Injecting with a Vial and Syringe | Lantus (Insulin Glargine Injection)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intravenous Therapy Procedure Manual
INTRAVENOUS THERAPY PROCEDURE MANUAL - 1 - LETTER OF ACCEPTANCE __________________________________________ hereby approves (Facility) the attached Reference Manual as of _____________________. (Date) The Intravenous Therapy Procedure Manual will be reviewed at least annually or more often when deemed appropriate. Revisions will be reviewed as they occur. Current copies of the Intravenous Therapy Procedure Manual shall be maintained at each appropriate nursing station. I have reviewed this manual and agree to its approval. __________________________ (Administrator) __________________________ (Director of Nursing) __________________________ (Medical Director) - 2 - TABLE OF CONTENTS TABLE OF CONTENTS INTRODUCTION A. Purpose 1 B. Local Standard of Practice 1 RESPONSIBILITIES A. Responsibilities: M Chest Pharmacy 1 B. Responsibilities: Administrator 1 C. Responsibilities: Director of Nursing Services (DON/DNS) 1 D. Skills Validation 2 AMENDMENTS GUIDELINES A. Resident Candidacy for IV Therapy 1 B. Excluded IV Medications and Therapies 1 C. Processing the IV Order 1 D. IV Solutions/Medications: Storage 2 E. IV Solutions/Medications: Handling 3 F. IV Solutions and Supplies: Destroying and Returning 4 G. IV Tubing 5 H. Peripheral IV Catheters and Needles 6 I. Central Venous Devices 7 J. Documentation and Monitoring 8 K. IV Medication Administration Times 9 L. Emergency IV Supplies 10 I TABLE OF CONTENTS PROTOCOLS A. IV Antibiotic 1 1. Purpose 2. Guidelines 3. Nursing Responsibilities B. IV Push 2 1. Purpose 2. Guidelines C. Anaphylaxis Allergic Reaction 4 1. Purpose 2. Guidelines 3. Nursing Responsibilities and Interventions 4. Signs and Symptoms of Anaphylaxis 5. Drugs Used to Treat Anaphylaxis 6. Physician Protocol PRACTICE GUIDELINES A. Purpose 1 B. Personnel 1 C. Competencies 1 D. -

Injection Technique 1: Administering Drugs Via the Intramuscular Route
Copyright EMAP Publishing 2018 This article is not for distribution except for journal club use Clinical Practice Keywords Intramuscular injection/ Medicine administration/Absorption Practical procedures This article has been Injection technique double-blind peer reviewed Injection technique 1: administering drugs via the intramuscular route rugs administered by the intra- concerns that nurses are still performing Author Eileen Shepherd is clinical editor muscular (IM) route are depos- outdated and ritualistic practice relating to at Nursing Times. ited into vascular muscle site selection, aspirating back on the syringe Dtissue, which allows for rapid (Greenway, 2014) and skin cleansing. Abstract The intramuscular route allows absorption into the circulation (Dough- for rapid absorption of drugs into the erty and Lister, 2015; Ogston-Tuck, 2014). Site selection circulation. Using the correct injection Complications of poorly performed IM Four muscle sites are recommended for IM technique and selecting the correct site injection include: administration: will minimise the risk of complications. l Pain – strategies to reduce this are l Vastus lateris; outlined in Box 1; l Rectus femoris Citation Shepherd E (2018) Injection l Bleeding; l Deltoid; technique 1: administering drugs via l Abscess formation; l Ventrogluteal (Fig 1, Table 1). the intramuscular route. Nursing Times l Cellulitis; Traditionally the dorsogluteal (DG) [online]; 114: 8, 23-25. l Muscle fibrosis; muscle was used for IM injections but this l Injuries to nerves and blood vessels muscle is in close proximity to a major (Small, 2004); blood vessel and nerves, with sciatic nerve l Inadvertent intravenous (IV) access. injury a recognised complication (Small, These complications can be avoided if 2004). -

22428 Moxifloxacin Statisical PREA
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Translational Science Office of Biostatistics S TATISTICAL R EVIEW AND E VALUATION CLINICAL STUDIES NDA/Serial Number: 22,428 Drug Name: Moxifloxacin AF (moxifloxacin hydrochloride ophthalmic solution) 0.5% Indication(s): Treatment of bacterial conjunctivitis Applicant: Alcon Pharmaceuticals, Ltd. Date(s): Letter date:21 May 2010; Filing date: 18 June, 2010; PDUFA goal date: 19 November 2010 Review Priority: Priority Biometrics Division: Anti-infective and Ophthalmology Products Statistical Reviewer: Mark. A. Gamalo, Ph.D. Concurring Reviewers: Yan Wang, Ph.D. Medical Division: Anti-infective and Ophthalmology Products Clinical Reviewer: Lucious Lim, M.D. Project Manager: Lori Gorski Keywords: superiority, Moxifloxacin hydrochloride ophthalmic solution, bacterial conjunctivitis, bulbar conjunctival injection, conjunctival discharge/exudate TABLE OF CONTENTS TABLE OF CONTENTS................................................................................................................ 2 LIST OF TABLES.......................................................................................................................... 3 1. EXECUTIVE SUMMARY ...................................................................................................... 4 1. 1 Conclusions and Recommendations..................................................................................... 4 1. 2 Brief Overview of Clinical Studies ..................................................................................... -
Informed Consent for Medication, Zyprexa
DEPARTMENT OF HEALTH SERVICES STATE OF WISCONSIN Division of Care and Treatment Services 42 CFR483.420(a)(2) F-24277 (09/2016) DHS 134.31(3)(o) DHS 94.03 & 94.09 §§ 51.61(1)(g) & (h) INFORMED CONSENT FOR MEDICATION Dosage and / or Side Effect information last revised on 04/16/2021 Completion of this form is voluntary. If not completed, the medication cannot be administered without a court order unless in an emergency. This consent is maintained in the client’s record and is accessible to authorized users. Name – Patient / Client (Last, First MI) ID Number Living Unit Date of Birth , Name – Individual Preparing This Form Name – Staff Contact Name / Telephone Number – Institution ANTICIPATED RECOMMENDED MEDICATION CATEGORY MEDICATION DOSAGE DAILY TOTAL DOSAGE RANGE RANGE Antipsychotic / Bipolar Agent Zyprexa oral tablet; Oral: 2.5 mg-50 mg with most doses in Zyprexa Zydis oral the 2.5 mg-20 mg range disintegrating tablet; IM: 5 mg-10 mg per dose, up to 3 doses Zyprexa Intramuscular 24 hours Injection; Long Acting Injectable: 150 mg-300 mg Zyprexa Relprevv IM every 2 weeks, Intramuscluar Injection 300 mg-405 mg IM every 4 weeks (olanzapine) The anticipated dosage range is to be individualized, may be above or below the recommended range but no medication will be administered without your informed and written consent. Recommended daily total dosage range of manufacturer, as stated in Physician’s Desk Reference (PDR) or another standard reference. This medication will be administered Orally Injection Other – Specify: 1. Reason for Use of Psychotropic Medication and Benefits Expected (note if this is ‘Off-Label’ Use) Include DSM-5 diagnosis or the diagnostic “working hypothesis.” 2. -

Product Monograph
PRODUCT MONOGRAPH Pr SANDOZ ONDANSETRON ODT Ondansetron Orally Disintegrating Tablets 4 mg and 8 mg ondansetron Manufacturer Standard Pr SANDOZ ONDANSETRON Ondansetron Tablets 4 mg and 8 mg ondansetron (as ondansetron hydrochloride dihydrate) Manufacturer Standard PrONDANSETRON INJECTION USP (ondansetron hydrochloride dihydrate) 2 mg/mL PrONDANSETRON HYDROCHLORIDE DIHYDRATE INJECTION Ondansetron Injection Manufacturer Standard 2 mg/mL Ondansetron (as ondansetron hydrochloride dihydrate) for injection Antiemetic (5-HT3-receptor antagonist) Sandoz Canada Inc. Date of Preparation: 145 Jules-Léger September 26, 2016 Boucherville, Québec, Canada J4B 7K8 Control No.: 198381 Ondansetron by Sandoz Page 1 of 43 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .......................................................... 3 SUMMARY PRODUCT INFORMATION ................................................................................. 3 INDICATIONS AND CLINICAL USE ....................................................................................... 4 CONTRAINDICATIONS ............................................................................................................ 4 WARNINGS AND PRECAUTIONS .......................................................................................... 5 ADVERSE REACTIONS ............................................................................................................ 7 DRUG INTERACTIONS ............................................................................................................ -
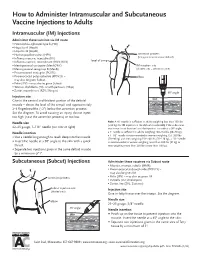
How to Administer Intramuscular and Subcutaneous Vaccines to Adults
How to Administer Intramuscular and Subcutaneous Vaccine Injections to Adults Intramuscular (IM) Injections Administer these vaccines via IM route • Haemophilus influenzae type b (Hib) • Hepatitis A (HepA) • Hepatitis B (HepB) • Human papillomavirus (HPV) acromion process (bony prominence above deltoid) • Influenza vaccine, injectable (IIV) • level of armpit • Influenza vaccine, recombinant (RIV3; RIV4) • Meningococcal conjugate (MenACWY) IM injection site • Meningococcal serogroup B (MenB) (shaded area = deltoid muscle) • Pneumococcal conjugate (PCV13) • Pneumococcal polysaccharide (PPSV23) – elbow may also be given Subcut • Polio (IPV) – may also be given Subcut • Tetanus, diphtheria (Td), or with pertussis (Tdap) • Zoster, recombinant (RZV; Shingrix) 90° angle Injection site skin Give in the central and thickest portion of the deltoid muscle – above the level of the armpit and approximately subcutaneous tissue 2–3 fingerbreadths (~2") below the acromion process. See the diagram. To avoid causing an injury, do not inject muscle too high (near the acromion process) or too low. Needle size Note: A ⅝" needle is sufficient in adults weighing less than 130 lbs (<60 kg) for IM injection in the deltoid muscle only if the subcutane- 22–25 gauge, 1–1½" needle (see note at right) ous tissue is not bunched and the injection is made at a 90° angle; Needle insertion a 1" needle is sufficient in adults weighing 130–152 lbs (60–70 kg); a 1–1½" needle is recommended in women weighing 153–200 lbs • Use a needle long enough to reach deep into the muscle. (70–90 kg) and men weighing 153–260 lbs (70–118 kg); a 1½" needle • Insert the needle at a 90° angle to the skin with a quick is recommended in women weighing more than 200 lbs (91 kg) or thrust. -
Intramuscular Injections: GUIDELINES for BEST PRACTICE B
2.1 ANCC Contact Hours Abstract The administration of injec- tions is a fundamental nursing skill; however, it is not without risk. Children receive numer- ous vaccines, and pediatric nurses administer the major- ity of these vaccines via the intramuscular route, and thus must be knowledgeable about safe and evidence-based immunization programs. Nurses may not be aware of the potential consequences associated with poor injection practices, and historically have relied on their basic nursing training or the advice of colleagues as a substitute for newer evidence about how to administer injections today. Evidence-based nursing practice requires pediatric nurses to review current literature to establish best practices and thus improved patient outcomes. Key words: Child; Evidence-based nursing; Injection intramuscu- lar; Vaccination. AbbyPediatric Rishovd, DNP, PNP Intramuscular Injections: GUIDELINES FOR BEST PRACTICE B. Boissonnet / BSIP SA / Alamy Alamy / B. Boissonnet / BSIP SA March/April 2014 MCN 107 Copyright © 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited. ver the past decade, the childhood vaccine (2011), and the World Health Organization (2004) have schedule has increased in complexity. De- now all strongly discouraged the practice of aspirating for pending upon the combinations adminis- blood when administering an IM injection. A randomized tered, children now may receive as many control trial found that the standard injection technique as 24 immunizations via intramuscular consisting of slow aspiration and injection followed by O(IM) injection by 2 years of age (Centers withdrawal of the needle was more painful and took lon- for Disease Control and Prevention [CDC], 2011). Pedi- ger than rapid injection without aspiration (Ipp, Taddio, atric nurses administer the majority of injections and thus Sam, Gladbach, & Parkin, 2007). -
A Guide to Aerosol Delivery Devices for Respiratory Therapists 4Th Edition
A Guide To Aerosol Delivery Devices for Respiratory Therapists 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC Platinum Sponsor Copyright ©2017 by the American Association for Respiratory Care A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC With a Foreword by Timothy R. Myers, MBA, RRT-NPS, FAARC Chief Business Officer American Association for Respiratory Care DISCLOSURE Douglas S. Gardenhire, EdD, RRT-NPS, FAARC has served as a consultant for the following companies: Westmed, Inc. and Boehringer Ingelheim. Produced by the American Association for Respiratory Care 2 A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition American Association for Respiratory Care, © 2017 Foreward Aerosol therapy is considered to be one of the corner- any) benefit from their prescribed metered-dose inhalers, stones of respiratory therapy that exemplifies the nuances dry-powder inhalers, and nebulizers simply because they are of both the art and science of 21st century medicine. As not adequately trained or evaluated on their proper use. respiratory therapists are the only health care providers The combination of the right medication and the most who receive extensive formal education and who are tested optimal delivery device with the patient’s cognitive and for competency in aerosol therapy, the ability to manage physical abilities is the critical juncture where science inter- patients with both acute and chronic respiratory disease as sects with art. -
Infusion/Injection Coding Education Injection/Infusion Hierarchy for Facility Reporting
INFUSION/INJECTION CODING EDUCATION INJECTION/INFUSION HIERARCHY FOR FACILITY REPORTING Chemotherapy Infusion Chemotherapy IV Push Chemotherapy Injection Therapeutic, Prophylactic, or Diagnostic Infusions Therapeutic, Prophylactic, or Diagnostic IV Push Therapeutic, Prophylactic, or Diagnostic Injections Hydration 2 INFUSION/INJECTION DECISION TREE How long did it take? How was it given? What did the patient receive? Why is the patient here? 3 TIME DOCUMENTATION IS CRITICAL • Time Documentation is Critical • Drug administration codes are services that reference time and are “time- based” codes • Documentation should support the services reported • Therapeutic Infusions Hydration • 1st Hour 16-90 minutes 31-90 minutes • 2nd Hour 91-150 minutes 91-150 minutes • 3rd Hour 151-210 minutes 151-210 minutes • Best Practice – document “start” and “stop” times for infusions • Noridian Drugs, Biologicals, and Injections Documentation Requirements indicate: • Medication Administration Record (MAR) from date(s) of service that include name of medications(s), dose, route of administration and infusion start and stop times, if applicable 4 INITIAL SERVICE • “Initial” service is described as “the service that best describes the key or primary reason for the encounter” • Order of service delivery does not determine what is “initial” service • Hierarchy does not apply to Subcutaneous/Intramuscular injections • Only one per patient encounter UNLESS: • Two separate IV sites are medically used/necessary • Patient returns for a separate and medically necessary and reasonable encounter on the same day • These may be reported with two initial services with a modifier -59 (XE) on the second IV or second encounter 5 INITIAL SERVICE • IV Push with Hydration – What is the “initial” service? • When you bill IV hydration along with IV pushes, always report the IV push as the initial code. -

Injection Guide Overview and Goals of This Guide ����������������������������������� 1
Injection Guide Overview and goals of this guide . 1 Overview of injections. 3 Why did my doctor choose an injectable medication? ��������������� 3 Differences between injectable medication and oral medication . 3 Types of injections. 4 Parts of a syringe ��������������������������������������������������� 4 Steps for injecting medication ��������������������������������������� 5 Storage ������������������������������������������������������������� 5 Preparation ��������������������������������������������������������� 6 Wash your hands ����������������������������������������������� 6 Prepare your medication for injection ��������������������������� 7 Prepare the injection site ��������������������������������������� 8 Injection ����������������������������������������������������������� 9 Intramuscular injection ����������������������������������������� 9 Subcutaneous injection ����������������������������������������10 Disposal. .11 Monitoring of the injection site ����������������������������� 12 References . .13 Injection-site records ������������������������������������������������14 Overview and goals of this guide This guide is a quick reference on how to use medications that are given by injection. It gives step-by-step instructions for preparing and injecting the medication. It also covers safety precautions. The instructions in this guide apply whether you are giving the injection to someone you care for or you are giving the injection to yourself. This guide is not meant to replace instructions from your doctor nor the information -

Intravenous Infusions And/Or Injections
TUE Physician Guidelines Medical Information to Support the Decisions of TUECs INTRAVENOUS INFUSIONS Intravenous Infusions and/or Injections 1. Introduction Intravenous (IV) infusions have been included on the WADA List of Prohibited Substances and Methods under section M2. Prohibited Methods; Chemical and Physical Manipulation since 20051. An IV infusion or injection is the supply of fluid and/or prescribed medication by drip or push directly into a vein. Intravenous infusions are prohibited both in-competition and out-of-competition if the volume delivered exceeds 100 ml within a 12-hour period. The wording in the 2018 Prohibited List states that the following is prohibited: Intravenous infusions and/or injections of more than a total of 100 ml per 12-hour period except for those legitimately received in the course of hospital treatments, surgical procedures or clinical diagnostic investigations1. The wording in the Prohibited List for IV infusions is unique in that the method is not prohibited under the three exceptions stated above. However, a TUE may be necessary for a Prohibited Substance delivered by intravenous infusion even if the infusion itself is delivered in the setting of one of the three exceptions. IV infusions are included on the Prohibited List mainly because some athletes could use this Prohibited Method to: a) enhance their performance by increasing plasma volume levels; b) mask the use of a Prohibited Substance; c) distort the values of their Athlete Biological Passport. Infusions or injections of 100 ml or less within a 12-hour period are permitted unless the infused/injected substance is on the Prohibited List. -

ISMP Safe Practice Guidelines for Adult IV Push Medications
ISMP Safe Practice Guidelines for Adult IV Push Medications A compilation of safe practices from the ISMP Adult IV Push Medication Safety Summit Prepared by the Institute for Safe Medication Practices (ISMP) Table of Contents Introduction 1 Factors that Increase the Risk of IV Push Medication Errors in Adults 2 Risks Associated with Lack of Patient Information 3 Risks Associated with Lack of Drug Information 3 Risks Associated with Communication of Drug Information 3 Risks Associated with Drug Labeling, Packaging, and Nomenclature 3 Risks Associated with Drug Storage, Stock, Standardization, and Distribution 4 Risks Associated with Device Use 4 Risks Associated with Environment, Staffing, and Workflow 4 Risks Associated with Staff Education and Competency 4 Risk Management and Quality Improvement Challenges 5 Current Practices with IV Injectable Medications 6 Developing Consensus Guidelines for Adult IV Push Medications 7 Safe Practice Guidelines 8 1. Acquisition and Distribution of Adult IV Push Medications 8 2. Aseptic Technique 9 3. Clinician Preparation 10 4. Labeling 12 5. Clinician Administration 13 6. Drug Information Resources 14 7. Competency Assessment 15 8. Error Reporting 15 Future Inquiry 16 Conclusion 16 References 17 Definitions 19 ISMP Adult IV Push Medication Safety Summit Participants 20 Appendix A — ISMP Safe Practice Guidelines for Adult IV Push Medications 22 Disclosure 24 About ISMP 24 ISMP SAFE PRACTICE GUIDELINES FOR ADULT IV PUSH MEDICATIONS © ISMP 2015 Introduction Intravenous (IV) therapy is considered an essential component of current healthcare delivery, with over 90% of hospitalized patients receiving some form of infusion therapy. 1-2 Errors involving IV medications can occur in all phases of the medication use process and can be particularly dangerous based on the drug’s properties and the complexity of its therapeutic action.