Intravenous Therapy Medications Or Therapeutic Solutions May Be
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intravenous Therapy Procedure Manual
INTRAVENOUS THERAPY PROCEDURE MANUAL - 1 - LETTER OF ACCEPTANCE __________________________________________ hereby approves (Facility) the attached Reference Manual as of _____________________. (Date) The Intravenous Therapy Procedure Manual will be reviewed at least annually or more often when deemed appropriate. Revisions will be reviewed as they occur. Current copies of the Intravenous Therapy Procedure Manual shall be maintained at each appropriate nursing station. I have reviewed this manual and agree to its approval. __________________________ (Administrator) __________________________ (Director of Nursing) __________________________ (Medical Director) - 2 - TABLE OF CONTENTS TABLE OF CONTENTS INTRODUCTION A. Purpose 1 B. Local Standard of Practice 1 RESPONSIBILITIES A. Responsibilities: M Chest Pharmacy 1 B. Responsibilities: Administrator 1 C. Responsibilities: Director of Nursing Services (DON/DNS) 1 D. Skills Validation 2 AMENDMENTS GUIDELINES A. Resident Candidacy for IV Therapy 1 B. Excluded IV Medications and Therapies 1 C. Processing the IV Order 1 D. IV Solutions/Medications: Storage 2 E. IV Solutions/Medications: Handling 3 F. IV Solutions and Supplies: Destroying and Returning 4 G. IV Tubing 5 H. Peripheral IV Catheters and Needles 6 I. Central Venous Devices 7 J. Documentation and Monitoring 8 K. IV Medication Administration Times 9 L. Emergency IV Supplies 10 I TABLE OF CONTENTS PROTOCOLS A. IV Antibiotic 1 1. Purpose 2. Guidelines 3. Nursing Responsibilities B. IV Push 2 1. Purpose 2. Guidelines C. Anaphylaxis Allergic Reaction 4 1. Purpose 2. Guidelines 3. Nursing Responsibilities and Interventions 4. Signs and Symptoms of Anaphylaxis 5. Drugs Used to Treat Anaphylaxis 6. Physician Protocol PRACTICE GUIDELINES A. Purpose 1 B. Personnel 1 C. Competencies 1 D. -

Injection Technique 1: Administering Drugs Via the Intramuscular Route
Copyright EMAP Publishing 2018 This article is not for distribution except for journal club use Clinical Practice Keywords Intramuscular injection/ Medicine administration/Absorption Practical procedures This article has been Injection technique double-blind peer reviewed Injection technique 1: administering drugs via the intramuscular route rugs administered by the intra- concerns that nurses are still performing Author Eileen Shepherd is clinical editor muscular (IM) route are depos- outdated and ritualistic practice relating to at Nursing Times. ited into vascular muscle site selection, aspirating back on the syringe Dtissue, which allows for rapid (Greenway, 2014) and skin cleansing. Abstract The intramuscular route allows absorption into the circulation (Dough- for rapid absorption of drugs into the erty and Lister, 2015; Ogston-Tuck, 2014). Site selection circulation. Using the correct injection Complications of poorly performed IM Four muscle sites are recommended for IM technique and selecting the correct site injection include: administration: will minimise the risk of complications. l Pain – strategies to reduce this are l Vastus lateris; outlined in Box 1; l Rectus femoris Citation Shepherd E (2018) Injection l Bleeding; l Deltoid; technique 1: administering drugs via l Abscess formation; l Ventrogluteal (Fig 1, Table 1). the intramuscular route. Nursing Times l Cellulitis; Traditionally the dorsogluteal (DG) [online]; 114: 8, 23-25. l Muscle fibrosis; muscle was used for IM injections but this l Injuries to nerves and blood vessels muscle is in close proximity to a major (Small, 2004); blood vessel and nerves, with sciatic nerve l Inadvertent intravenous (IV) access. injury a recognised complication (Small, These complications can be avoided if 2004). -

22428 Moxifloxacin Statisical PREA
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Science Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/Serial Number: 22,428 Drug Name: Moxifloxacin AF (moxifloxacin hydrochloride ophthalmic solution) 0.5% Indication(s): Treatment of bacterial conjunctivitis Applicant: Alcon Pharmaceuticals, Ltd. Date(s): Letter date:21 May 2010; Filing date: 18 June, 2010; PDUFA goal date: 19 November 2010 Review Priority: Priority Biometrics Division: Anti-infective and Ophthalmology Products Statistical Reviewer: Mark. A. Gamalo, Ph.D. Concurring Reviewers: Yan Wang, Ph.D. Medical Division: Anti-infective and Ophthalmology Products Clinical Reviewer: Lucious Lim, M.D. Project Manager: Lori Gorski Keywords: superiority, Moxifloxacin hydrochloride ophthalmic solution, bacterial conjunctivitis, bulbar conjunctival injection, conjunctival discharge/exudate TABLE OF CONTENTS TABLE OF CONTENTS................................................................................................................ 2 LIST OF TABLES.......................................................................................................................... 3 1. EXECUTIVE SUMMARY ...................................................................................................... 4 1. 1 Conclusions and Recommendations..................................................................................... 4 1. 2 Brief Overview of Clinical Studies ..................................................................................... -

Attachment 3
CURRICULUM CLINICAL BASE / CA-1 / CA-2 / CA-3 ANESTHESIOLOGY RESIDENCY PROGRAM GOALS AND OBJECTIVES AND CORE COMPETENCIES Department of Anesthesiology University of Missouri at Kansas City School of Medicine Saint Luke’s Hospital Truman Medical Center Children’s Mercy Hospital Revised 2011 Table of Contents Pages Introduction – Statement of Curriculum ................................................................................................................... 3 I. Rendering Patient Insensible to Pain ............................................................................................................. 4-10 II. Support of Life Functions ............................................................................................................................. 11-16 III. Clinical Base Year A. Cardiology ................................................................................................................................................. 17-32 B. Emergency Medicine ................................................................................................................................. 33-44 C. General Medicine ....................................................................................................................................... 45-49 D. Infectious Disease ...................................................................................................................................... 50-59 E. Nephrology .............................................................................................................................................. -

Nicotine Patches Appear Safe for CAD Patients
May 1, 2007 • www.internalmedicinenews.com Cardiovascular Medicine 37 Nicotine Patches Appear Safe for CAD Patients BY BRUCE JANCIN 30%, but many physicians have been re- induced myocardial defect on single-photon ment arm jumped from 10.9 to 25.2 Denver Bureau luctant to recommend it for their patients emission computed tomography (SPECT) ng/mL, Dr. Leja said. After 1 week, patients with coronary artery disease (CAD) be- to receive either 21-mg nicotine patches or were encouraged to quit smoking while N EW O RLEANS — Nicotine patches cause nicotine is known to increase heart placebo in addition to continuing their usu- continuing to use their assigned patches. are safe for use in smokers with known rate and blood pressure, and can induce al amount of cigarette smoking. The pri- Upon SPECT imaging at week 4, the coronary artery disease and stress-induced vasoconstriction as well, Dr. Monika J. Leja mary end point of the study was change in size of the perfusion defects in the nico- myocardial ischemia, according to the re- reported at the annual scientific session of total perfusion defect size upon repeat stress tine patch group remained unchanged sults of the first-ever randomized, place- the American College of Cardiology. SPECT imaging performed at 1 week. from baseline, although their plasma nico- bo-controlled, multicenter clinical trial to Dr. Leja and her coinvestigators at the There was no change in the total or is- tine levels remained as high as at week 1. examine this issue. Methodist DeBakey Heart Center in Hous- chemic perfusion defect size, compared The trial was supported by Glaxo- Nicotine replacement therapy doubles ton randomized 55 heavy smokers with with baseline, in either group even though SmithKline Consumer Healthcare. -
Informed Consent for Medication, Zyprexa
DEPARTMENT OF HEALTH SERVICES STATE OF WISCONSIN Division of Care and Treatment Services 42 CFR483.420(a)(2) F-24277 (09/2016) DHS 134.31(3)(o) DHS 94.03 & 94.09 §§ 51.61(1)(g) & (h) INFORMED CONSENT FOR MEDICATION Dosage and / or Side Effect information last revised on 04/16/2021 Completion of this form is voluntary. If not completed, the medication cannot be administered without a court order unless in an emergency. This consent is maintained in the client’s record and is accessible to authorized users. Name – Patient / Client (Last, First MI) ID Number Living Unit Date of Birth , Name – Individual Preparing This Form Name – Staff Contact Name / Telephone Number – Institution ANTICIPATED RECOMMENDED MEDICATION CATEGORY MEDICATION DOSAGE DAILY TOTAL DOSAGE RANGE RANGE Antipsychotic / Bipolar Agent Zyprexa oral tablet; Oral: 2.5 mg-50 mg with most doses in Zyprexa Zydis oral the 2.5 mg-20 mg range disintegrating tablet; IM: 5 mg-10 mg per dose, up to 3 doses Zyprexa Intramuscular 24 hours Injection; Long Acting Injectable: 150 mg-300 mg Zyprexa Relprevv IM every 2 weeks, Intramuscluar Injection 300 mg-405 mg IM every 4 weeks (olanzapine) The anticipated dosage range is to be individualized, may be above or below the recommended range but no medication will be administered without your informed and written consent. Recommended daily total dosage range of manufacturer, as stated in Physician’s Desk Reference (PDR) or another standard reference. This medication will be administered Orally Injection Other – Specify: 1. Reason for Use of Psychotropic Medication and Benefits Expected (note if this is ‘Off-Label’ Use) Include DSM-5 diagnosis or the diagnostic “working hypothesis.” 2. -

Product Monograph
PRODUCT MONOGRAPH Pr SANDOZ ONDANSETRON ODT Ondansetron Orally Disintegrating Tablets 4 mg and 8 mg ondansetron Manufacturer Standard Pr SANDOZ ONDANSETRON Ondansetron Tablets 4 mg and 8 mg ondansetron (as ondansetron hydrochloride dihydrate) Manufacturer Standard PrONDANSETRON INJECTION USP (ondansetron hydrochloride dihydrate) 2 mg/mL PrONDANSETRON HYDROCHLORIDE DIHYDRATE INJECTION Ondansetron Injection Manufacturer Standard 2 mg/mL Ondansetron (as ondansetron hydrochloride dihydrate) for injection Antiemetic (5-HT3-receptor antagonist) Sandoz Canada Inc. Date of Preparation: 145 Jules-Léger September 26, 2016 Boucherville, Québec, Canada J4B 7K8 Control No.: 198381 Ondansetron by Sandoz Page 1 of 43 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .......................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................. 3 INDICATIONS AND CLINICAL USE ....................................................................................... 4 CONTRAINDICATIONS ............................................................................................................ 4 WARNINGS AND PRECAUTIONS .......................................................................................... 5 ADVERSE REACTIONS ............................................................................................................ 7 DRUG INTERACTIONS ............................................................................................................ -
Intravenous Infusion Drug Administration: Flushing Guidance
Intravenous Infusion Drug Administration: Flushing Guidance April 2019 Acknowledgements: Andrew Barton – Author/reviewer NIVAS Chair Advanced Nurse Practitioner, IV Therapy and Vascular Access Frimley Health NHS Foundation Trust Tim Jackson – Reviewer/contributor, NIVAS Board Deputy Chair Consultant in Anesthesia & Intensive Care Medicine Calderdale & Huddersfield NHS Foundation Trust Gemma Oliver - Reviewer/contributor NIVAS Board Nurse Consultant, Integrated IV Care East Kent Hospitals NHS Foundation Trust Nicola York - Reviewer/contributor NIVAS Board Clinical Nurse Manager Vascular Access and Nutrition support Oxford University Hospitals NHS Foundation Trust Matt Jones - Reviewer/contributor NIVAS Board Consultant Anaesthetist East Kent Hospitals NHS Foundation Trust Steve Hill - Reviewer/contributor NIVAS Board Procedural Team Manger The Christie NHS Foundation Trust Marie Woodley - Reviewer/contributor NIVAS Board Clinical Nurse Specialist IV therapy/OPAT Lead Buckinghamshire Healthcare Trust Contents: Introduction………………………………………………………………………… Page 1 Methods of administering intravenous therapy………………………………… Page 2 Intravenous bolus injection…………………………………………….… Page 2 Continuous, variable dose syringe driver injection……………………. Page 2 Intravenous infusion…………………………………………………….… Page 3 Option 1: Discarding the infusion set………………………………….… Page 3 Option 2: Flushing the Infusion set manually…………………………... Page 4 Option 3: Flushing the infusion set with a closed system…………….. Page 4 General Guidance…………………………………………………………………. Page 5 Conclusion…………………………………………………………………………. -

Intravenous Therapytherapy
IntravenousIntravenous TherapyTherapy Department of EMS Professions Temple College IVIV TherapyTherapy OverviewOverview I DefinitionsDefinitions && IndicationsIndications I FluidFluid ResuscitationResuscitation I EquipmentEquipment andand SuppliesSupplies I ChoosingChoosing FluidsFluids andand CathetersCatheters I ProcedureProcedure andand TechniqueTechnique TipsTips – Peripheral Venipuncture – Intraosseous Access I PotentialPotential ComplicationsComplications DefinitionsDefinitions I IVIV // VenipunctureVenipuncture I CrystalloidsCrystalloids I PeripheralPeripheral // CentralCentral I ColloidsColloids I IntraosseousIntraosseous AccessAccess I HypertonicHypertonic I FluidFluid ResuscitationResuscitation I IsotonicIsotonic I MedicationMedication AccessAccess I DripDrip RatesRates I KVOKVO // TKOTKO IndicationsIndications forfor VenipunctureVenipuncture I VolumeVolume I VenousVenous AccessAccess toto – Dehydration CirculationCirculation I Water – Blood collection I Electrolytes I Labs – Blood Loss I Field Chemistry I Colloids – Medication I Crystalloids Administration FluidFluid ResuscitationResuscitation I DehydrationDehydration andand I ShockShock VolumeVolume LossLoss ManagementManagement – Replace Lost Fluid or – Controversial Blood – Definitive therapy = – Often requires 2 -3 Surgery and blood times the amount replacement lost (2:1 rule) – EMS → judicious replacement – Improve end organ perfusion (BP at 90 - 100 mm Hg) EquipmentEquipment andand SuppliesSupplies I FluidsFluids I SuppliesSupplies – Normal Saline – IV Catheters (0.9% -
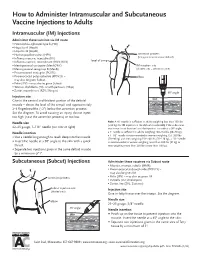
How to Administer Intramuscular and Subcutaneous Vaccines to Adults
How to Administer Intramuscular and Subcutaneous Vaccine Injections to Adults Intramuscular (IM) Injections Administer these vaccines via IM route • Haemophilus influenzae type b (Hib) • Hepatitis A (HepA) • Hepatitis B (HepB) • Human papillomavirus (HPV) acromion process (bony prominence above deltoid) • Influenza vaccine, injectable (IIV) • level of armpit • Influenza vaccine, recombinant (RIV3; RIV4) • Meningococcal conjugate (MenACWY) IM injection site • Meningococcal serogroup B (MenB) (shaded area = deltoid muscle) • Pneumococcal conjugate (PCV13) • Pneumococcal polysaccharide (PPSV23) – elbow may also be given Subcut • Polio (IPV) – may also be given Subcut • Tetanus, diphtheria (Td), or with pertussis (Tdap) • Zoster, recombinant (RZV; Shingrix) 90° angle Injection site skin Give in the central and thickest portion of the deltoid muscle – above the level of the armpit and approximately subcutaneous tissue 2–3 fingerbreadths (~2") below the acromion process. See the diagram. To avoid causing an injury, do not inject muscle too high (near the acromion process) or too low. Needle size Note: A ⅝" needle is sufficient in adults weighing less than 130 lbs (<60 kg) for IM injection in the deltoid muscle only if the subcutane- 22–25 gauge, 1–1½" needle (see note at right) ous tissue is not bunched and the injection is made at a 90° angle; Needle insertion a 1" needle is sufficient in adults weighing 130–152 lbs (60–70 kg); a 1–1½" needle is recommended in women weighing 153–200 lbs • Use a needle long enough to reach deep into the muscle. (70–90 kg) and men weighing 153–260 lbs (70–118 kg); a 1½" needle • Insert the needle at a 90° angle to the skin with a quick is recommended in women weighing more than 200 lbs (91 kg) or thrust. -

Intravenous Medicine Administration Self-Directed Learning Package
Acute Services Division Practice Development Department Intravenous Medicine Administration Self-directed Learning Package Margaret A. Connolly Katherine Hill Lynne Robertson Debbie Thompson Pinky Virhia First published August 2007 Revised July 2014 For review July 2016 Contribution by Christina Ronyane © Practice Development Department, NHS Greater Glasgow and Clyde 2014. All rights reserved. No part of this document may be reproduced, stored in a retrieval system or transmitted in any form or by any means electronic, mechanical, photocopying,recording or otherwise without the prior permission of Practice Development Department, NHS GG&C. Acknowledgement of sources of illustrations Figure 1 – page 7 Yellow Card Reproduced with the kind permission of the MHRA. Figure 2 – page 9 Peripheral venous access. Reproduced with the kind permission of Smith and Nephew. Figure 3 – page 10 Midline. Images provided by Vygon (UK) Ltd – © Vygon (UK) Ltd 2012. Figure 4 – page 10 Peripherally inserted central catheter. Provided by Vygon (UK) Ltd - © Vygon (UK) Ltd 2012. Figure 5 – page 10 Non Skin Tunnelled Central Line. Reproduced with the kind permission of Smith and Nephew. Figure 6 – page 11 Skin Tunnelled central venous access. Provided by Vygon (UK) Ltd - © Vygon (UK) Ltd 2012. Figure 7 – page 11 Indwelling Central Venous Access Device. Provided by Vygon (UK) Ltd - © Vygon (UK) Ltd 2012. Figure 10 – page 19 Anaphylaxis algorithm - Reproduced with the kind permission of the Resuscitation Council (UK). Contents Prerequisites for undertaking the IV -

Improvement of Biodistribution with Pegylated Liposomes Containing
ANTICANCER RESEARCH 31: 153-160 (2011) Improvement of Biodistribution with PEGylated Liposomes Containing Docetaxel with Degradable Starch Microspheres for Hepatic Arterial Infusion in the Treatment of Liver Metastases: A Study in CC-531 Liver Tumor-bearing WAG RIJ Rats U. POHLEN, H.J. BUHR and G. BERGER Department of Surgery, Charité Universitaetsmedizin Berlin, Benjamin Franklin Campus, Berlin, Germany Abstract. Aim: To improve the drug concentration in liver metastatic breast cancer develop liver metastases and have a metastases, docetaxel was encapsulated in polyethyleneglycol- poor prognosis, with a median survival of 1-2 years and a 5- liposomes and administered regionally with degradable starch year survival rate of approximately 20% (6, 7). microspheres (DSM). Materials and Methods: A rodent model The most frequently applied chemotherapeutic agent for of solitary metastasis (CC-531 adenocarcinoma) was studied. advanced breast cancer, ovarian cancer and gastric cancer is The animals were randomized into six groups and treated with docetaxel (8-10). 15 ng/kg docetaxel: I: intravenous (i.v.). II: PEG-liposomes Docetaxel inhibits cell proliferation by inducing a i.v.; III: intraartial (i.a.) via the hepatica artery; IV: i.a.) + sustained mitotic block at the metaphase/anaphase anticancer DSM; V: PEG-liposomes i.a.; and VI: PEG-liposomes i.a. + agents in this class promote the polymerization of stable DSM. The docetaxel concentration in the serum, liver and liver microtubules, inhibit their disassembly and profoundly affect tumor at defined times (5, 15, 30, 60,120 240 min and 24 h) a number of key cellular functions that depend on the was measured using HPLC.