Diving and Hyperbaric Medicine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Inquest Finding
Coroners Act 1996 [Section 26(1)] Western Australia RECORD OF INVESTIGATION INTO DEATH Ref No: 18/17 I, Barry Paul King, Coroner, having investigated the death of Jarrod Arthur Hampton with an inquest held at the Perth Coroner’s Court on 15 May 2017 to 18 May 2017 and on 22 May 2017 to 26 May 2017, find that the identity of the deceased person was Jarrod Arthur Hampton and that death occurred on 14 April 2012 in the waters of the Indian Ocean approximately 90 nautical miles south of Broome from drowning secondary to incapacitation from air embolism in the following circumstances: Counsel Appearing: Sergeant L Housiaux assisted the Coroner Ms G A Archer SC (instructed by Corrs Chambers Westgarth) and Mr N D Ellery appeared for Paspaley Pearling Company Pty Ltd Mr A Coote appeared for the deceased’s family Mr P Hopwood appeared for the Pearl Producers Association Ms H C Richardson (State Solicitors Office) appeared for WorkSafe Table of Contents INTRODUCTION .............................................................................................................. 2 THE EVIDENCE ................................................................................................................ 4 THE DECEASED ............................................................................................................... 8 THE DECEASED’S DIVING BACKGROUND ....................................................................... 9 THE DECEASED’S SHOULDER AND PECTORALIS MAJOR .............................................. 10 THE DECEASED JOINS -
What Chamber Operators Should Know About Ear Barotrauma (And How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018
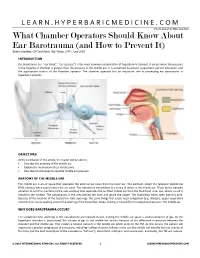
LEARN.HYPERBARICMEDICINE.COM International ATMO Education What Chamber Operators Should Know About Ear Barotrauma (and How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018 INTRODUCTION Ear barotrauma (i.e. “ear block”, “ear squeeze”) is the most common complication of hyperbaric treatment. It occurs when the pressure in the hyperbaric chamber is greater than the pressure in the middle ear. It is prevented by patient assessment, patient education, and the appropriate actions of the chamber operator. The chamber operator has an important role in preventing ear barotrauma in hyperbaric patients. OBJECTIVES At the conclusion of this article, the reader will be able to: Describe the anatomy of the middle ear Explain the mechanism of ear barotrauma Describe 3 techniques to equalize middle ear pressure ANATOMY OF THE MIDDLE EAR The middle ear is an air space that separates the external ear canal from the inner ear. The eardrum, called the tympanic membrane (TM), vibrates when sound enters the ear canal. The vibration is transmitted to a series of bones in the middle ear. These bones transmit vibration to another membrane (the oval window) that separates the air‐filled middle ear from the fluid‐filled inner ear, where sound is sensed in the cochlea. The nasopharynx is the area behind the nose and above the palate. The Eustachian tubes open into this area. Because of the location of the Eustachian tube openings, the same things that cause nasal congestion (e.g. allergies, upper respiratory infection) can cause swelling around the opening of the Eustachian tubes, making it more difficult to equalize pressure in the middle ear. -
22575VIC Course in Basic Oxygen Administration for First Aid
22575VIC Course in Basic Oxygen Administration for First Aid This course has been accredited under Part 4.4 of the Education and Training Reform Act 2006 Version 1 Accredited for the period: 1 January 2021 to 31 December 2025 © State of Victoria (Department of Education and Training) 2021. Copyright of this material is reserved to the Crown in the right of the State of Victoria. This work is licensed under a Creative Commons Attribution-NoDerivs 3.0 Australia licence (see Creative Commons for more information). You are free use, copy and distribute to anyone in its original form as long as you attribute Department of Education and Training as the author, and you license any derivative work you make available under the same licence. Disclaimer In compiling the information contained in and accessed through this resource, the Department of Education and Training (DET) has used its best endeavours to ensure that the information is correct and current at the time of publication but takes no responsibility for any error, omission or defect therein. To the extent permitted by law, DET, its employees, agents and consultants exclude all liability for any loss or damage (including indirect, special or consequential loss or damage) arising from the use of, or reliance on the information contained herein, whether caused or not by any negligent act or omission. If any law prohibits the exclusion of such liability, DET limits its liability to the extent permitted by law, for the resupply of the information. Third party sites This resource may contain links to third party websites and resources. -

Hypothermia and Respiratory Heat Loss While Scuba Diving
HYPOTHERMIA AND RESPIRATORY HEAT LOSS WHILE SCUBA DIVING Kateřina Kozáková Faculty of Physical Education and Sport, Charles University in Prague, Department of Biomedical Labo- ratory Abstract One of the factors affecting length of stay under water of a diver is heat comfort. During scuba diving there is an increased risk of hypothermia. Hypothermia is one of the most life threatening factors of a diver and significantly affects his performance. The body heat loss runs by different mechanisms. One of them is the respiratory mechanism, which is often overlooked. Compressed dry air or other media is coming out from the cylinder, which have to be heated and humidified to a suitable value. Thus the organism loses body heat and consequently energy. Based on literature search the article will describe safe dive time in terms of hypo- thermia in connection to respiratory heat loss. Key words: hypothermia, heat loss, respiration, scuba diving, water environment Souhrn Jedním z faktorů ovlivňujících délku pobytu potápěče pod vodou je tepelný komfort. Během výkonu přístro- jového potápění hrozí zvýšené riziko hypotermie. Hypotermie představuje jedno z nejzávažnějších ohrožení života potápěče a zásadně ovlivňuje jeho výkon. Ke ztrátám tělesného tepla dochází různými mechanismy. Jednou cestou tepelných ztrát je ztráta tepla dýcháním, která je často opomíjená. Z potápěčského přístroje vychází suchý stlačený vzduch nebo jiné médium, který je třeba při dýchání ohřát a zvlhčit na potřebnou hodnotu. Tím organismus ztrácí tělesné teplo a potažmo energii. Tento článek, na základě literární rešerše, popíše bezpečnou dobou ponoru z hlediska hypotermie a v souvislosti se ztrátou tepla dýcháním. Klíčová slova: hypotermie, ztráta tepla, dýchání, přístrojové potápění, vodní prostředí Introduction amount of body heat. -
Guidance for Divers on Medical Certificates of Fitness to Dive
Guidance for Divers on Medical Certificates of Fitness to Dive Guidance for Divers on Medical Certificates Our Vision: of Fitness to Dive Healthy, safe and productive lives and enterprises May 2019 Cyan 100% Magenta 76% Yellow 0 Black 27% Guidance for Divers on TABLE OF CONTENTS Medical Certificates of Fitness to Dive May 2019 1.0 Introduction .............................................................................2 2.0 Legal Requirements .....................................................................3 3.0 Procedure for Applying for a Medical.....................................................5 4.0 Criteria for Conducting Medicals ........................................................ 6 5.0 Frequency of Medical Assessments, Conditions and Limitations......................... 7 Appendix 1 - Medical Questionnaire .......................................................... 8 Published in November 2019 by the Health and Safety Authority, The Metropolitan Building, James Joyce Street, Dublin 1. ©All rights reserved. r fo Guidance ers on on ers Div es tificat r Ce Medical 1.0 INTRODUCTION e Div to Fitness of May 2019 May 1.1 Under the Safety, Health and Welfare at Work (Diving) Regulations 2018 and 2019 (S.I. No. 254 of 2018 as amended by S.I. No. 180 of 2019), hereafter referred to as the Diving Regulations, a diver must not dive in a diving project unless they hold a valid certificate of medical fitness to dive issued by a medical examiner of divers. These guidelines provide information on the process and the certificates. The guidelines are aimed at divers who dive for work purposes, but the information will also be of interest to diving contractors and diving supervisors. 1.2 Working underwater can be a hostile work environment so fitness to dive is vital. It is important that the diver does not suffer from any medical condition that could affect the safety of themselves or other members of the dive team. -

Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St
Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St. Louis, Missouri LINDA DECKERT, MA, CCC-SLP, Special School District of St. Louis County, Town & Country, Missouri Vocal cord dysfunction involves inappropriate vocal cord motion that produces partial airway obstruction. Patients may present with respiratory distress that is often mistakenly diagnosed as asthma. Exercise, psychological conditions, airborne irritants, rhinosinusitis, gastroesophageal reflux disease, or use of certain medications may trigger vocal cord dysfunction. The differential diagnosis includes asthma, angioedema, vocal cord tumors, and vocal cord paralysis. Pulmo- nary function testing with a flow-volume loop and flexible laryngoscopy are valuable diagnostic tests for confirming vocal cord dysfunction. Treatment of acute episodes includes reassurance, breathing instruction, and use of a helium and oxygen mixture (heliox). Long-term manage- ment strategies include treatment for symptom triggers and speech therapy. (Am Fam Physician. 2010;81(2):156-159, 160. Copyright © 2010 American Academy of Family Physicians.) ▲ Patient information: ocal cord dysfunction is a syn- been previously diagnosed with asthma.8 A handout on vocal cord drome in which inappropriate Most patients with vocal cord dysfunction dysfunction, written by the authors of this article, is vocal cord motion produces par- have intermittent and relatively mild symp- provided on page 160. tial airway obstruction, leading toms, although some patients may have pro- toV subjective respiratory distress. When a per- longed and severe symptoms. son breathes normally, the vocal cords move Laryngospasm, a subtype of vocal cord away from the midline during inspiration and dysfunction, is a brief involuntary spasm of only slightly toward the midline during expi- the vocal cords that often produces aphonia ration.1 However, in patients with vocal cord and acute respiratory distress. -

Full Text (PDF)
REVIEW COPD Physiological and clinical relevance of exercise ventilatory efficiency in COPD J. Alberto Neder1, Danilo C. Berton1,2, Flavio F. Arbex3, Maria Clara Alencar4, Alcides Rocha3, Priscila A. Sperandio3, Paolo Palange5 and Denis E. O’Donnell1 Affiliations: 1Respiratory Investigation Unit and Laboratory of Clinical Exercise Physiology, Queen’s University and Kingston General Hospital, Kingston, ON, Canada. 2Division of Respiratory Medicine, Federal University of Rio Grande do Sul, Porto Alegre, Brazil. 3Pulmonary Function and Clinical Exercise Physiology, Respiratory Division, Federal University of Sao Paulo, Sao Paulo, Brazil. 4Division of Cardiology, Federal University of Minas Gerais, Belo Horizonte, Brazil. 5Dept of Public Health and Infectious Diseases, Sapienza University of Rome, Rome, Italy. Correspondence: J. Alberto Neder, 102 Stuart Street, Kingston, Ontario, Canada K7L 2V6. E-mail: [email protected] @ERSpublications Ventilatory efficiency is a key measurement for the interpretation of cardiopulmonary exercise testing in COPD http://ow.ly/1nsY307pbz8 Cite this article as: Neder JA, Berton DC, Arbex FF, et al. Physiological and clinical relevance of exercise ventilatory efficiency in COPD. Eur Respir J 2017; 49: 1602036 [https://doi.org/10.1183/13993003.02036- 2016]. ABSTRACT Exercise ventilation (V′E) relative to carbon dioxide output (V′CO2) is particularly relevant to patients limited by the respiratory system, e.g. those with chronic obstructive pulmonary disease (COPD). ′ − ′ High V E V CO2 (poor ventilatory efficiency) has been found to be a key physiological abnormality in symptomatic patients with largely preserved forced expiratory volume in 1 s (FEV1). Establishing an ′ − ′ association between high V E V CO2 and exertional dyspnoea in mild COPD provides evidence that exercise intolerance is not a mere consequence of detraining. -

Public Safety Scuba Diving
Industry Guide 47 A Guide to Public Safety Diving N.C. Department of Labor Occupational Safety and Health Division N.C. Department of Labor 1101 Mail Service Center Raleigh, NC 27699-1101 Cherie Berry Commissioner of Labor N.C. Department of Labor Occupational Safety and Health Program Cherie Berry Commissioner of Labor OSHA State Plan Designee Kevin Beauregard Deputy Commissioner for Safety and Health Scott Mabry Assistant Deputy Commissioner for Safety and Health Tom Savage Standards Officer Author Acknowledgments A Guide to Public Safety Diving has been prepared with materials and information from the General Industry Standards, 29 CFR 1910, Subpart T—Commercial Diving Operations, and OSHA Instruction CPL 02-00-151 (U.S. Department of Labor, Occupational Safety and Health Administration). This guide also contains information from sources such as U.S. Navy Diving Manual, National Association of Search and Rescue, California Department Fish and Game Diving Safety Manual, and the National Fire Protection Association, NFPA 1670—Standard on Operations and Technical Search and Rescue. Through an existing alliance established between the N.C. Department of Labor’s Occupational Safety and Health Divi- sion and the North Carolina Public Safety Divers’ Association (PSDA), a collaborative effort was established to make this guide possible. The PSDA board of directors provided expertise involving public safety diving in sharing best practices and technical knowledge. A special thanks to Chuck Elgin, North Carolina Underwater Response Team, for his dedication and hard work assisting in the development of this publication. This guide is intended to be consistent with all existing OSHA standards; therefore, if an area is considered by the reader to be inconsistent with a standard, then the OSHA standard should be followed. -

Critical Care in the Monoplace Hyperbaric Chamber
Critical Care in the Monoplace Hyperbaric Critical Care - Monoplace Chamber • 30 minutes, so only key points • Highly suggest critical care medicine is involved • Pitfalls Lindell K. Weaver, MD Intermountain Medical Center Murray, Utah, and • Ventilator and IV issues LDS Hospital Salt Lake City, Utah Key points Critical Care in the Monoplace Chamber • Weaver LK. Operational Use and Patient Care in the Monoplace Chamber. In: • Staff must be certified and experienced Resp Care Clinics of N Am-Hyperbaric Medicine, Part I. Moon R, McIntyre N, eds. Philadelphia, W.B. Saunders Company, March, 1999: 51-92 in CCM • Weaver LK. The treatment of critically ill patients with hyperbaric oxygen therapy. In: Brent J, Wallace KL, Burkhart KK, Phillips SD, and Donovan JW, • Proximity to CCM services (ed). Critical care toxicology: diagnosis and management of the critically poisoned patient. Philadelphia: Elsevier Mosby; 2005:181-187. • Must have study patient in chamber • Weaver, LK. Critical care of patients needing hyperbaric oxygen. In: Thom SR and Neuman T, (ed). The physiology and medicine of hyperbaric oxygen therapy. quickly Philadelphia: Saunders/Elsevier, 2008:117-129. • Weaver LK. Management of critically ill patients in the monoplace hyperbaric chamber. In: Whelan HT, Kindwall E., Hyperbaric Medicine Practice, 4th ed.. • CCM equipment North Palm Beach, Florida: Best, Inc. 2017; 65-95. • Without certain modifications, treating • Gossett WA, Rockswold GL, Rockswold SB, Adkinson CD, Bergman TA, Quickel RR. The safe treatment, monitoring and management -

The Use of Heliox in Treating Decompression Illness
The Diving Medical Advisory Committee DMAC, Eighth Floor, 52 Grosvenor Gardens, London SW1W 0AU, UK www.dmac-diving.org Tel: +44 (0) 20 7824 5520 [email protected] The Use of Heliox in Treating Decompression Illness DMAC 23 Rev. 1 – June 2014 Supersedes DMAC 23, which is now withdrawn There are many ways of treating decompression illness (DCI) at increased pressure. In the past 20 years, much has been published on the use of oxygen and helium/oxygen mixtures at different depths. There is, however, a paucity of carefully designed scientific studies. Most information is available from mathematical models, animal experiments and case reports. During a therapeutic compression, the use of a different inert gas from that breathed during the dive may facilitate bubble resolution. Gas diffusivity and solubility in blood and tissue is expected to play a complex role in bubble growth and shrinkage. Mathematical models, supported by some animal studies, suggest that breathing a heliox gas mixture during recompression could be beneficial for nitrogen elimination after air dives. In humans, diving to 50 msw, with air or nitrox, almost all cases of DCI can be adequately treated at 2.8 bar (18 msw), where 100% oxygen is both safe and effective. Serious neurological and vestibular DCI with only partial improvements during initial compression at 18 msw on oxygen may benefit from further recompression to 30 msw with heliox 50:50 (Comex therapeutic table 30 – CX30). There have been cases successfully treated on 50:50 heliox (CX30), on the US Navy recompression tables with 80:20 and 60:40 heliox (USN treatment table 6A) instead of air and in heliox saturation. -

Title: Drowning and Therapeutic Hypothermia: Dead Man Walking
Title: Drowning and Therapeutic Hypothermia: Dead Man Walking Author(s): Angela Kavenaugh, D.O., Jamie Cohen, D.O., Jennifer Davis MD FAAP, Department of PICU Affiliation(s): Chris Evert Children’s Hospital, Broward Health Medical Center ABSTRACT BODY: Background: Drowning is the second leading cause of death in children and is associated with severe morbidity and mortality, most often due to hypoxic-ischemic encephalopathy. Those that survive are often left with debilitating neurological deficits. Therapeutic Hypothermia after resuscitation from ventricular fibrillation or pulseless ventricular tachycardia induced cardiac arrest is the standard of care in adults and has also been proven to have beneficial effects that persist into early childhood when utilized in neonatal birth asphyxia, but has yet to be accepted into practice for pediatrics. Objective: To present supportive evidence that Therapeutic Hypothermia improves mortality and morbidity specifically for pediatric post drowning patients. Case Report: A five year old male presented to the Emergency Department after pool submersion of unknown duration. He was found to have asphyxial cardiac arrest and received bystander CPR, which was continued by EMS for a total of 10 minutes, including 2 doses of epinephrine. CPR continued into the emergency department. Upon presentation to the ED, he was found to have fixed and dilated pupils, unresponsiveness, with a GCS of 3. Upon initial pulse check was found to have return of spontaneous circulation, with sinus tachycardia. His blood gas revealed 6.86/45/477/8/-25. He was intubated, given 2 normal saline boluses and 2 mEq/kg of Sodium Bicarbonate. The initial head CT was normal. -

Drift Diver Program #RST.010
Course Overview Drift Diver Program #RST.010 Drift diving allows the diver to cover a large expanse of water during a dive, and makes diving where currents are present much more enjoyable. This course is designed to be an introduction to drift diving and to help the student diver develop the skills, knowledge and techniques necessary for safe & comfortable drift diving. Drift Diving is effortless and relaxing because you simply glide with the current and feel the rush of flying underwater. But, with this type of diving come special procedures that you need to know so you can maximize your fun underwater. From equipment requirements to dive planning, we’ll cover all the aspects of drift diving during this course. During your PADI Drift Diver certification course, you’ll learn about drift dive planning, organization, techniques and potential hazards, as well as special equipment and procedures like buoyancy. But it’s not all theory because you’ll go on two open water dives where you can put your new knowledge into action. You may count this Specialty certification toward one of the five required Specialties for the Master Scuba Diver certification. Agency Certification Required Student Equipment PADI Basic Scuba Set-up Lift bag with finger spool Course Name & Certification Issued Drift Diver Administrative Items Medical Statement Student Prerequisite(s) Liability Release Form PADI (Jr.) Adventure Diver -or- equivalent Required Student Materials Minimum Age None 12 Materials included in Course Fee Class Session(s) (hours) PADI Drift Diver Manual 1 (1) Library Items Available? Pool Session(s) PADI Drift Diver DVD optional Class Start Dates Open Water Dives See Class Schedule for Dates 2 Minimum/Maximum Depths 130 ft.