Plasmodium Prevalence and Artemisinin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A History of the Anlong Veng Community a History Of
A HIstoRy Of Anlong Veng CommunIty A wedding in Anlong Veng in the early 1990s. (Cover photo) Aer Vietnamese forces entered Cambodia in 1979, many Khmer Rouge forces scaered to the jungles, mountains, and border areas. Mountain 1003 was a prominent Khmer Rouge military base located within the Dangrek Mountains along the Cambodian-Thai border, not far from Anlong Veng. From this military base, the Khmer Rouge re-organized and prepared for the long struggle against Vietnamese and the People’s Republic of Kampuchea government forces. Eventually, it was from this base, Khmer Rouge forces would re-conquer and sele Anlong Veng in early 1990 (and a number of other locations) until their re-integration into Cambodian society in late 1998. In many ways, life in Anlong Veng was as difficult and dangerous as it was in Mountain 1003. As one of the KR strongholds, Anlong Veng served as one of the key launching points for Khmer Rouge guerrilla operations in Cambodia, and it was subject to constant aacks by Cambodian government forces. Despite the perilous circumstances and harsh environment, the people who lived in Anlong Veng endeavored, whenever possible, to re-connect with and maintain their rich cultural heritage. Tossed from the seat of power in 1979, the Khmer Rouge were unable to sustain their rigid ideo- logical policies, particularly as it related to community and family life. During the Democratic Movement of the Khmer Rouge Final Stronghold Kampuchea regime, 1975–79, the Khmer Rouge prohibited the traditional Cambodian wedding ceremony. Weddings were arranged by Khmer Rouge leaders and cadre, who oen required mass ceremonies, with lile regard for tradition or individual distinction. -
Evaluation Report on ECHO Funded Humanitarian Mine Action Pilot Projects in North-West of Cambodia
James Madison University JMU Scholarly Commons Center for International Stabilization and Global CWD Repository Recovery Fall 10-2003 Evaluation Report on ECHO Funded Humanitarian Mine Action Pilot Projects in North-West of Cambodia Marcel Durocher Agim Hoti Mok Tonh Keo Vut Follow this and additional works at: https://commons.lib.jmu.edu/cisr-globalcwd Part of the Defense and Security Studies Commons, Peace and Conflict Studies Commons, Public Policy Commons, and the Social Policy Commons Recommended Citation Durocher, Marcel; Hoti, Agim; Tonh, Mok; and Vut, Keo, "Evaluation Report on ECHO Funded Humanitarian Mine Action Pilot Projects in North-West of Cambodia" (2003). Global CWD Repository. 1132. https://commons.lib.jmu.edu/cisr-globalcwd/1132 This Article is brought to you for free and open access by the Center for International Stabilization and Recovery at JMU Scholarly Commons. It has been accepted for inclusion in Global CWD Repository by an authorized administrator of JMU Scholarly Commons. For more information, please contact [email protected]. EVALUATION REPORT ON ECHO FUNDED HUMANITARIAN MINE ACTION PILOT PROJECTS IN NORTH-WEST OF CAMBODIA th October 6 2003 Marcel Durocher Agim Hoti Mok Tonh Keo Vuthy TABLE OF CONTENTS ACRONYMS AND ABBREVIATIONS.......................................................................................................... 5 ACKNOWLEDGEMENTS .............................................................................................................................. 6 INTRODUCTION............................................................................................................................................ -

Microsoft Office 2000
Six-month Narrative Report Project title “Strengthening Indigenous Leadership towards sustainable land and natural resource management in Preah Vihear Province through People - Led development approach” 1st January to 30th June, 2016 Ms. Rona Smit, a Special Report of United Nation meeting with NGOs Prey Preah Rokar Community Network and independent Monk network in Preah Vihea Province March 29, 2016 for Social Justice conducted forest campaign June 09, 2016 Mr. Oum Mara, Preah Vihear provincial governor signed the agreement IP communities and people whose land affected by ELC protested in with community leaders who protest against land grabbing by ELC Jan front of Preah Vihear provincial hall to demand authority to protect 04, 2016 and solved land conflict, December 28, 2015 -Jan 04, 2016 Submitted on July 03, 2016 Prepared By Checked by Poek Sophorn & Tem Ven, Ang Cheatlom Area Program Coordinators Executive Director PKH Semester Report (Jan-June) 2016 1 Table of Contents List of abbreviations ........................................................................................................................................ 3 Executive Summary ......................................................................................................................................... 4 1. Introduction to the project .................................................................................................................... 5 2. Implemented Project Activities and Achievements ..................................................................... -
Environmental Safeguards Due Diligence Report Cambodia: Third
Environmental Safeguards Due Diligence Report April 2021 Cambodia: Third Rural Water Supply and Sanitation Services Sector Development Program Seventeen (17) Subprojects in Nine (9) Provinces: Banteay Meanchey, Battambang, Kampong Chhnang, Kampot, Kampong Speu, Kampong Thom, Preah Vihear, Pursat, and Siem Reap Province Main Report and Annex 1 to Annex 5 Prepared by Ministry of Rural Development for the Royal Government of Cambodia and the Asian Development Bank. This environmental safeguards due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Environmental Safeguards Due Diligence Report 5 April 2021 Resubmitted 18 May 2021 Cambodia: Third Rural Water Supply and Sanitation Service Sector Development Project Seventeen (17) Subprojects in Nine (9) Provinces: Banteay Meanchey, Battambang, Kampong Chhnang, Kampot, Kampong Speu, Kampong Thom, Preah Vihear, Pursat, and Siem Reap Province Prepared by Ministry of Rural Development for the Royal Government of Cambodia and the Asian Development Bank. This environmental safeguard due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. -
2016 Voter Registration Monitoring and Observation Report February
2016 Voter Registration Monitoring and Observation Report February 2017 1 Table of Contents: I. Executive Summary: ......................................................................................................................... 2 II. Background and Introduction ..................................................................................................... 4 III. NEC - Irregularities and Complaints ..................................................................................... 10 A. Data error irregularities reported by the NEC................................................................... 10 B. Complaint settlement reported by the NEC ........................................................................ 11 IV. Registration Monitoring Results ............................................................................................ 15 A. Observation on the Conduct of Preparatory Logistics: Recruitment and Training of Registration Staff .....................................................................................................................15 B. Checklist based survey monitoring: observation process and results .................... 18 C. Major Areas of Concern and Needed Reform ..................................................................... 29 Appendix ................................................................................................................................................. 37 2 I. Executive Summary: Findings and Recommendations The NEC announced Letter for registration -
Annual Report Annual Report
Cambodia Road Crash and Victim Information System Annual Report © HIB Developed by: Ministry of Interior Ministry of Health Ministry of Public Works Handicap International Belgium and Transport Notice: This report may be freely reviewed, abstracted, reproduced or translated in part or in whole, but not for the purposes of sale. Website: www.roadsafetycambodia.info Cambodia Road Crash and Victim Information System Annual Report 2008 Table of Contents List of Figures.......................................................................................................................................................... 3 Foreword .................................................................................................................................................................. 5 Foreword .................................................................................................................................................................. 5 Note from the Minister of Public Works and Transport............................................................................. 5 Note from the Minister of Health ............................................................................................................... 6 Note from the Ministry of Interior............................................................................................................... 7 Note from World Health Organization....................................................................................................... 8 Note from Handicap -
Interim Workshop
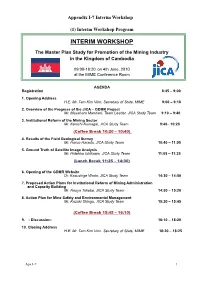
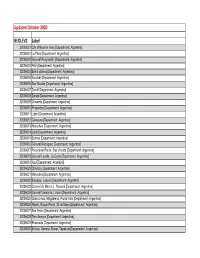
Appendix I-7 Interim Workshop (1) Interim Workshop Program INTERIM WORKSHOP The Master Plan Study for Promotion of the Mining Industry in the Kingdom of Cambodia 09:00-18:20, on 4th June, 2010 at the MIME Conference Room AGENDA Registration 8:45 – 9:00 1. Opening Address H.E. Mr. Tam Kim Vinn, Secretary of State, MIME 9:00 – 9:10 2. Overview of the Progress of the JICA – GDMR Project Mr. Masaharu Marutani, Team Leader, JICA Study Team 9:10 – 9:40 3. Institutional Reform of the Mining Sector Mr. Kenichi Kumagai, JICA Study Team 9:40– 10:20 (Coffee Break 10:20 – 10:40) 4. Results of the Field Geological Survey Mr. Haruo Harada, JICA Study Team 10:40 – 11:05 5. Ground Truth of Satellite Image Analysis Mr. Hidehiro Ishikawa, JICA Study Team 11:05 – 11:25 (Lunch Break 11:25 – 14:30) 6. Opening of the GDMR Website Dr. Kazushige Wada, JICA Study Team 14:30 – 14:50 7. Proposed Action Plans for Institutional Reform of Mining Administration and Capacity Building Mr. Naoya Takebe, JICA Study Team 14:50 – 15:20 8. Action Plan for Mine Safety and Environmental Management Mr. Kazuki Shingu, JICA Study Team 15:20 – 15:45 (Coffee Break 15:45 – 16:10) 9. - Discussion- 16:10 – 18:20 10. Closing Address H.E. Mr. Tam Kim Vinn, Secretary of State, MIME 18:20 – 18:25 Apx I-7 1 (2) The List of Participants The List of Participants on the Interim Workshop on 4th June, 2010 No. Name Title Organization 1 H.E Mr. -
GEOLEV2 Label Updated October 2020
Updated October 2020 GEOLEV2 Label 32002001 City of Buenos Aires [Department: Argentina] 32006001 La Plata [Department: Argentina] 32006002 General Pueyrredón [Department: Argentina] 32006003 Pilar [Department: Argentina] 32006004 Bahía Blanca [Department: Argentina] 32006005 Escobar [Department: Argentina] 32006006 San Nicolás [Department: Argentina] 32006007 Tandil [Department: Argentina] 32006008 Zárate [Department: Argentina] 32006009 Olavarría [Department: Argentina] 32006010 Pergamino [Department: Argentina] 32006011 Luján [Department: Argentina] 32006012 Campana [Department: Argentina] 32006013 Necochea [Department: Argentina] 32006014 Junín [Department: Argentina] 32006015 Berisso [Department: Argentina] 32006016 General Rodríguez [Department: Argentina] 32006017 Presidente Perón, San Vicente [Department: Argentina] 32006018 General Lavalle, La Costa [Department: Argentina] 32006019 Azul [Department: Argentina] 32006020 Chivilcoy [Department: Argentina] 32006021 Mercedes [Department: Argentina] 32006022 Balcarce, Lobería [Department: Argentina] 32006023 Coronel de Marine L. Rosales [Department: Argentina] 32006024 General Viamonte, Lincoln [Department: Argentina] 32006025 Chascomus, Magdalena, Punta Indio [Department: Argentina] 32006026 Alberti, Roque Pérez, 25 de Mayo [Department: Argentina] 32006027 San Pedro [Department: Argentina] 32006028 Tres Arroyos [Department: Argentina] 32006029 Ensenada [Department: Argentina] 32006030 Bolívar, General Alvear, Tapalqué [Department: Argentina] 32006031 Cañuelas [Department: Argentina] -

Usaid Greening Prey Lang Annual Report #2 October 1, 2019 – September 30, 2020
PHOTO CREDIT: USAID Greening Prey Lang USAID GREENING PREY LANG ANNUAL REPORT #2 OCTOBER 1, 2019 – SEPTEMBER 30, 2020 November 2020 This publication was produced for review by the United States Agency for International Development. It was prepared by Tetra Tech. This publication was produced for review by the United States Agency for International Development by Tetra Tech, through USAID Contract No. 72044218C00001, USAID Greening Prey Lang Activity. This report was prepared by: Tetra Tech 159 Bank Street, Suite 300 Burlington, Vermont 05401 USA Telephone: (802) 495-0282 Fax: (802) 658-4247 Email: [email protected] Tetra Tech Contacts: Matthew Edwardsen, Chief of Party Telephone: +855 (0) 85/6 888 416 Email: [email protected] Patricia Caffrey, Project Manager Telephone: +1 (802) 495-0303 Email: [email protected] Cover Photo: Treehouse at BeTreed Adventures in Phnom Thnout-Phnom Pok Wildlife Sanctuary, Preah Vihear province. Credit: USAID Greening Prey Lang. USAID GREENING PREY LANG ANNUAL REPORT #2 OCTOBER 1, 2019 – SEPTEMBER 30, 2020 November 2020 Date original report submitted to USAID: November 14, 2020 Date comments received from USAID: December 1, 2020 Date revised report submitted to USAID: December 4, 2020 & December 10, 2020 Date report approved by USAID: December 10, 2020 DISCLAIMER The author’s views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. TABLE OF CONTENTS TABLE -

Plasmodium Prevalence and Artemisinin
Bosman et al. Malaria Journal 2014, 13:394 http://www.malariajournal.com/content/13/1/394 RESEARCH Open Access Plasmodium prevalence and artemisinin-resistant falciparum malaria in Preah Vihear Province, Cambodia: a cross-sectional population-based study Philippe Bosman1, Jorgen Stassijns1*, Fabienne Nackers2, Lydie Canier3, Nimol Kim3, Saorin Khim3, Sweet C Alipon4, Meng Chuor Char5, Nguon Chea5, Lek Dysoley5, Rafael Van den Bergh1, William Etienne1, Martin De Smet1, Didier Ménard3 and Jean-Marie Kindermans1 Abstract Background: Intensified efforts are urgently needed to contain and eliminate artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion. Médecins Sans Frontières plans to support the Ministry of Health in eliminating P. falciparum in an area with artemisinin resistance in the north-east of Cambodia. As a first step, the prevalence of Plasmodium spp. and the presence of mutations associated with artemisinin resistance were evaluated in two districts of Preah Vihear Province. Methods: A cross-sectional population-based study using a two-stage cluster sampling was conducted in the rural districts of Chhaeb and Chey Saen, from September to October 2013. In each district, 30 clusters of 10 households were randomly selected. In total, blood samples were collected for 1,275 participants in Chhaeb and 1,224 in Chey Saen. Prevalence of Plasmodium spp. was assessed by PCR on dried blood spots. Plasmodium falciparum positive samples were screened for mutations in the K13-propeller domain gene (PF3D7_1343700). Result: The prevalence of Plasmodium spp. was estimated at 1.49% (95% CI 0.71–3.11%) in Chhaeb and 2.61% (95% CI 1.45–4.66%) in Chey Saen. -

Acleda 2013 Annualrepo
VISION AND MISSION Vision ACLEDA Bank’s vision is to be Cambodia’s leading commercial bank providing superior financial services to all segments of the community. Mission Our mission is to provide micro, small and medium entrepreneurs with the wherewithal to manage their financial resources efficiently and by doing so to improve the quality of their lives. By achieving these goals we will ensure a sustainable and growing benefit to our shareholders, our staff and the community at large. We will at all times observe the highest principles of ethical behaviour, respect for society, the law and the environment. This report has been prepared and issued by the Marketing Division of ACLEDA Bank Plc., to whom any comments or requests for further information should be sent. Headquarters: #61, Preah Monivong Blvd., Sangkat Srah Chork, Khan Daun Penh, Phnom Penh, Kingdom of Cambodia. P.O. Box: 1149 Tel: +855 (0)23 998 777 / 430 999 Fax: +855 (0)23 998 666 / 430 555 E-mail: [email protected] Website: www.acledabank.com.kh SWIFT Code: ACLBKHPP Call Center (24/7) Tel: +855 (0)23 994 444, +855 (0)15 999 233 E-mail: [email protected] 1 FINANCIAL RESULTS 31/12/13 31/12/12 31/12/11 31/12/10 31/12/09 Change Units in US$ ‘000 Audited Audited Audited Audited Audited (%)1 Consolidated Financial Results Assets 2,407,791 1,982,743 1,526,873 1,192,134 922,573 21.44% Loans and Advances 1,527,680 1,294,789 1,023,924 749,656 539,714 17.99% Liabilities 2,021,546 1,716,119 1,336,179 1,051,543 812,063 17.80% Deposits 1,709,596 1,507,751 1,174,966 -

Address of ACLEDA Bank Plc
Address of ACLEDA Bank Plc No. Office Name Address Tel/Fax/E-mail I- HEADQUARTERS Tel: (855) 23 430 999 / 998 777 Fax: (855) 23 430 555 E-mail: [email protected] For Customer Inquiry Call: #61, Preah Monivong Blvd., Sangkat Srah Chork, Khan Daun Penh, Phnom Penh. Tel: (855) 23 994 444 (855) 15 999 233 P.O. Box: 1149 HEADQUARTERS (OPERATION DIVISION) E-mail: [email protected] 1 Website: www.acledabank.com.kh SWIFT Code: ACLBKHPP OPERATION DIVISION Tel: (855) 23 998 340 Fax: (855) 23 998 316 E-mail: [email protected] II- CAPITAL BRANCHES No 29 and 30CD, Street 217 and 213, Group 63, Phum 7, Sangkat Veal Vong, Khan Prampir Meakkakra, Phnom Tel: (855) 23 997 169 / 179 / 189 Penh. (855) 15 900 342 PHNOM PENH Branch P.O. Box: 1149 2 (855) 23 881 465 / 224 Website: www.acledabank.com.kh E-mail: [email protected] SWIFT Code: ACLBKHPP No 252 ABCD, Preah Monivong Blvd., Group 40, Phum 10, Sangkat Boeng Reang, Khan Doun Penh, Phnom Penh. Tel: (855) 23 222 626 / 424 P.O. Box: 1149 DOUN PENH Branch (855)-15 900 254 3 Website: www.acledabank.com.kh E-mail: [email protected] SWIFT Code: ACLBKHPP No 46, Russian Federation Blvd., Group 1, Paprak Khang Tboung Village, Sangkat Kakab 1, Khan Pur SenChey, Phnom Penh. Tel: (855) 15 900 252 POCHENTONG Branch P.O. Box: 1149 4 E-mail: [email protected] Website: www.acledabank.com.kh SWIFT Code: ACLBKHPP No 482, Group 6, Phum Spean Khpous, Sangkat Kilometre N0.6, Khan Russey Keo, Phnom Penh.