Urinary Tract Infections & Asymptomatic Bacteriuria (Slides)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Incontinence
GLICKMAN UROLOGICAL & KIDNEY INSTITUTE Urinary Incontinence What is it? can lead to incontinence, as can prostate cancer surgery or Urinary incontinence is the inability to control when you radiation treatments. Sometimes the cause of incontinence pass urine. It’s a common medical problem. As many as isn’t clear. 20 million Americans suffer from loss of bladder control. The condition is more common as men get older, but it’s Where can I get help? not an inevitable part of aging. Often, embarrassment stops Talking to your doctor is the first step. You shouldn’t feel men from seeking help, even when the problem is severe ashamed; physicians regularly help patients with this prob- and affects their ability to leave the house, spend time with lem and are comfortable talking about it. Many patients family and friends or take part in everyday activities. It’s can be evaluated and treated after a simple office visit. possible to cure or significantly improve urinary inconti- Some patients may require additional diagnostic tests, nence, once its underlying cause has been identified. But which can be done in an outpatient setting and aren’t pain- it’s important to remember that incontinence is a symp- ful. Once these tests have determined the cause of your tom, not a disease. Its cause can be complex and involve incontinence, your doctor can recommend specific treat- many factors. Your doctor should do an in-depth evaluation ments, many of which do not require surgery. No matter before starting treatment. how serious the problem seems, urinary incontinence is a condition that can be significantly relieved and, in many What might be causing my incontinence? cases, cured. -

Point-Of-Care Ultrasound to Assess Anuria in Children
CME REVIEW ARTICLE Point-of-Care Ultrasound to Assess Anuria in Children Matthew D. Steimle, DO, Jennifer Plumb, MD, MPH, and Howard M. Corneli, MD patients to stay abreast of the most current advances in medicine Abstract: Anuria in children may arise from a host of causes and is a fre- and provide the safest, most efficient, state-of-the-art care. Point- quent concern in the emergency department. This review focuses on differ- of-care US can help us meet this goal.” entiating common causes of obstructive and nonobstructive anuria and the role of point-of-care ultrasound in this evaluation. We discuss some indications and basic techniques for bedside ultrasound imaging of the CLINICAL CONSIDERATIONS urinary system. In some cases, as for example with obvious dehydration or known renal failure, anuria is not mysterious, and evaluation can Key Words: point-of-care ultrasound, anuria, imaging, evaluation, be directed without imaging. In many other cases, however, diagnosis point-of-care US can be a simple and helpful way to assess urine (Pediatr Emer Care 2016;32: 544–548) volume, differentiate urinary retention in the bladder from other causes, evaluate other pathology, and, detect obstructive causes. TARGET AUDIENCE When should point-of-care US be performed? Because this imag- ing is low-risk, and rapid, early use is encouraged in any case This article is intended for health care providers who see chil- where it might be helpful. Scanning the bladder first answers the dren and adolescents in acute care settings. Pediatric emergency key question of whether urine is present. -

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

Overactive Bladder: What You Need to Know Whiteboard Animation Transcript with Shawna Johnston, MD and Emily Stern, MD
Obstetrics and Gynecology – Overactive Bladder: What You Need to Know Whiteboard Animation Transcript with Shawna Johnston, MD and Emily Stern, MD Overactive bladder (OAB) is a symptom-based disease state, which includes urinary frequency, nocturia, and urgency, with or without urgency incontinence. Symptoms of a urinary tract infection (UTI) are similar but additionally include dysuria (painful voiding) and hematuria. OAB tends to be a chronic progressive condition, while UTI symptoms are acute and may be associated with fever and malaise. In patients whose symptoms are unclear, urinalysis and urine culture may help rule out infection. If symptoms point to OAB, you should rule out: 1. Neurological disorders, such as multiple sclerosis, dementia, parkinson’s disease, and stroke. 2. Medical disorders such as diabetes, and 3. Prolapse, as women with obstructed voiding, usually from advanced prolapse, can have symptoms that mimic those of OAB. It is important to delineate how OAB symptoms affect a patient’s quality of life. Women with OAB are often socially isolated and sleep poorly. On history, pay attention to lifestyle factors such as caffeine and fluid intake, environmental triggers, and medications that may worsen symptoms like diuretics. Cognitive impairment and diabetes can influence OAB symptoms. Estrogen deficiency worsens OAB symptoms, so menopausal status and hormone use are important to note. Physical exam includes a screening sacral neurologic exam, an assessment for pelvic organ prolapse and a cough stress test to rule out stress urinary incontinence. On pelvic exam, look for signs of estrogen deficiency. Investigations include urinalysis, urine culture, and a post-void residual volume measurement. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -
Urinary System
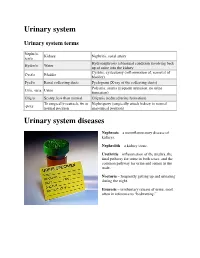
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Diagnosis and Management of Urinary Incontinence in Childhood
Committee 9 Diagnosis and Management of Urinary Incontinence in Childhood Chairman S. TEKGUL (Turkey) Members R. JM NIJMAN (The Netherlands), P. H OEBEKE (Belgium), D. CANNING (USA), W.BOWER (Hong-Kong), A. VON GONTARD (Germany) 701 CONTENTS E. NEUROGENIC DETRUSOR A. INTRODUCTION SPHINCTER DYSFUNCTION B. EVALUATION IN CHILDREN F. SURGICAL MANAGEMENT WHO WET C. NOCTURNAL ENURESIS G. PSYCHOLOGICAL ASPECTS OF URINARY INCONTINENCE AND ENURESIS IN CHILDREN D. DAY AND NIGHTTIME INCONTINENCE 702 Diagnosis and Management of Urinary Incontinence in Childhood S. TEKGUL, R. JM NIJMAN, P. HOEBEKE, D. CANNING, W.BOWER, A. VON GONTARD In newborns the bladder has been traditionally described as “uninhibited”, and it has been assumed A. INTRODUCTION that micturition occurs automatically by a simple spinal cord reflex, with little or no mediation by the higher neural centres. However, studies have indicated that In this chapter the diagnostic and treatment modalities even in full-term foetuses and newborns, micturition of urinary incontinence in childhood will be discussed. is modulated by higher centres and the previous notion In order to understand the pathophysiology of the that voiding is spontaneous and mediated by a simple most frequently encountered problems in children the spinal reflex is an oversimplification [3]. Foetal normal development of bladder and sphincter control micturition seems to be a behavioural state-dependent will be discussed. event: intrauterine micturition is not randomly distributed between sleep and arousal, but occurs The underlying pathophysiology will be outlined and almost exclusively while the foetus is awake [3]. the specific investigations for children will be discussed. For general information on epidemiology and During the last trimester the intra-uterine urine urodynamic investigations the respective chapters production is much higher than in the postnatal period are to be consulted. -

Gotta Gotta Go Right Now: a Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis
Gotta Go Right Now: A Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis Kelly Haack, M.A., and William J. Warzak, Ph.D. Department of Psychology, Munroe-Meyer Institute at the University of Nebraska Medical Center INTRODUCTION METHOD RESULTS Participant Bartter’s Syndrome Baseline 2 Months Following BRT ¾ Bartter’s Syndrome is caused by a defect in the kidney’s ¾ The participant was a 14-year-old male with Bartter’s Syndrome. Fluid Intake and Output Fluid Intake and Output ability to reabsorb potassium. ¾ He presented with frequent daytime and nighttime voiding. 1000 1000 ¾ As a result, the kidneys remove too much potassium from ¾ Medical History: 900 900 the body. 4 years old: Renal Ultrasound showed normal kidneys and 800 800 ¾ Excessive loss of potassium leads to muscle cramping and hypokalemia (low potassium level) was ruled out. Intake weakness, constipation, increased frequency of urination, 700 700 Intake and growth failure. 11 years old: Ditropan XL 10 mg daily and Imipramine 35 mg 600 600 daily were prescribed to treat symptoms of overactive bladder, Nocturnal Enuresis 500 500 ML such as frequent urination. ML ¾ Nocturnal Enuresis is involuntary passing of urine while 12 years old: Neurological exam was normal and neurogenic 400 400 asleep. bladder was ruled out. 300 300 Output Bartter’s Syndrome Output • Continued taking Ditropan and Imipramine. 200 200 and • Prescribed DDAVP 0.6 mg each evening to increase urine 100 100 concentration and decrease urine production. Nocturnal Enuresis 0 0 ¾ Adolescents with Bartter’s Syndrome often have a problem • Started use of a urine alarm; however, it was a short trial and 3:00 6:00 7:45 9:45 1:00 2:30 4:00 5:00 6:20 8:00 9:30 1:00 2:45 5:00 7:00 9:00 2:00 4:00 5:00 7:00 9:00 1:45 4:00 7:00 4:00 7:05 9:45 2:00 4:00 5:45 7:00 9:30 2:30 5:00 7:45 2:30 4:30 7:00 9:30 1:45 5:00 12:00 11:00 11:00 10:45 12:00 10:00 12:00 concentrating urine and excrete an excessive volume of he slept through it and continued to wet 5 out of 7 nights. -

Dysuria White Paper
CASE STUDY SUMMARY Management of Dysuria for BPH Surgical Procedures Ricardo Gonzalez, M.D. Medical Director of Voiding Dysfunction at Houston Metro Urology, Houston, Texas Dysuria following Benign Prostatic approach, concentrating on one area without Hyperplasia (BPH) Procedures ‘jumping around.’ Keep the laser at .5 mm away from the tissue when using the GreenLight PV® Transient dysuria following surgical treatment system; and 3 mm or less for the GreenLight of benign prostatic hyperplasia (BPH) is not an HPS® and GreenLight XPS® systems. Care must uncommon occurrence regardless of treatment. also be taken at the bladder neck: Identify Many factors may contribute to dysuria after the UOs and trigone, use lower power these procedures, including irritation from the (60-80 watts) and avoid directing energy introduction of the cystoscope; the degree of into the bladder.” tissue necrosis; the surgical modality utilized; the surgical technique employed; and the patient’s condition. This paper will focus on Pre-and Post-Operative Management both pre-procedural as well as post-procedural of Dysuria management of irritative symptoms related to Dr. Ricardo Gonzalez is an expert in the surgical BPH procedures. treatment of BPH with the GreenLight Laser System. “I spend considerable time Contributors to Dysuria educating patients on what to expect after Ricardo Gonzalez, M.D., Medical Director of surgical treatment of BPH, including dysuria,” Voiding Dysfunction at Houston Metro Urology says Dr. Gonzalez. “Proper patient education states, “Inefficient surgical technique can encour- will prevent many unnecessary phone calls age coagulative necrosis, which may increase from patients.” inflammation. This is more likely to be the case Dr. -
Urinary Tract Infections
Urinary Tract Infections www.kidney.org Did you know that... n Urinary tract infections (UTIs) are responsible for nearly 10 million doctor visits each year. n One in five women will have at least one UTI in her lifetime. Nearly 20 percent of women who have a UTI will have another, and 30 percent of those will have yet another. Of this last group, 80 percent will have recurrences. n About 80 to 90 percent of UTIs are caused by a single type of bacteria. 2 NATIONAL KIDNEY FOUNDATION n UTIs can be treated effectively with medications called antibiotics. n People who get repeated UTIs may need additional tests to check for other health problems. n UTIs also may be called cystitis or a bladder infection. This brochure answers the questions most often asked about UTIs. If you have more questions, speak to your doctor. What is a urinary tract infection? A urinary tract infection is what happens when bacteria (germs) get into the urinary tract (the bladder) and multiply. The result is redness, swelling and pain in the urinary tract (see diagram). WWW.KIDNEY.ORG 3 Most UTIs stay in the bladder, the pouch-shaped organ where urine is stored before it passes out of the body. If a UTI is not treated promptly, the bacteria can travel up to the kidneys and cause a more serious type of infection, called pyelonephritis (pronounced pie-low-nef-right- iss). Pyelonephritis is an actual infection of the kidney, where urine is produced. This may result in fever and back pain. What causes a UTI? About 80 to 90 percent of UTIs are caused by a type of bacteria, called E.