Pseudoephidrine and Diving (.Pdf)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia and Respiratory Heat Loss While Scuba Diving
HYPOTHERMIA AND RESPIRATORY HEAT LOSS WHILE SCUBA DIVING Kateřina Kozáková Faculty of Physical Education and Sport, Charles University in Prague, Department of Biomedical Labo- ratory Abstract One of the factors affecting length of stay under water of a diver is heat comfort. During scuba diving there is an increased risk of hypothermia. Hypothermia is one of the most life threatening factors of a diver and significantly affects his performance. The body heat loss runs by different mechanisms. One of them is the respiratory mechanism, which is often overlooked. Compressed dry air or other media is coming out from the cylinder, which have to be heated and humidified to a suitable value. Thus the organism loses body heat and consequently energy. Based on literature search the article will describe safe dive time in terms of hypo- thermia in connection to respiratory heat loss. Key words: hypothermia, heat loss, respiration, scuba diving, water environment Souhrn Jedním z faktorů ovlivňujících délku pobytu potápěče pod vodou je tepelný komfort. Během výkonu přístro- jového potápění hrozí zvýšené riziko hypotermie. Hypotermie představuje jedno z nejzávažnějších ohrožení života potápěče a zásadně ovlivňuje jeho výkon. Ke ztrátám tělesného tepla dochází různými mechanismy. Jednou cestou tepelných ztrát je ztráta tepla dýcháním, která je často opomíjená. Z potápěčského přístroje vychází suchý stlačený vzduch nebo jiné médium, který je třeba při dýchání ohřát a zvlhčit na potřebnou hodnotu. Tím organismus ztrácí tělesné teplo a potažmo energii. Tento článek, na základě literární rešerše, popíše bezpečnou dobou ponoru z hlediska hypotermie a v souvislosti se ztrátou tepla dýcháním. Klíčová slova: hypotermie, ztráta tepla, dýchání, přístrojové potápění, vodní prostředí Introduction amount of body heat. -

THE PHYSICIAN's GUIDE to DIVING MEDICINE the PHYSICIAN's GUIDE to DIVING MEDICINE Tt",,.,,,,., , ••••••••••• ,
THE PHYSICIAN'S GUIDE TO DIVING MEDICINE THE PHYSICIAN'S GUIDE TO DIVING MEDICINE tt",,.,,,,., , ••••••••••• , ......... ,.", •••••••••••••••••••••••• ,. ••. ' ••••••••••• " .............. .. Edited by Charles W. Shilling Catherine B. Carlston and Rosemary A. Mathias Undersea Medical Society Bethesda, Maryland PLENUM PRESS • NEW YORK AND LONDON Library of Congress Cataloging in Publication Data Main entry under title: The Physician's guide to diving medicine. Includes bibliographies and index. 1. Submarine medicine. 2. Diving, Submarine-Physiological aspects. I. Shilling, Charles W. (Charles Wesley) II. Carlston, Catherine B. III. Mathias, Rosemary A. IV. Undersea Medical Society. [DNLM: 1. Diving. 2. Submarine Medicine. WD 650 P577] RC1005.P49 1984 616.9'8022 84-14817 ISBN-13: 978-1-4612-9663-8 e-ISBN-13: 978-1-4613-2671-7 DOl: 10.1007/978-1-4613-2671-7 This limited facsimile edition has been issued for the purpose of keeping this title available to the scientific community. 10987654 ©1984 Plenum Press, New York A Division of Plenum Publishing Corporation 233 Spring Street, New York, N.Y. 10013 All rights reserved No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording, or otherwise, without written permission from the Publisher Contributors The contributors who authored this book are listed alphabetically below. Their names also appear in the text following contributed chapters or sections. N. R. Anthonisen. M.D .. Ph.D. Professor of Medicine University of Manitoba Winnipeg. Manitoba. Canada Arthur J. Bachrach. Ph.D. Director. Environmental Stress Program Naval Medical Research Institute Bethesda. Maryland C. Gresham Bayne. -
Darling Marine Center Local Shore Diving Guide
Darling Marine Center Local Shore Diving Guide University of Maine Scientific Diving Program Table of Contents Recommended Equipment List……………………………………………………………..2 Local Information…………………………………………………………………………...3 Recompression Chambers…………………………………………………………………..3 General Emergency Action Plan…………………………………………………………….3-4 Documentation……………………………………………………………………………….4 Dive Sites DMC Pier……………………………………………………………………………5-6 Kresge Point………………………………………………………………………….7-8 Lowes Cove Mooring Field…………………………………………………………..9-10 Pemaquid Point……………………………………………………………………….11-12 Rachel Carson Preserve………………………………………………………………13-15 Sand Cove…………………………………………………………………………….16-17 Thread of life…………………………………………………………………………18-19 Appendix………………………………………………………………………………………20 1 Recommended Equipment List • Dive flag • DAN oxygen and first aid kit • Spare tank • Extra weights • Save-a-dive kit • Dive slate/underwater paper (recording purposes) Recommended Personal Equipment • Exposure suit- minimum7mm wetsuit o Booties o Gloves o Hood o Wool socks • Fins • BCD • Mask, Snorkel • Weights • Surface marker buoy • Dive watch • Dive computer • Knife/cutting tool 2 Local Information: Fire, Medical, Police 911 Emergency Dispatch Lincoln County Emergency (207)563-3200 Center Nearest Hospital Lincoln Health-Miles (207)563-1234 Campus USCG Boothbay (207)633-2661 Divers Alert Network Emergency hotline 1-919-684-9111 Medical information 1-919-684-2948 Diving Safety Officer Christopher Rigaud (207)563-8273 Recompression Chambers: In the event of a diving accident, call 911 and facilitate transport of victim to a hospital or medical facility. The medical staff will determine whether hyperbaric treatment is needed. St. Mary’s Regional Lewiston, ME (207)777-8331 Will NOT accept Medical Center divers after 4:30pm St. Joseph’s Hospital Bangor, ME (207)262-1550 Typically, available after hours Wound and Beverly, MA (978)921-1210 Hyperbaric Medicine Basic Emergency Information: See Appendix for the approved Emergency Action Plan by the UMaine DCB. -

Diving and Hyperbaric Medicine
Diving and Hyperbaric Medicine 7KH-RXUQDORIWKH6RXWK3DFL¿F8QGHUZDWHU0HGLFLQH6RFLHW\ ,QFRUSRUDWHGLQ9LFWRULD $% ISSN 1833 - 3516 Volume 37 No. 4 ABN 29 299 823 713 December 2007 Diving expeditions: from Antarctica to the Tropics Diving deaths in New Zealand Epilepsy and diving – time for a change? Mechanical ventilation of patients at pressure Print Post Approved PP 331758/0015 9^k^c\VcY=neZgWVg^XBZY^X^cZKdajbZ(,Cd#)9ZXZbWZg'%%, PURPOSES OF THE SOCIETY IdegdbdiZVcY[VX^a^iViZi]ZhijYnd[VaaVheZXihd[jcYZglViZgVcY]neZgWVg^XbZY^X^cZ Idegdk^YZ^c[dgbVi^dcdcjcYZglViZgVcY]neZgWVg^XbZY^X^cZ IdejWa^h]V_djgcVa IdXdckZcZbZbWZghd[i]ZHdX^ZinVccjVaanViVhX^Zci^ÄXXdc[ZgZcXZ OFFICE HOLDERS EgZh^YZci 9g8]g^h6Xdii (%EVg`6kZcjZ!GdhhancEVg` :çbV^a1XVXdii5deijhcZi#Xdb#Vj3 Hdji]6jhigVa^V*%,' EVhiçEgZh^YZci 9gGdWncLVa`Zg &'7VggVaa^ZgHigZZi!<g^[Äi] :çbV^a1GdWnc#LVa`Zg5YZ[ZcXZ#\dk#Vj3 68I'+%( HZXgZiVgn 9gHVgV]H]Vg`Zn E#D#7DM&%*!CVggVWZZc :çbV^a1hejbhhZXgZiVgn5\bV^a#Xdb3 CZlHdji]LVaZh'&%& IgZVhjgZg 9g<jnL^aa^Vbh E#D#7dm&.%!GZY=^aaHdji] :çbV^a1hejbh5[VhibV^a#cZi3 K^Xidg^V(.(, :Y^idg 6hhdX#Egd[#B^`Z9Vk^h 8$d=neZgWVg^XBZY^X^cZJc^i :çbV^a1hejbh_5XY]W#\dki#co3 8]g^hiX]jgX]=dhe^iVa!Eg^kViZ7V\),&%!8]g^hiX]jgX]!CO :YjXVi^dcD[ÄXZg 9g;^dcVH]Vge ').XC^X]dahdcGdVY!H]ZcidcEVg` :çbV^a1h]Vge^Z[5YdXidgh#dg\#j`3 LZhiZgc6jhigVa^V+%%- EjWa^XD[ÄXZg 9gKVcZhhV=VaaZg E#D#7dm-%'(!8Vggjb9dlch :çbV^a1kVcZhhV#]VaaZg5XYbX#Xdb#Vj3 K^Xidg^V('%& 8]V^gbVc6CO=B< 9g9Vk^YHbVgi 9ZeVgibZcid[9^k^c\VcY=neZgWVg^XBZY^X^cZ :çbV^a1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 GdnVa=dWVgi=dhe^iVa!=dWVgi!IVhbVc^V,%%% LZWbVhiZg -

Training Objectives for a Diving Medical Physician
The Diving Medical Advisory Committee Training Objectives for a Diving Medicine Physician This guidance includes all the training objectives agreed by the Diving Medical Advisory Committee, the European Diving Technology Committee and the European Committee for Hyperbaric Medicine in 2011. Rev 1 - 2013 INTRODUCTION The purpose of this document is to define more closely the training objectives in diving physiology and medicine that need to be met by doctors already fully accredited or board-certified in a clinical speciality to national standards. It is based on topic headings that were originally prepared for a working group of European Diving Technology Committee (EDTC) and the European Committee of Hyperbaric Medicine (ECHM) as a guide for diving medicine some 20 years ago by J.Desola (Spain), T.Nome (Norway) & D.H.Elliott (U.K.). The training now required for medical examiners of working divers and for specialist diving medicine physicians was based on a EDTC/ECHM standard 1999 and subsequently has been enhanced by the Diving Medical Advisory Committee (DMAC), revised and agreed in principle by DMAC, EDTC and ECHM in 2010 and then ratified by EDTC and ECHM in 2011. The requirements now relate to an assessment of competence, the need for some training in occupational medicine, the need for maintenance of those skills by individual ‘refresher training’. Formal recognition of all this includes the need to involve a national authority for medical education. These objectives have been applied internationally to doctors who provide medical support to working divers. (Most recreational instructors and dive guides are, by their employment, working divers and so the guidance includes the relevant aspects of recreational diving. -

K Robinson, M Byers. Diving Medicine
J R Army Med Corps 2005; 151: 256-263 J R Army Med Corps: first published as 10.1136/jramc-151-04-07 on 1 December 2005. Downloaded from Diving Medicine K Robinson, M Byers with diving. This article aims to review the physics and physiology of diving, discuss the common medical conditions that occur whilst diving, and consider the current thinking in relation to aetiol- ogy and treatment. A Brief History of Diving Breath-hold diving has probably been around from before written history. Divers were reportedly used in the Trojan Wars (1194-1184 BC) to disrupt the enemy navies. Aristotle described ruptured tympan- ic membranes and ear infections in sponge divers, and Marco Polo wrote of pearl divers reaching depths of 27 metres. Alexander the Great is supposed to have made a dive in a primitive diving bell, Roger Bacon described men walking on the seabed in 1240, and in 1535 Guglielmo de Lorena developed the first true diving bell (3). In 1774 Freminet used a bellows to deliv- er air from the surface to a diver and Siebe Introduction developed the diving suit in 1819 (3). This It could be argued that diving is the most consisted of a copper helmet and jacket, extreme sport of all. Survival in such a which was modified in 1839 to resemble the hostile underwater environment is waterproof suit recognised and in regular use http://militaryhealth.bmj.com/ dependent on sophisticated breathing to the present day. apparatus and an understanding of the Self-contained underwater breathing inherent risks. Diving incidents are well apparatus (SCUBA) was also developed in publicised, not least because of the the 19th century and in 1943 Jacques severe injuries that ensue, but remain an Cousteau and Emile Gagnan demonstrated uncommon occurrence. -

The Development of Hyperbaric and Diving Medicine in Singapore Chng J, Low C T E, Kang W L
Review Article Singapore Med J 2011; 52(12) : 901 The development of hyperbaric and diving medicine in Singapore Chng J, Low C T E, Kang W L ABSTRACT HBOT has had a long history that began when the Hyperbaric oxygen therapy is a noninvasive first hyperbaric treatment chamber or ‘domicilium’ therapy used in the treatment of diving-related was constructed in 1662 by a British clergyman named medical illnesses. It is an important adjunct in the Henshaw, who utilised it to treat a multitude of medical management of a variety of medical conditions. conditions.(3) Since then, there have been many reports of The Republic of Singapore Navy Medical Service the beneficial effects of increased pressure, and by 1877, (NMS) is the main driver of the development of chambers were used widely for many conditions.(4) In 1879, hyperbaric and diving medicine in Singapore. the use of hyperbaric therapy to prolong safe anaesthesia The practice of hyperbaric medicine has during surgery was realised.(5) In the early 1900s, the use of inherent risks, and unregulated application of HBOT to treat medical problems became more prevalent. this therapy may do more harm than good. NMS The late 1950s and early 1960s are believed by many to be and Singapore General Hospital (SGH) signed the birth of modern-day hyperbaric medicine. One large a Memorandum of Understanding to combine contribution was made by Dr I Boerema. He conceived NMS’s experience with the clinical expertise the idea of ‘drenching’ tissues with oxygen by increasing of SGH to provide holistic care for diving and the ambient pressure surrounding the patient. -

Medical Aspects of Harsh Environments, Volume 2, Chapter
Military Diving Operations and Medical Support Chapter 31 MILITARY DIVING OPERATIONS AND MEDICAL SUPPORT † RICHARD D. VANN, PHD*; AND JAMES VOROSMARTI, JR, MD INTRODUCTION BREATH-HOLD DIVING CENTRAL NERVOUS SYSTEM OXYGEN TOXICITY IN COMBAT DIVERS UNDERWATER BREATHING APPARATUS Open-Circuit Self-Contained Underwater Breathing Apparatus: The Aqualung Surface-Supplied Diving Closed-Circuit Oxygen Scuba Semiclosed Mixed-Gas Scuba Closed-Circuit, Mixed-Gas Scuba THE ROLE OF RESPIRATION IN DIVING INJURIES Carbon Dioxide Retention and Dyspnea Interactions Between Gases and Impaired Consciousness Individual Susceptibility to Impaired Consciousness DECOMPRESSION PROCEDURES No-Stop (No-Decompression) Dives In-Water Decompression Stops Surface Decompression Repetitive and Multilevel Diving Dive Computers Nitrogen–Oxygen Diving Helium–Oxygen and Trimix Diving Omitted Decompression Flying After Diving and Diving at Altitude The Safety of Decompression Practice SATURATION DIVING Atmospheric Control Infection Hyperbaric Arthralgia Depth Limits Decompression THERMAL PROTECTION AND BUOYANCY TREATMENT OF DECOMPRESSION SICKNESS AND ARTERIAL GAS EMBOLISM Therapy According to US Navy Treatment Tables Decompression Sickness in Saturation Diving MEDICAL STANDARDS FOR DIVING SUBMARINE RESCUE AND ESCAPE SUMMARY *Captain, US Navy Reserve (Ret); Divers Alert Network, Center for Hyperbaric Medicine and Environmental Physiology, Box 3823, Duke University Medical Center, Durham, North Carolina 27710 †Captain, Medical Corps, US Navy (Ret); Consultant in Occupational, Environmental, and Undersea Medicine, 16 Orchard Way South, Rockville, Maryland 20854 955 Military Preventive Medicine: Mobilization and Deployment INTRODUCTION Divers breathe gases and experience pressure land) teams and two SEAL delivery vehicle (SDV) changes that can cause different injuries from those teams. SEALs are trained for reconnaissance and encountered by most combatant or noncombatant direct action missions at rivers, harbors, shipping, military personnel. -
Underwater Medicine
TEMPLE UNIVERSITY COURSE REGISTRATION FORM UNDERWATER MEDICINE 2016 UNDERWATER MEDICINE 2016 A training program in diving medicine designed with special emphasis on diagnosis and treatment of diving disorders, REGISTRATION FEE: $650.00** fitness for diving and hyperbaric oxygen therapy. This $750 after Dec 30, 2015 program is certified for 25 AMA PRA category 1 credits $850 for registrants not in the UMA package through Temple University School of Medicine. The program Fee includes: Lectures and Course Materials. is offered in collaboration with the Undersea and Hyperbaric Medical Society. Enclosed is my check in the amount of $650.00 for registration. Make checks payable to Underwater Medicine Associates. presents the COURSE DESCRIPTION Return to: Medical evaluation of a diver or diving candidate demands that the physician have a knowledge of the unique physical Underwater Medicine Associates 42 nd Annual qualifications needed for this sport. In this year’s program, P.O. BOX 481 we will pay special attention to diagnosing diving disorders, Bryn Mawr, PA 19010 and will provide a combination of didactic lectures and case examples with interactive discussions to enhance learning **Course Registration Fee and Hotel Registration Deposit can related to diagnosis of diving disorders, assessment for fitness be combined on one check, or paid by credit card UNDERWATER to dive, marine injuries and toxicity and hyperbaric oxygen therapy. Upon completion of the course, participants should have a general knowledge of diving medicine and medical NAME_______________________________DEGREE______ -

PARTICIPANT INFORMATION SHEET DAN Rebreather Study 2020 - Caustic Cocktail IRB #025-20-20 (Expiry: 2021-08-05)
PARTICIPANT INFORMATION SHEET DAN Rebreather Study 2020 - Caustic Cocktail IRB #025-20-20 (expiry: 2021-08-05) CONCISE SUMMARY This survey aims to collect data from rebreather divers regarding their experiences with caustic cocktail(s) while diving. You qualify for participation in this study if you are a certified rebreather diver and you have experienced a caustic cocktail or dived with someone who experienced a caustic cocktail. There are no individual benefits and no currently foreseeable risks to you in participating in this study. If you are interested in learning more about the study, please continue reading and review the following pages carefully before agreeing to participate. INTRODUCTION You are invited to complete a short survey about rebreather diving. The study is entirely sponsored by DAN. PURPOSE OF THE STUDY The purpose of this study is to collect information from adult rebreather divers and their experiences with a “Caustic Cocktail”. BACKGROUND When water mixes with the carbon-dioxide absorbent in rebreathers, e.g. due to a leak in the unit, a solution of caustic soda is produced. When a diver ingests this poisonous mixture, known as a “Caustic Cocktail”, it is important to provide appropriate first aid. It is uncertain how common suffering a caustic cocktail is among certified rebreather divers, or what immediate first-aid treatments are being employed. This survey will gather information on rebreather divers and their diving experience, including whether they have suffered a caustic cocktail event and how it was treated. HOW THE STUDY WORKS Certified rebreather divers aged 18 years or older at the time of completing the survey are invited to participate. -
Decompression Sickness (DCS) “Bends”
SLMA Guide to Management of Decompression Sickness (DCS) “Bends” A collaborative Publication of the Sri Lanka Medical Association and the Directorate of Health Services – Sri Lanka Navy 2013 These guidelines are the result of a long-term collaboration between divers with experience in caring for DCS victims, doctors and diving officers of the Sri Lanka Navy with experience in administering Hyperbaric Oxygen (HBO) treatment to such victims, a doctor who is a trained SCUBA diver with knowledge of the subject and a neurophysician with experience in treating victims who have not undergone recompression therapy. Edited by Malik Fernando for the Sri Lanka Medical Association and the Directorate of Health Services – Sri Lanka Navy November 2013 Updated May 2018 Published by Sri Lanka Medical Association ‘Wijerama House’ 6, Wijerama Mawatha Colombo 7 Guide to Management of Decompression Sickness (DCS) “Bends” A collaborative Publication of the Sri Lanka Medical Association and the Directorate of Health Services of the Sri Lanka Navy Decompression sickness (DCS), commonly called ‘bends’, is a condition seen in those who have breathed compressed air, such as SCUBA divers, for too long at too high a pressure and who have returned to atmospheric pressure too quickly. This happens when they do not follow recommended diving protocols and come up to atmospheric pressure after a prolonged period at a great depth so rapidly that there is no time for inert gases dissolved in the blood and tissues to be eliminated. The result is that bubbles of nitrogen form in the blood and tissues due to the rapid reduction of ambient pressure. -
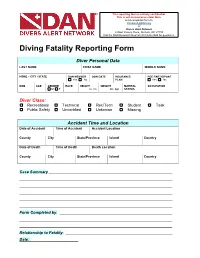
Diving Fatality Reporting Form
This reporting form is entirely confidential. This is not an insurance claim form. send completed form to: [email protected] or Divers Alert Network 6 West Colony Place, Durham, NC 27705 Call the DAN Research Dept at (919) 684-2948 for questions. Diving Fatality Reporting Form Diver Personal Data LAST NAME FIRST NAME MIDDLE NAME HOME – CITY / STATE DAN MEMBER JOIN DATE INSURANCE PDE PARTICIPANT Yes No PLAN Yes No DOB AGE GENDER RACE HEIGHT WEIGHT MARITAL OCCUPATION M F in cm lbs kgs STATUS Diver Class: Recreational Technical Rec/Tech Student Task Public Safety Uncertified Unknown Missing Accident Time and Location Date of Accident Time of Accident Accident Location County City State/Province Island Country Date of Death Time of Death Death Location County City State/Province Island Country Case Summary Form Completed by: Relationship to Fatality: Date: Name: Case #: Diver Experience CERTIFIED DIVER YEAR of INITIAL CERTIFYING AGENCY(s) Yes No CERTIFICATION # DIVES in LAST 12 MONTHS # DIVES in LAST 5 YEARS LAST DIVE PRECEDING ACCIDENT Days Months Years CERTIFICATION LEVEL Student Rescue Technical Military Basic/Open Water Master/Asst. Instructor Commercial None Advanced/Specialty Instructor and Above Scientific Other: GENERAL EXPERIENCE LEVEL Uncertified Inexperienced (6-20) Advanced (41-60) Novice (0-5 dives) Intermediate (21-40) Experienced (61+ dives) Diver Health PREVIOUS DIVE ACCIDENT If yes, what year SMOKE CIGARETTES # packs / week # years smoking Yes No Yes No Past PREVIOUS CONDITIONS CURRENT CONDITIONS CURRENT MEDICATIONS MEDICATION