FBR du Bénin et j’en ai fait un rapport Dans cette deuxième partie du point n°1, j’ai procédé à la sélection de 70 formations sanitaire (FS) dans 10 ZS témoins (au lieu de 8ZS témoins) car suivant les critères de sélection de ces FS, les 8ZS sélectionnées dans la première partie du point n°1, m’ont permis de sélectionner à leur tour 47 FS témoins au lieu de 70 FS témoins. La Sélection aléatoire simple d’une ZS contrôle dans chacun des 8 listes a donné les 8 ZS contrôles suivantes : 1.ZS Bohicon-Zakpota-Zogbodomey : ZS contrôle : ZS Djidja-Abomey-Agbangnizoun 2.ZS Covè-Ouinhi-Zangnanado : ZS contrôle : ZS Pobè-Ketou-Adja-Ouèrè 3.ZS Lokossa-Athiémé : ZS contrôle : ZS Aplahoué-Djakotomè-Dogbo 4.ZS Ouidah-Kpomassè-Tori-Bossito : ZS contrôle : ZS Allada-Toffo-Zê 5.ZS Porto-Novo-Aguégués-Sèmè-Podji : ZS contrôle : ZS Cotonou 6 6.ZS Adjohoun-Bonou-Dangbo : ZS contrôle : ZS Abomey-Calavi-Sô-Ava 7.ZS Banikoara : ZS contrôle : ZS Kandi-Gogounou-Ségbana 8.ZS Kouandé-Ouassa-Péhunco-Kérou : ZS contrôle : ZS Tanguiéta-Cobly-Matéri Les critères de sélections des FS témoins proposés dans les TDR peuvent être classés en critères exclusifs (être à moins de 15 km de la frontière d’une ZS du Projet FBR et avoir moins de 2 personnels qualifiés) et en critères non exclusifs (certaines FS témoins doivent avoir au moins 15 CPN par jour). -

Paper Download
ECAS 2017 #BidoungChallenge in Cameroon ■ Profile ■ 1972: Born in Osaka, Japan 1994-96: Japanese Embassy to Senegal Political impact of 2000-01:University of Bordeaux (Science Po) 2003: Ph.D. in Political Science (Kobe University, Japan) 2011-12: Centre Emile Durkheim, IEP Bordeaux (Visiting fellow) decentralization 2013- : Associate Prof at Ritsumeikan University, Japan in urbanizing Africa ◆Research subjects (African politics & Int’l relations): Democratization, Decentralization , Power & Symbol, Witchcraft July 1, 2017 and politics, Asia-Africa relations, African studies in Asian countries, Border, Local govt’s int’l cooperation , SNS in Politics, Takuo IWATA Laughter in politics, Eating acts (manducation) in politics etc. (Ritsumeikan Univ, Kyoto, Japan) ◆Field work area: West Africa ( Benin , Burkina Faso , Togo, [email protected] occasionally Ghana, Mali), Asian countries 1 2 Source: Journal du Jeudi (No.1289, June 2-8, 2016) Source: Africa Daily News (@AfricaDNews, Feb 8, 2017) ■ Today’s content ■ 1. Introduction 1. Introduction 1-1. Research question ◆ How decentralization & urbanization affect local political 2. Decentralization Process in African Countries power balance, then national politics in African countries (with[out] ongoing democratization process)? 3. Political Impact of Decentralization 1-2. Research approach & objective 4. Development of Decentralized Cooperation ◆ Focusing on politics in urban local governments ( communes ) 5. Political Turbulences in Decentralizing 1-3. Research topic Local Governance ◆ Politicizing local governance in decentralization reform ◆ Decentralization in urban Africa, decentralized cooperation 6. Conclusion (local diplomacy), Storm of discharges of Mayors ◆ Case studies in Benin & Burkina Faso 3 4 InterviewSource: with Journal Mayor du Jeudi of Abomey (Burkina (Benin)Faso), No.959, [October February 2005, 4-10, 2010.Cotonou] 2. -

Chemical Composition and Antimicrobial Activity of The
Clément et al. Universal Journal of Pharmaceutical Research Available online on 15.9.2019 at http://ujpr.org Universal Journal of Pharmaceutical Research An International Peer Reviewed Journal Open access to Pharmaceutical research This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial Share Alike 4.0 License which permits unrestricted non commercial use, provided the original work is properly cited Volume 4, Issue 4, 2019 RESEARCH ARTICLE CHEMICAL COMPOSITION AND ANTIMICROBIAL ACTIVITY OF THE ESSENTIAL OILS OF FOUR VARIETIES OF LIPPIA MULTIFLORA IN BENIN GANDONOU Dossa Clément1*, BAMBOLA Bouraïma2, TOUKOUROU Habib3 , GBAGUIDI Ahokannou 2 1 4 5 1 Fernand , DANSOU Christian , AWEDE Bonaventure , LALEYE Anatole , AHISSOU Hyacinthe 1Laboratory of Enzymology and Biochemistry of Proteins, Faculty of Science and Technology, University of Abomey-Calavi, 01BP: 188, Cotonou, Benin. 2Pharmacognosie Laboratory /Institute of Research and Experimentation in Traditional Medicine and Pharmacopoeia (IREMPT) / Benin Center for Scientific Research and Innovation (CBRSI) / Faculty of Science and Technology, University of Abomey-Calavi, 01 BP 06 Oganla Porto-novo, Benin. 3Laboratory of Organic Pharmaceutical Chemistry, School of Pharmacy, Faculty of Health Sciences, University of Abomey- Calavi, Fairground Campus, 01 BP: 188, Cotonou, Benin. 4Unit of Teaching and Research in Physiology Faculty of Health Sciences, University of Abomey-Calavi, Cotonou, Benin. 5Cellogenetics and Cell Biology Laboratory, Faculty of Health Sciences, University of Abomey-Calavi 01BP 188 Cotonou, Benin. ABSTRACT Objective: Present study involves the study of the chemical composition of the essential oils extracted from the leaves by gas chromatography and gas chromatography coupled with mass spectrometry of Lippia multiflora harvested in the regions of Kétou, Savalou, Bohicon and Mono and tested by the well diffusion method against pathogenic microorganisms. -

Evaluation Design Report for the Benin Power Compact's Electricity Generation Project and Electricity Distribution Project
FINAL REPORT Evaluation Design Report for the Benin Power Compact's Electricity Generation Project and Electricity Distribution Project March 7, 2018 Christopher Ksoll Kristine Bos Arif Mamun Anthony Harris Sarah Hughes Submitted to: Millennium Challenge Corporation 1099 14th Street, NW Suite 700 Washington, DC 20005 Project Monitor: Hamissou Samari Contract Number: MCC-16-CON-0058 Submitted by: Mathematica Policy Research 1100 1st Street, NE, 12th Floor Washington, DC 20002-4221 Telephone: (202) 484-9220 Facsimile: (202) 863-1763 Project Director: Sarah Hughes Reference Number: 50339.01.200.031.000 This page has been left blank for double-sided copying. BENIN ENERGY II: EVALUATION DESIGN REPORT MATHEMATICA POLICY RESEARCH CONTENTS ACRONYMS ............................................................................................................................................... VII I. INTRODUCTION ........................................................................................................................................ 1 II. OVERVIEW OF THE COMPACT, GENERATION ACTIVITY, AND DISTRIBUTION ACTIVITY ......................................................................................................................................... 5 A. Overview of the Benin Power Compact ..................................................................................... 5 B. Overview of the theory of change .............................................................................................. 9 C. Economic rate of return and