Congenital Eyelid Anomalies: What General Physician Needs to Know
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cone Interaction with Progressive Macular Dysfunction
Correspondence 823 Sir, occasionally in the context of ectodermal dysplasia Management of ankyloblepharon filiforme adnatum syndromes3 and popliteal pterygium syndrome.4 AFA has also been reported in association with Edward’s Ankyloblepharon filiforme adnatum (AFA) is a syndrome,5 and CHANDS6 (curly hair, ankyloblepharon, rare congenital malformation affecting the eyelids. nail dysplasia). Other associations include hydrocephalus, We report a case describing its management. meningomyelocoele, and imperforate anus,7 cardiac defects and syndactyly.4 Detailed systemic assessment by an experienced paediatrician is therefore imperative in Case report the management of AFA. Our report illustrates a simple surgical approach that A male neonate was referred for assessment of his left is modified from previously published cases.1,2,4 It is safe eyelids. He was born at term, to a primigravid mother, and well tolerated with the aid of topical anaesthesia. weighing 3150 g. Pregnancy and delivery were Surgical correction should be performed promptly to unremarkable. There was no family history of minimise any risk of occlusion amblyopia, and enable ophthalmic or systemic disease. A detailed systemic full examination of the eye. assessment by a paediatrician was clear. Ocular examination showed partial fusion of his left upper and lower eyelids by a central, narrow band Conflict of interest of tissue, arising from the grey lines (Figure 1). Full The authors declare no conflict of interest. eyelid opening was impaired and interpalpebral aperture was limited to 3.5 mm. Right eye examination was normal. The band of tissue was retracted anteriorly with References a squint hook, clamped for 10 s, and excised with Vannas 1 Scott MH, Richard JM, Farris BK. -

Treatment of Congenital Ptosis
13 Review Article Page 1 of 13 Treatment of congenital ptosis Vladimir Kratky1,2^ 1Department of Ophthalmology, Queen’s University, Kingston, Canada; 21st Medical Faculty, Charles University, Prague, Czech Republic Correspondence to: Vladimir Kratky, BSc, MD, FRCSC, DABO. Associate Professor of Ophthalmology, Director of Ophthalmic Plastic and Orbital Surgery, Oculoplastics Fellowship Director, Queen’s University, Kingston, Canada; 1st Medical Faculty, Charles University, Prague, Czech Republic. Email: [email protected]. Abstract: Congenital ptosis is an abnormally low position of the upper eyelid, with respect to the visual axis in the primary gaze. It can be present at birth or manifest itself during the first year of life and can be bilateral or unilateral. Additionally, it may be an isolated finding or part of a constellation of signs of a specific syndrome or systemic associations. Depending on how much it interferes with the visual axis, it may be considered as a functional or a cosmetic condition. In childhood, functional ptosis can lead to deprivation amblyopia and astigmatism and needs to be treated. However, even mild ptosis with normal vision can lead to psychosocial problems and correction is also advised, albeit on a less urgent basis. Although, patching and glasses can be prescribed to treat the amblyopia, the mainstay of management is surgical. There are several types of surgical procedure available depending on the severity and etiology of the droopy eyelid. The first part of this paper will review the different categories of congenital ptosis, including more common associated syndromes. The latter part will briefly cover the different surgical approaches, with emphasis on how to choose the correct condition. -

Corneal Ectasia
Corneal Ectasia Secretary for Quality of Care Anne L. Coleman, MD, PhD Academy Staff Nicholas P. Emptage, MAE Nancy Collins, RN, MPH Doris Mizuiri Jessica Ravetto Flora C. Lum, MD Medical Editor: Susan Garratt Design: Socorro Soberano Approved by: Board of Trustees September 21, 2013 Copyright © 2013 American Academy of Ophthalmology® All rights reserved AMERICAN ACADEMY OF OPHTHALMOLOGY and PREFERRED PRACTICE PATTERN are registered trademarks of the American Academy of Ophthalmology. All other trademarks are the property of their respective owners. This document should be cited as follows: American Academy of Ophthalmology Cornea/External Disease Panel. Preferred Practice Pattern® Guidelines. Corneal Ectasia. San Francisco, CA: American Academy of Ophthalmology; 2013. Available at: www.aao.org/ppp. Preferred Practice Pattern® guidelines are developed by the Academy’s H. Dunbar Hoskins Jr., MD Center for Quality Eye Care without any external financial support. Authors and reviewers of the guidelines are volunteers and do not receive any financial compensation for their contributions to the documents. The guidelines are externally reviewed by experts and stakeholders before publication. Corneal Ectasia PPP CORNEA/EXTERNAL DISEASE PREFERRED PRACTICE PATTERN DEVELOPMENT PROCESS AND PARTICIPANTS The Cornea/External Disease Preferred Practice Pattern® Panel members wrote the Corneal Ectasia Preferred Practice Pattern® guidelines (“PPP”). The PPP Panel members discussed and reviewed successive drafts of the document, meeting in person twice and conducting other review by e-mail discussion, to develop a consensus over the final version of the document. Cornea/External Disease Preferred Practice Pattern Panel 2012–2013 Robert S. Feder, MD, Co-chair Stephen D. McLeod, MD, Co-chair Esen K. -

Novel Anterior Segment Phenotypes Resulting from Forkhead Gene Alterations: Evidence for Cross-Species Conservation of Function
Novel Anterior Segment Phenotypes Resulting from Forkhead Gene Alterations: Evidence for Cross-Species Conservation of Function Ordan J. Lehmann,1 Stephen Tuft,2 Glen Brice,3 Richard Smith,4 Åsa Blixt,5 Rachel Bell,3 Bengt Johansson,6 Tim Jordan,1 Roger A. Hitchings,2 Peng T. Khaw,2 Simon W. M. John,4 Peter Carlsson,5 and Shomi S. Bhattacharya1 PURPOSE. Mutations in murine and human versions of an ances- cause it may affect the clinical management of certain trally related gene usually result in similar phenotypes. How- glaucoma subtypes and lead to excessive treatment. The ever, interspecies differences exist, and in the case of two FOXC1 and Foxe3 data, taken together with the novel ocular forkhead transcription factor genes (FOXC1 and FOXC2), phenotypes of FOXC2 mutations, highlight the remarkable these differences include corneal or anterior segment pheno- cross-species conservation of function among forkhead genes. types, respectively. This study was undertaken to determine (Invest Ophthalmol Vis Sci. 2003;44:2627–2633) DOI:10.1167/ whether such discrepancies provide an opportunity for iden- iovs.02-0609 tifying novel human–murine ocular phenotypes. METHODS. Four pedigrees with early-onset glaucoma pheno- types secondary to segmental chromosomal duplications or ecognition that mutations in orthologous genes frequently deletions encompassing FOXC1 and 18 individuals from 9 Rcause similar phenotypes has allowed the field of compar- FOXC2 mutation pedigrees underwent detailed ocular pheno- ative genetics to contribute to the understanding of human typing. Subsequently, mice with mutations in Foxc1 or a re- disease. As the human, murine, and Drosophila PAX6 mutants lated forkhead gene, Foxe3, were assessed for features of the (aniridia, Small eye, and eyeless) demonstrate, genotypic con- human phenotypes. -

Whole Exome Sequencing Gene Package Vision Disorders, Version 6.1, 31-1-2020
Whole Exome Sequencing Gene package Vision disorders, version 6.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCA4 Cone-rod dystrophy 3, 604116 601691 94 100 100 97 Fundus flavimaculatus, 248200 {Macular degeneration, age-related, 2}, 153800 Retinal dystrophy, early-onset severe, 248200 Retinitis pigmentosa 19, 601718 Stargardt disease -

Blepharophimosis, Ptosis, and Epicanthus Inversus Syndrome
Blepharophimosis, ptosis, and epicanthus inversus syndrome Case Report A rare case of adult-onset blepharophimosis, ptosis, and epicanthus inversus syndrome: Case report Mahesha S1, Shruthi Bhimalli2, Manoj Y Bhat2 From 1Chief Medical Officer, 2Fellow in IOL, Department of Cataract and Trauma, Sankara Eye Hospital, Harakere, Shimoga, Karnataka, India Correspondence to: Dr. Shruthi Bhimalli, Department of Cataract and Trauma, Sankara Eye Hospital, Harakere, Shimoga - 577202, Karnataka, India. E-mail: [email protected] Received - 02 June 2019 Initial Review - 24 June 2019 Accepted - 25 July 2019 ABSTRACT Blepharophimosis, ptosis, and epicanthus inversus syndrome (BPES) is a rare genetic condition caused by a mutation in the FOXL2 gene and it is inherited in an autosomal dominant pattern. Identification and diagnosis of BPES syndrome by an ophthalmologist are relatively easy, based on the characteristic ocular manifestations. The most common age group at the time of diagnosis is 4 to 8 years. Here, we present an unusual case of BPES in a patient who presented with the syndrome at the age of 52 years. There is a need for increased awareness about this condition among ophthalmologists as early diagnosis is the key factor in preventing long term complications. Keywords: Blepharophimosis, Epicanthus inversus syndrome, Ptosis. lepharophimosis, ptosis, and epicanthus inversus action, epicanthus inversus and telecanthus (Fig. 1). On acuity syndrome (BPES) is a genetic condition associated testing, his best vision was ‘finger counting close to face’ in his Bwith mutations in the Fork head Box L2 (FOXL2) gene. right eye and ‘finger counting at one meter’ in his left eye. He had The syndrome is inherited in an autosomal dominant pattern, with corneal ectasia with scarring and vascularization (Fig. -
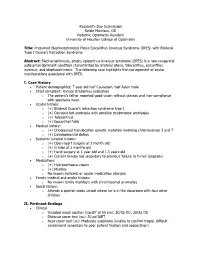
P> Resident’S Day Submission Kelsie Morrison, OD Pediatric Optometry Resident University of Houston College of Optometry
Resident’s Day Submission Kelsie Morrison, OD Pediatric Optometry Resident University of Houston College of Optometry Title: Presumed Blepharophimosis Ptosis Epicanthus Inversus Syndrome (BPES) with Bilateral Type I Duane’s Retraction Syndrome Abstract: Blepharophimosis, ptosis, epicanthus inversus syndrome (BPES) is a rare congenital autosomal dominant condition characterized by bilateral ptosis, telecanthus, epicanthus inversus, and blepharphimosis. The following case highlights the management of ocular manifestations associated with BPES. I. Case History Patient demographics: 7 year old half Caucasian, half Asian male Chief complaint: Annual strabismus evaluation o The patient’s father reported good vision without glasses and non-compliance with spectacle wear. Ocular history: o (+) Bilateral Duane’s retraction syndrome type I o (+) Constant left esotropia with possible strabmismic amblyopia o (+) Telecanthus o (+) Epicanthal folds Medical history: o (+) Unbalanced translocation genetic mutation involving chromosomes 3 and 7 o (+) Developmental delays Systemic surgical history: o (+) Open heart surgery at 1 month old o (+) G-tube at 2 months old o (+) Hand surgery at 1 year old and 1.5 years old o (+) Current G-tube fed secondary to previous ‘failure to thrive’ diagnosis Medications o (+) Hydrocortisone cream o (+) Murolax o No known systemic or ocular medication allergies Family medical and ocular history: o No known family members with chromosomal anomalies Social history: o Attends a special needs school where he is in the -

Congenital Ocular Anomalies in Newborns: a Practical Atlas
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2020;9(2):e090207 doi: 10.7363/090207 Received: 2019 Jul 19; revised: 2019 Jul 23; accepted: 2019 Jul 24; published online: 2020 Sept 04 Mini Atlas Congenital ocular anomalies in newborns: a practical atlas Federico Mecarini1, Vassilios Fanos1,2, Giangiorgio Crisponi1 1Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy 2Department of Surgery, University of Cagliari, Cagliari, Italy Abstract All newborns should be examined for ocular structural abnormalities, an essential part of the newborn assessment. Early detection of congenital ocular disorders is important to begin appropriate medical or surgical therapy and to prevent visual problems and blindness, which could deeply affect a child’s life. The present review aims to describe the main congenital ocular anomalies in newborns and provide images in order to help the physician in current clinical practice. Keywords Congenital ocular anomalies, newborn, anophthalmia, microphthalmia, aniridia, iris coloboma, glaucoma, blepharoptosis, epibulbar dermoids, eyelid haemangioma, hypertelorism, hypotelorism, ankyloblepharon filiforme adnatum, dacryocystitis, dacryostenosis, blepharophimosis, chemosis, blue sclera, corneal opacity. Corresponding author Federico Mecarini, MD, Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy; tel.: (+39) 3298343193; e-mail: [email protected]. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

An Operation for Congenital Ptosis by George Young
Br J Ophthalmol: first published as 10.1136/bjo.8.6.272 on 1 June 1924. Downloaded from 272 THE BRITISH JOURNAL OF OPHTHALMIOI,OGY added plus lenses (eye being under atropin), J.2, fluently. This made her left eye equal, for distance, to her better eye, which is now getting worse owing to increased bulging, and will probably follow the course of the other one soon. R.V.: 6/36, c. -1.OD sph. + 3.50D cyl. 1550: 6/24 and J.5. Furthermore, it may be noted that the intraocular tension was now normal on the side of the iridectomy, while the right eye was hard, and I submitted it again to pilocarpin and bandage at night. I sent her home for a fortnight to feed up, take malt and cod liver oil and fats, and to take plenty of rest and recuperate. On July 8 the final result was: L.V.: 6/36, c.-5.OD sph. +3.50D cyl. 1600: 6/12 full, and -3.OD sph. and +3.50D cyl. J.2. Soon I shall tattoo the stellate leucoma with an artificial pupil. May 10, 1924. Since writing the above, some ten months ago, affairs have kept steady. There is no bulging of the left cornea or scar. I attempted tattooing at two sittings, and have considerably diminished the glare of the scar, but I refrain from risking the deep tattooing necessary for securing an imitation round black pupil, fearing to do harm. Glasses were prescribed and worn with comfort and great help, the vision being maintained as above. -

Ocular Emergencies for the Primary Care Optometrist
Ocular Emergencies Ocular Emergencies for the Disclosure Statement Primary Care Optometrist . Honorarium, Speaker, Consultant, Research Grant: Aerie, Alcon, Allergan, B+L, Carl Zeiss, Glaukos, Heidelberg, Novartis, Topcon, Michael Chaglasian, OD, FAAO Associate Professor Illinois Eye Institute Illinois College of Optometry [email protected] What is a “True” Emergency? “True” Emergency . Pain (vs. discomfort) . History is key to differentiating emergency versus urgency . Current or potential for: Phone or in person Vision loss Proper triage is essential Structural damage After hours protocol Needs immediate (same day) attention Your office and your specialists Medico-legal implications History Emergency Exam Vision Recent ocular disease or One or both eyes? surgery . Acuity . External examination Visual field Other diseases . Visual fields . SLE Sudden or gradual cardiac, vascular, or . Pupils Blurred or lost? autoimmune . IOP Diplopia? viruses . Ocular Motility . Fundus exam Mono or Bino Medications or recent Pain changes to medications Redness Nausea/vomiting Onset Trauma Contact lenses M. Chaglasian, OD 1 Ocular Emergencies Emergency Kit “True” Emergency . Chemical Burns . Eye shield . pH paper Alkaline . Pressure patch . Bandage CL’s . Sterile eye wash . Diamox . Central Retinal Artery Occlusion . Alger brush . Topical drops . Forceps Antibiotics NSAID’s . Golf spud . Both have extremely high risk of severe and permanent Steroids vision loss which can be prevented via immediate Cycloplegics intervention and treatment Chemical Trauma Chemical Burns . Copious irrigation anesthetic . Acid exposure speculum Only penetrate through epithelium sterile saline v tap water car battery, vinegar, and some refrigerants . Contacts can be removed after irrigation . Sweep fornices – repeatedly . Alkaline exposure Penetrates tissues more easily and . Examination after irrigation and neutralization of pH have a prolonged effect . -

The Management of Congenital Malpositions of Eyelids, Eyes and Orbits
Eye (\988) 2, 207-219 The Management of Congenital Malpositions of Eyelids, Eyes and Orbits S. MORAX AND T. HURBLl Paris Summary Congenital malformations of the eye and its adnexa which are multiple and varied can affect the whole eyeball or any part of it, as well as the orbit, eyelids, lacrimal ducts, extra-ocular muscles and conjunctiva. A classification of these malformations is presented together with the general principles of treatment, age of operating and surgical tactics. The authors give some examples of the anatomo-clinical forms, eyelid malpositions such as entropion, ectropion, ptosis, levator eyelid retraction, medial canthus malposition, congenital eyelid colobomas, and congenital orbital abnormalities (Craniofacial stenosis, orbi tal plagiocephalies, hypertelorism, anophthalmos, microphthalmos and cryptophthalmos) . Congenital malformations of the eye and its as echography, CT-scan and NMR, enzymatic adnexa are multiple and varied. They can work-up or genetic studies (Table I). affect the whole eyeball or any part of it, as Surgical treatment when feasible will well as the orbit, eyelids, lacrimal ducts extra encounter numerous problems; age will play a ocular muscles and conjunctiva. role, choice of a surgical protocol directly From the anatomical point of view, the fol related to the existing complaints, and coop lowing can be considered. eration between several surgical teams Position abnormalities (malpositions) of (ophthalmologic, plastic, cranio-maxillo-fac one or more elements and formation abnor ial and neurosurgical), the ideal being to treat malities (malformations) of the same organs. Some of these abnormalities are limited to Table I The manag ement of cong enital rna/positions one organ and can be subjected to a relatively of eyelid s, eyes and orbits simple and well recognised surgical treat Ocular Findings: ment.