Impacts of Reused/ Reclaimed Water: Organisms and Chemicals of Concern Research and Development Office Science and Technology Program Final Report ST-2015-9782-01
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Reuse: a Safe and Effective Way to Save Water
SOUTH FLORIDA WATER MANAGEMENT DISTRICT Water Reuse: A safe and effective way to save water ON THE INSIDE The demand for water is projected to increase over the long term in n Reclaimed water and reuse explained South Florida. Urban populations, agricultural operations and the environment depend on adequate water supplies. Fresh ground n Reuse success stories water and surface water will not be sufficient to satisfy all future n Reuse on a regional level demands. Meeting this growing thirst hinges on efforts to develop How water is reclaimed n alternative water sources. This brochure looks at one of the ways to n Purple pipes signify conserve Florida’s water resources — reclaiming water for reuse. reclaimed water Consider what happens to the water used inside the home. Once down the drain, this water is piped to the local wastewater treatment plant where it undergoes treatment to meet state standards for disposal. Historically, most of the water was disposed by injecting it deep underground or by discharging to surrounding waters or to the ocean. This is a wasteful way to treat such a valuable resource. More and more communities are finding that wastewater need not be wasted. They are reclaiming this water for irrigation of residential lots, golf courses, sports fields and orange groves; industrial cooling; car washing; fire protection; and Reclaimed water sign in Collier County groundwater recharge. Reuse is also beneficial to the environment. Success Stories During times of drought, reclaimed water •Pompano Beach – The city takes is a dependable source of water because wastewater being piped to the ocean, its availability is not dependent on rainfall. -
Use of a Water Treatment Sludge in a Sewage Sludge Dewatering Process
E3S Web of Conferences 30, 02006 (2018) https://doi.org/10.1051/e3sconf/20183002006 Water, Wastewater and Energy in Smart Cities Use of a water treatment sludge in a sewage sludge dewatering process Justyna Górka1,*, Małgorzata Cimochowicz-Rybicka1 , and Małgorzata Kryłów1 1 University of Technology, Department of Environmental Engineering, 24 Warszawska, Cracow 31- 155, Poland Abstract. The objective of the research study was to determine whether a sewage sludge conditioning had any impact on sludge dewaterability. As a conditioning agent a water treatment sludge was used, which was mixed with a sewage sludge before a digestion process. The capillary suction time (CST) and the specific filtration resistance (SRF) were the measures used to determine the effects of a water sludge addition on a dewatering process. Based on the CST curves the water sludge dose of 0.3 g total volatile solids (TVS) per 1.0 g TVS of a sewage sludge was selected. Once the water treatment sludge dose was accepted, disintegration of the water treatment sludge was performed and its dewaterability was determined. The studies have shown that sludge dewaterability was much better after its conditioning with a water sludge as well as after disintegration and conditioning, if comparing to sludge with no conditioning. Nevertheless, these findings are of preliminary nature and future studies will be needed to investigate this topic. 1 Introduction Dewatering of sludge is a very important stage of the sludge processing. It reduces both sludge mass and volume, which consequently reduces costs of a further sludge processing, facilitates its transport and allows for its thermal processing. -

A Novel Waste Water Treatment Plant for the Disposal of Organic Waste from Mobile Toilets
A Novel Waste Water Treatment Plant for The Disposal of Organic Waste from Mobile Toilets A Novel Waste Water Treatment Plant for The Disposal of Organic Waste from Mobile Toilets G. BONIFAZI, R. GASBARRONE, R. PALMIERI, G. CAPOBIANCO, S. SERRANTI Departments of Medical Sciences and Biotechnologies and of Chemical Eng. Materials, Environment- Sapienza University of Rome, Abstract The EU wastewater management industry is continuously looking for innovative technological solutions that can enter the market with a reduced environmental impact. This paper focuses on the problems associated to the disposal of human waste and on the specific market of the so-called mobile toilets. These are independent portable units equipped with sanitary tools that use chemical agents to disinfect the vessel and not connected to the sewer network. With growing awareness towards effective sanitation, mobile toilets have gained immense popularity in recent years and are now widely used at construction sites, event venues, public places, and in several other application like temporary refugee housing, migrants’ camps, military missions, cases of natural disasters, airplanes, trains, campers, caravans and campsites. This paper illustrates a new process for the disposal of organic waste from mobile toilets. Keywords: Waste Water Treatment Plants, Chemical Portable Toilets, Use of sludges in agriculture. 1. Introduction into surface and ground water and to avoid toxic effects on soil, plants, animals and humans. In The use of sludge in agriculture within the EU is most cases, national authorities have currently regulated only by the limits of heavy implemented policies supporting the use of metals (Cd, Cu, Hg, Ni, Pb and Zn) listed in sludge in agriculture, as it is considered to be the Council Directive 86/278/EEC. -

The Role of Water Reclamation in Water Resources Management in the 21St Century
THE ROLE OF WATER RECLAMATION IN WATER RESOURCES MANAGEMENT IN THE 21ST CENTURY K. Esposito1*, R. Tsuchihashi2, J. Anderson1, J. Selstrom3 1*: Metcalf & Eddy, 60 East 42nd Street, 43rd Floor, New York, NY 10165 2: Metcalf & Eddy, 719 2nd Street, Suite 11, Davis, CA 95616 3: Metcalf & Eddy, 2751 Prosperity Ave Suite 200, Fairfax, VA 22031 ABSTRACT In recognition of the existing and impending stress to traditional water supply, water planners must look beyond structural developments and interbasin water transfers to secure supply into the future. In this process, it is becoming evident that various issues related to water must be integrated into a whole system approach, including water supply, water use, wastewater treatment, stormwater management, and management of surrounding water environment. In bringing disparate water assets together, alternatives to traditional water supply should arise. Integrated water resources management can provide a realistic framework for examining the feasibility of water reuse. This paper evaluates how water reuse can become a strategic alternative in water resources management. The key challenges that limit water reclamation as one of the key elements in integrated water resources management scheme are discussed, including limitations with typical centralized wastewater treatment systems and public health protection, particularly the implications of trace contaminants. The key considerations to address these challenges are presented including (1) selection of appropriate treatment processes and reuse applications, (2) scientific and engineering solutions to emerging concerns, (3) consideration for cost effective and sustainable system, and (4) public acceptance. Recent water reclamation projects are presented to illustrate the response of the engineering community to the challenges of making water reclamation and reuse a real and sustainable solution to water supply system management planning. -

2.2 Sewage Sludge Incineration
2.2 Sewage Sludge Incineration There are approximately 170 sewage sludge incineration (SSI) plants in operation in the United States. Three main types of incinerators are used: multiple hearth, fluidized bed, and electric infrared. Some sludge is co-fired with municipal solid waste in combustors based on refuse combustion technology (see Section 2.1). Refuse co-fired with sludge in combustors based on sludge incinerating technology is limited to multiple hearth incinerators only. Over 80 percent of the identified operating sludge incinerators are of the multiple hearth design. About 15 percent are fluidized bed combustors and 3 percent are electric. The remaining combustors co-fire refuse with sludge. Most sludge incinerators are located in the Eastern United States, though there are a significant number on the West Coast. New York has the largest number of facilities with 33. Pennsylvania and Michigan have the next-largest numbers of facilities with 21 and 19 sites, respectively. Sewage sludge incinerator emissions are currently regulated under 40 CFR Part 60, Subpart O and 40 CFR Part 61, Subparts C and E. Subpart O in Part 60 establishes a New Source Performance Standard for particulate matter. Subparts C and E of Part 61--National Emission Standards for Hazardous Air Pollutants (NESHAP)--establish emission limits for beryllium and mercury, respectively. In 1989, technical standards for the use and disposal of sewage sludge were proposed as 40 CFR Part 503, under authority of Section 405 of the Clean Water Act. Subpart G of this proposed Part 503 proposes to establish national emission limits for arsenic, beryllium, cadmium, chromium, lead, mercury, nickel, and total hydrocarbons from sewage sludge incinerators. -

Energy Recovery from Sewage Sludge: the Case Study of Croatia
energies Article Energy Recovery from Sewage Sludge: The Case Study of Croatia Dinko Đurđevi´c 1,* , Paolo Blecich 2 and Željko Juri´c 1 1 Energy Institute Hrvoje Požar, 10000 Zagreb, Croatia; [email protected] 2 Faculty of Engineering, University of Rijeka, 51000 Rijeka, Croatia; [email protected] * Correspondence: [email protected] Received: 26 April 2019; Accepted: 16 May 2019; Published: 20 May 2019 Abstract: Croatia produced 21,366 tonnes of dry matter (DM) sewage sludge (SS) in 2016, a quantity expected to surpass 100,000 tonnes DM by 2024. Annual production rates for future wastewater treatment plants (WWTP) in Croatia are estimated at 5.8–7.3 Nm3/people equivalent (PE) for biogas and 20–25 kgDM/PE of sewage sludge. Biogas can be converted into 12–16 kWhel/PE of electricity and 19–24 kWhth/PE of heat, which is sufficient for 30–40% of electrical and 80–100% of thermal autonomy. The WWTP autonomy can be increased using energy recovery from sewage sludge incineration by 60% for electricity and 100% of thermal energy (10–13 kWhel/PE and 30–38 kWhth/PE). However, energy for sewage sludge drying exceeds energy recovery, unless solar drying is performed. 2 The annual solar drying potential is estimated between 450–750 kgDM/m of solar drying surface. The lower heating value of dried sewage sludge is 2–3 kWh/kgDM and this energy can be used for assisting sludge drying or for energy generation and supply to WWTPs. Sewage sludge can be considered a renewable energy source and its incineration generates substantially lower greenhouse gases emissions than energy generation from fossil fuels. -

Mobility of Heavy Metals in Municipal Sewage Sludge from Different Throughput Sewage Treatment Plants
Pol. J. Environ. Stud. Vol. 21, No. 6 (2012), 1603-1611 Original Research Mobility of Heavy Metals in Municipal Sewage Sludge from Different Throughput Sewage Treatment Plants Jarosław Gawdzik1*, Barbara Gawdzik2** 1Faculty of Civil and Environmental Engineering, Kielce University of Technology, Division of Waste Management, Al. 1000-lecia Państwa Polskiego 7, 25-314 Kielce, Poland 2Institute of Chemistry, Faculty of Mathematics and Science, Jan Kochanowski University of Humanities and Sciences, Świętokrzyska 15, 25-406 Kielce, Poland Received: 27 June 2011 Accepted: 11 May 2012 Abstract Sewage sludge heavy metals can be dissolved, precipitated, co-precipitated with metal oxides, and adsorbed or associated on the particles in biological debris. Heavy metals are found in the form of oxides, hydroxides, sulphides, sulphates, phosphates, silicates, organic bindings forming complexes with humic com- pounds, and complex sugars. Polish regulations specifying the maximum levels of heavy metals in municipal sewage sludge used for agricultural purposes refer to the total content of lead, cadmium, mercury, nickel, zinc, copper, and chromium. The aim of our study was to evaluate the mobility of heavy metals in sewage sludge from wastewater treatment plants in Świętokrzyskie Province. Stabilized sewage sludge from wastewater treatment was ana- lyzed in accordance with the extraction method proposed by the Community Bureau of Reference (BCR). Zinc, cadmium, lead, and nickel were determined by means of the standard addition with the use of a Perkin-Elmer 3100-BG FAAS atomic absorption spectrophotometer. Chromium and copper were tested using the FAAS technique. The sequence analysis revealed the presence of heavy metals in all fractions (F-I, F-II, F-III, F-IV). -

Circular Economy in Wastewater Treatment Plant– Challenges and Barriers †
Proceedings Circular Economy in Wastewater Treatment Plant– Challenges and Barriers † Ewa Neczaj * and Anna Grosser Faculty of Infrastructure and Environment, Czestochowa University of Technology, 42-201 Czestochowa, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-343-250-917 † Presented at the 3rd EWaS International Conference on “Insights on the Water-Energy-Food Nexus”, Lefkada Island, Greece, 27–30 June 2018. Published: 31 July 2018 Abstract: The urban wastewater treatment plants can be an important part of circular sustainability due to integration of energy production and resource recovery during clean water production. Currently the main drivers for developing wastewater industry are global nutrient needs and water and energy recovery from wastewater. The article presents current trends in wastewater treatment plants development based on Circular Economy assumptions, challenges and barriers which prevent the implementation of the CE and Smart Cities concept with WWTPs as an important player. WWTPs in the near future are to become “ecologically sustainable” technological systems and a very important nexus in SMART cities. Keywords: circular economy; wastewater treatment plant; resource recovery 1. Introduction The circular economy (CE) is the concept in which products, materials (and raw materials) should remain in the economy for as long as possible, and waste should be treated as secondary raw materials that can be recycled to process and re-use [1]. This distinguishes it from a linear economy based on the, ‘take-make-use-dispose’ system, in which waste is usually the last stage of the product life cycle. CE is a concept promotes sustainable management of materials and energy by minimalizing the amount of waste generation and their reuse as a secondary material. -

Sustainable Action Plan for County Operations 4890-012418 RTP-HT Table of Contents
REPORT CARD: FY 2016/2017 Sustainable Action Plan for County Operations 4890-012418 RTP-HT Table of contents Table of contents . 3 . Report card: FY 2016/2017 . 4 . How to use this report . 4 Progress summary . 5. Chapter 1 Chapter 4 Chapter 7 Minimizing the Carbon Footprint Alternative Fuel Waste of County Operations 6 Vehicles 12 Reduction 18 Noteworthy accomplishments . 6 Noteworthy accomplishments . 12 Noteworthy accomplishments . 18 Benefits & Performance . 7 Benefits & Performance . 13 Benefits & Performance . 19 Chapter 2 Chapter 5 Chapter 8 Renewable Energy & Energy Water Conservation Green Efficiency 8 & Management 14 Purchasing 20 Noteworthy accomplishments . 8 Noteworthy accomplishments . 14 Noteworthy accomplishments . 20 Benefits & Performance . 9 Benefits & Performance . 15 Benefits & Performance . 21 Chapter 3 Chapter 6 Chapter 9 Green Land Conservation Health & Building 10 & Management 16 Wellness 22 Noteworthy accomplishments . 10 Noteworthy accomplishments . 16 Noteworthy accomplishments . 22 Benefits & Performance . 11 Benefits & Performance . 17 Benefits & Performance . 23 Glossary . 24 References . 26 . Sustainable Action Plan for County Operations • Report Card: FY 2016/2017 | 3 REPORT CARD: FY 2016/2017 Sustainable Action Plan for County Operations n May 17, 2014, the Pima County Board of Supervisors adopted the 2014 Sustainable O Action Plan for County Operations . This plan seeks to achieve a “balance between economic development, social well-being and environmental protection to ensure the needs of current generations can be met without compromising the ability of future generations to meet their own needs .” Measuring progress is crucial to the success of Pima County’s sustainability efforts . The purpose of this report card is to inform County decision makers and the broader community about Pima Construction workers restore and preserve the Pima County’s progress toward meeting the goals and County Historic Courthouse . -
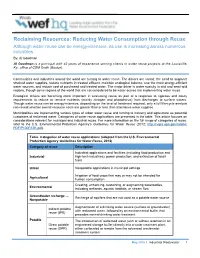
Reclaiming Resources: Reducing Water Consumption Through Reuse
Reclaiming Resources: Reducing Water Consumption through Reuse Although water reuse can be energy-intensive, its use is increasing across numerous industries By: Al Goodman Al Goodman is a principal with 42 years of experience serving clients in water reuse projects at the Louisville, Ky., office of CDM Smith (Boston). Communities and industries around the world are turning to water reuse. The drivers are varied: the need to augment strained water supplies, reduce nutrients in treated effluent, maintain ecological balance, use the most energy-efficient water sources, and reduce cost of purchased and treated water. The major driver is water scarcity in arid and semi-arid regions, though some regions of the world that are not considered to be water-scarce are implementing water reuse. Ecological drivers are becoming more important in evaluating reuse as part of a response to rigorous and costly requirements to reduce or remove nutrients (mainly nitrogen and phosphorus) from discharges to surface waters. Though water reuse can be energy-intensive, depending on the level of treatment required, only a full life-cycle analysis can reveal whether overall resource costs are greater than or less than alternative water supplies. Municipalities are implementing various types of urban water reuse and turning to industry and agriculture as potential customers of reclaimed water. Categories of water reuse applications are presented in the table. This article focuses on considerations relevant for municipal and industrial reuse. For more information on the full range of categories of reuse, refer to the U.S. Environmental Protection Agency’s Guidelines for Water Reuse (2012; http://nepis.epa.gov/Adobe/ PDF/P100FS7K.pdf). -

Quantifying the Potential of Renewable Natural Gas to Support a Reformed Energy Landscape: Estimates for New York State
energies Review Quantifying the Potential of Renewable Natural Gas to Support a Reformed Energy Landscape: Estimates for New York State Stephanie Taboada 1,2, Lori Clark 2,3, Jake Lindberg 1,2, David J. Tonjes 2,3,4 and Devinder Mahajan 1,2,* 1 Department of Materials Science and Chemical Engineering, Stony Brook University, Stony Brook, NY 11794, USA; [email protected] (S.T.); [email protected] (J.L.) 2 Institute of Gas Innovation and Technology, Advanced Energy Research and Technology, Stony Brook, NY 11794, USA; [email protected] (L.C.); [email protected] (D.J.T.) 3 Department of Technology and Society, Stony Brook University, 100 Nicolls Rd, Stony Brook, NY 11794, USA 4 Waste Data and Analysis Center, Stony Brook University, 100 Nicolls Rd, Stony Brook, NY 11794, USA * Correspondence: [email protected] Abstract: Public attention to climate change challenges our locked-in fossil fuel-dependent energy sector. Natural gas is replacing other fossil fuels in our energy mix. One way to reduce the greenhouse gas (GHG) impact of fossil natural gas is to replace it with renewable natural gas (RNG). The benefits of utilizing RNG are that it has no climate change impact when combusted and utilized in the same applications as fossil natural gas. RNG can be injected into the gas grid, used as a transportation fuel, or used for heating and electricity generation. Less common applications include utilizing RNG to produce chemicals, such as methanol, dimethyl ether, and ammonia. The GHG impact should be quantified before committing to RNG. This study quantifies the potential production of biogas (i.e., Citation: Taboada, S.; Clark, L.; the precursor to RNG) and RNG from agricultural and waste sources in New York State (NYS). -

Water Reclamation for Direct Re-Use in Urban and Industrial Applications in South Africa and Its Projected Impact Upon Water Demand
Water Reclamation for Direct Re-Use in Urban and Industrial Applications in South Africa and its Projected Impact Upon Water Demand A Grobicki • B Cohen Report to the Water Research Commission by Abbott Grobicki (Pty) Ltd r WRC Report No KV118/99 -^r -^r -^r *^^ Disclaimer This report emanates from a project financed by ihe Waler Research Commission (WRC) and is approved for publication. Approval docs not signify that the contents necessarily reflect the views and policies of the WRC or the members of the project steering committee, nor does mention of trade names or commercial products constitute endorsement or recommendation tor use. Vrywaring Hierdie verslag spruit voort uit 'n navorsingsprojek wat deur die Waternavorsingskommissic (WNK) gefinansier is en goedgekeur is vir publikasie. Goedkeuring beteken nie noodwendig dat die inhoud die sicning en beleid van die WNK of die lede van die projek-loodskomitee weerspieel nie, of dat melding van handelsname of -ware deur die WNK vir gebruik goedgekeur n( aanbeveel word nie. WATER RECLAMATION FOR DIRECT RE-USE IN URBAN AND INDUSTRIAL APPLICATIONS IN SOUTH AFRICA, AND ITS PROJECTED IMPACT UPON WATER DEMAND A STUDY FOR THE WATER RESEARCH COMMISSION BY DR ANIA GROBICKI AND DR BRETT COHEN Abbott Grobicki (Pty) Ltd Kimberley House 34 Shortmarket Street 8001 Cape Town Tel: (021) 424-3892, Fax: (021) 424-3895 email: [email protected] OCTOBER 1998 ii EXECUTIVE SUMMARY Water reclamation, or the direct use of treated sewage effluent to replace a proportion of the fresh water demand, is regarded as a non-conventional approach to water management. However, water reclamation is becoming increasingly common internationally, especially in countries which have water shortages similar to that in South Africa.