Simple Heart Cure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Norman Conquest: the Style and Legacy of All in the Family
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Boston University Institutional Repository (OpenBU) Boston University OpenBU http://open.bu.edu Theses & Dissertations Boston University Theses & Dissertations 2016 The Norman conquest: the style and legacy of All in the Family https://hdl.handle.net/2144/17119 Boston University BOSTON UNIVERSITY COLLEGE OF COMMUNICATION Thesis THE NORMAN CONQUEST: THE STYLE AND LEGACY OF ALL IN THE FAMILY by BAILEY FRANCES LIZOTTE B.A., Emerson College, 2013 Submitted in partial fulfillment of the requirements for the degree of Master of Fine Arts 2016 © 2016 by BAILEY FRANCES LIZOTTE All rights reserved Approved by First Reader ___________________________________________________ Deborah L. Jaramillo, Ph.D. Assistant Professor of Film and Television Second Reader ___________________________________________________ Michael Loman Professor of Television DEDICATION This thesis is dedicated to Jean Lizotte, Nicholas Clark, and Alvin Delpino. iv ACKNOWLEDGMENTS First, I’m exceedingly thankful for the guidance and patience of my thesis advisor, Dr. Deborah Jaramillo, whose investment and dedication to this project allowed me to explore a topic close to my heart. I am also grateful for the guidance of my second reader, Michael Loman, whose professional experience and insight proved invaluable to my work. Additionally, I am indebted to all of the professors in the Film and Television Studies program who have facilitated my growth as a viewer and a scholar, especially Ray Carney, Charles Warren, Roy Grundmann, and John Bernstein. Thank you to David Kociemba, whose advice and encouragement has been greatly appreciated throughout this entire process. A special thank you to my fellow graduate students, especially Sarah Crane, Dani Franco, Jess Lajoie, Victoria Quamme, and Sophie Summergrad. -
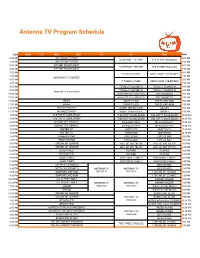
Antenna TV Program Schedule
Antenna TV Program Schedule East MON TUE WED THU FRI SAT SUN West 5:00 AM BACHELOR FATHER 2:00 AM SUSPENSE THEATRE THE THREE STOOGES 5:30 AM BACHELOR FATHER 2:30 AM 6:00 AM FATHER KNOWS BEST 3:00 AM SUSPENSE THEATRE THE THREE STOOGES 6:30 AM FATHER KNOWS BEST 3:30 AM 7:00 AM 4:00 AM IT TAKES A THIEF HERE COME THE BRIDES 7:30 AM 4:30 AM ANTENNA TV THEATER 8:00 AM 5:00 AM IT TAKES A THIEF HERE COME THE BRIDES 8:30 AM 5:30 AM 9:00 AM TOTALLY TOONED IN TOTALLY TOONED IN 6:00 AM 9:30 AM TOTALLY TOONED IN TOTALLY TOONED IN 6:30 AM ANTENNA TV THEATER 10:00 AM ANIMAL RESCUE CLASSICS (E/I) THE MONKEES 7:00 AM 10:30 AM ANIMAL RESCUE CLASSICS (E/I) THE MONKEES 7:30 AM 11:00 AM HAZEL SWAP TV (E/I) THE FLYING NUN 8:00 AM 11:30 AM HAZEL SWAP TV (E/I) THE FLYING NUN 8:30 AM 12:00 PM MCHALE'S NAVY WORD TRAVELS (E/I) GIDGET 9:00 AM 12:30 PM MCHALE'S NAVY WORD TRAVELS (E/I) GIDGET 9:30 AM 1:00 PM THE PATTY DUKE SHOW THE PATTY DUKE SHOW THE PATTY DUKE SHOW 10:00 AM 1:30 PM THE PATTY DUKE SHOW THE PATTY DUKE SHOW THE PATTY DUKE SHOW 10:30 AM 2:00 PM DENNIS THE MENACE MCHALE'S NAVY MCHALE'S NAVY 11:00 AM 2:30 PM DENNIS THE MENACE MCHALE'S NAVY MCHALE'S NAVY 11:30 AM 3:00 PM MISTER ED MISTER ED MISTER ED 12:00 PM 3:30 PM MISTER ED MISTER ED MISTER ED 12:30 PM 4:00 PM GREEN ACRES CIRCUS BOY CIRCUS BOY 1:00 PM 4:30 PM GREEN ACRES CIRCUS BOY CIRCUS BOY 1:30 PM 5:00 PM I DREAM OF JEANNIE ADV. -

LGBTQ Episodic Television Study Guide
Archive Study Guide: LESBIAN, GAY, BISEXUAL AND TRANSGENDER TELEVISION: SITCOMS AND EPISODIC DRAMAS ARCHIVE STUDY GUIDE The representation of Lesbian, Gay, Bisexual and Transgender (LGBT) communities on television is marked by a history of stereotypes and inexplicable invisibility. By the 1970s, gay media-watch groups communicated their concerns to the television industry and a sense of cooperation began to emerge between the LG BT community and broadcasters. During the 1980s, the AIDS crisis and resulting prejudices ushered in a new era of problematic and offensive portrayals. In the late 1990s, Ellen Degeneres' landmark coming out, (both in real- life, and through the character she portrayed in her sitcom), generated much controversy and discussion, ultimately paving the way for well -developed gay characters in prominent primetime TV roles. Despite such advances, stereotypes continue to resurface and perpetuate, and the full diversity of the LGBT community is more often than not underrepresented in the mass media. This is only a partial list – consult the Archive Research and Study Center for additional titles, including relevant materials held in the Outfest Legacy Collection. HEARST NEWSREEL Hearst Newsreel Footage. Movie Stars Join Circus for Charity! Los Angeles, California (1948-09-04). Wrestling telecasts of the late 1940s and early 1950s often featured flamboyant characters with (implied) gay personas. Features Bob Hope acting as manager of outlandish TV wrestler Gorgeous George, who faces actor Burt Lancaster in a match. Study Copy: VA6581 M Hearst Newsreel Footage. Wrestling from Montreal, Quebec, Canada (1948-10-22). Gorgeous George vs. Pete Petersen. Study Copy: VA8312 M TELEVISION (Please note some titles may require additional lead-time to make available for viewing) 1950s Western Main Event Wrestling. -
Incidental Social Learning Among Black and White Viewers in Relation to Luthorit Rian S Characterizations in Pripe-Rise Ntertaiiment
DOCUMENT RESUME. ED 122 279 CS 202 O84 AUTHOR Leckenby, John .D.'; Su'rlin Stuart 0. : 'TITLE incidental Social Learning Among Black and White Viewers in Relation to luthorit rian s Characterizations in Pripe-rise ntertaiiment . Programmidg. PUB DATE 75 4 NOTE 25p.: Paper presedted at th nnual Meeting of the Association for Education in Journalism (Ottawa, Ontario, August 1975) 0 'EDRS PRICt 3?-$0.83 5C$1.67 Plus Postage DESCiIPTORS Adult Learning; *Authoritarianism; Caucasian Race; *Incidental Learning; sass Media; Negro Attitudes; Observational Learning; *Racial Attitudes; Social ittitudes; Social ?actors; Social Influences; *Social Values; Television Research; Television Shrveys; *Television Viewing IDENTIFIERS All in the Family; Sanford and Son ABSTRACT The nature of incidental social learning in 'television viewers in the Fasily" and "Sanford and Son" was the focus of this invLigation. Seven hundred and eight-one racially and'econosically AO-Zed respondents fro. Chicago and Atlanta provided the data source. Telephone interviews attempted ta-assess viewer opinions of the reality of characters po rayed and racial' attitudes assumed, entertainment value of the progTa sing, and presende of a moral lesson. Frequency of viewing, identi ication with a.specific character, and levels of cultural estrang sent, powerlessness, and meaninglessness Were also assessed.:Pindin ggest that high frequency viewers of both programs find the programming t b t . entertaining and revealing of actual behavior of the-gro s 'portrayed. These individuals are inclined to agree with the authoritarian views of the major characters in the two prograps4 ,"Fred" and "Archie." In addition, a'high correlation existed between high4frequency viewing and viewer self-perception of alienation and estrangement from the outside world. -

"Introduction: Survey of Literature of "All in The
6 "INTRODUCTION: SURVEY OF LITERATURE OF "ALL IN THE FAMILY" Mike Porter On the night of January 12, 1971 a group of men sat watching a monitor in the CBS executive suite in New York. Some were optjmistic but all were nervous as careers lay on the line. Meanwhile, a continent away, another gentleman was "pacing the floor of a viewing room in Television City, 1 Hollywood, like an expectant father." It was too late for anyone to change their minds--the point of no return had been reached. At 10:30 p.m. EST, these men looked on as a new mid-season replacement program was fed down the lines to awaiting and warned affiliates nationwide. Meanwhile, in every major television market, extra operators hired by the network prepared themselves for the expected tempest of an enraged American public. As was later recalled, these men "kind of sneaked it on 2 one night with no advance advertising or anything." As the show began with its now familiar theme song--American entered into what was later described as "a new era of candor. The name of the program was "All in the Family." Without a doubt, "All in the Family" is one of the most controversial yet successful series in the history The show about Archie Bunker, his wife Edith, his daughter Gloria and his son-in-law the "Meathead," became what one 7 4 observer called "instant American folklore." Indeed that observation became true since in 1978 Archie Bunker's famous chair was installed as an exhibit at the Smithsonian Institution. -

February 21, 2007
FOR IMMEDIATE RELEASE Contact: Geoffrey Baum 213-821-1491 USC Establishes Norman Lear Chair in Entertainment, Media and Society Martin Kaplan to hold Endowed Chair at USC Annenberg School LOS ANGELES, February 21, 2007 – Norman Lear, the pioneering television and film producer, political and social activist and philanthropist is being honored by the University of Southern California with the establishment of the Norman Lear Chair in Entertainment, Media and Society, Geoffrey Cowan, dean of the USC Annenberg School for Communication announced today. The inaugural holder of the Norman Lear Chair is Martin Kaplan, founding director of the Norman Lear Center at the USC Annenberg School. Kaplan, an Annenberg Research Professor, has been associate dean of the School since 1997. “I view few things as more important to the health of our culture as Martin Kaplan’s work leading the Center that exists in my name at the USC Annenberg School,” said Lear. “I could not be more honored that Mr. Kaplan has additionally agreed to occupy a Chair in my name – so honored, that I would be happy to surround his Chair with a roomful of furniture, piano included, were the Annenberg School to allow.” “USC’s decision to create and name this chair is a wonderful tribute to Norman’s commitment to USC Annenberg and the work of the Lear Center,” said Cowan, who noted that, other than the Annenberg family, Lear is the largest donor to the USC Annenberg School. In addition to $11 million from Mr. Lear—which includes a new $6 million pledge—the Lear Center has garnered more than $9 million in gifts and research grants from foundation, government and other sources. -

COIOR Advice
g £ - l^C H E ST E R HERALD. Wed,, March 2, 1983 Canoe race Virginity still good buy in love marketplace DEAR ABBY: Many letters in your choose not to risk falling into that habit Now, at age 48 I find that I am much column have touched me, but none until I have found the person with more passiohate thfin I was when I was Keiinedy Is warned: Boy meets girl: Text of ruling set April 10 moved me as much as the one from whom I can establish an exclusive a 23-year-oU- virgin. I was able to "Holding Out and Proud Out of It.” Dear lifelong commitment. exercise control back then. (I didn’t New twist at MMH In Coventry Horray for her! And horray for you know what I was missing.) Be thinking of cuts By Alex GIrelli for printing it. More people need to Please don’t think I'm an oddball. Herald City Fdltn- know that there are still some women Abby I’m not. I’m just saving myself for the As immature as this my sound. I’m ... page 3 ... page 11 page 9 The seventli annual Hockanum River Canoe around who don’t jump into bed with Abigail person I marry. And in case you’re not sure that I willbe able to exercise every John, Mick and Murray, I know I wondering — I’m straight, and I’ll be 38 Race, an event that attacts an average of 100 Van Buren that control that control now, so I just competitors, has been scheduled for April 10, have lots of guys because I wouldnt my next birthday. -

BUSINESS Junior High and High Schooi Students Ex-Comic’S Help Drops Spells Success Bv Denis G
to - MANCHESTER HERALD. Thursduy, March 22, 1984 Busy summer likely for vacation industry Conventioneers and most Organized tours woh't provide them. Forget additional $7 execution fee. If you hove to pay onty^S,' Reaction to rape verdict hlartford protesters We are now entering the busiest summer ever for about discount air fares: the m ajor carriers serving you can mail in your application. ~ ‘ the vacation industry — with a variety of forces Los Angeles have stopped them for the weeks Moreover, since 1981, every individual, even an lire. Portuguese defendants take over Colt dome slated by GOP combining to push vacation travel to all-time highs. surrounding the games. infant, is required to have a passport issued in his ® The U.S. dollar is strong, tempting us to go abroad to Y o u t If your plans include foreign travel, you have no her own name. Children under age 18 are still issued tour and buy bargains; the Summer Olympic Games time to fiddle, either. Check whether your passport is five-year passports, at a cost of $27. page 2 ... page 10 .. page 3 will open in Los Angeles, pulling us to the West Coast Money's current and il not, submit an application promptly. Many countries require a visa before you can enteE. by the hundreds of thousands. Economic expansion is The State Department does its best to send your For some countries, you must submit your passpoit assured through this summer at least, encouraging us Worth passport within a short time. You will assist by filling with yoiir visa application before your departure.' to open our pocketbooks and wallets to spend. -

Fall 2020 RTF 359S: Black Television Comedy-WB Course Instructor
Fall 2020 RTF 359S: Black Television Comedy-WB Course Instructor: Adrien Sebro Email: [email protected] Seminar Day and Time: Tuesday and Thursday 9:30AM-11:00AM Office Hours: Tuesday 12:00PM-1PM or by appointment Teaching Assistant: Email: Office Hours: By appointment Course Description: For cultural critics to ignore television’s potential as a Forum of resistance is to misread levels of vernacular meaning inherent in many Black television texts. Often viewed as a medium of bufFoonery or harsh stereotyping, situational comedies that Focus on Black communities have in fact had a crucial role in political progress, activism, and evolving social conditions in the United States. With close attention to themes such as socioeconomics, gender, religion, and politics, Black sitcoms address American social injustices in ways that other sitcoms simply are unable to. This course will chronicle a history of American Black sitcoms over time, that worked to respond to their political moment and have radically transFormed television as a space For pedagogy. It is important to mention, that this course’s Focus on the sitcom genre is deliberate. The sitcom can be read to help lay bare the mores, images, ideals, prejudices, and ideologies in its topical moment. There is much history that can and must be captured From the sitcom. As Darrell Hamamoto states, “the study of the television situation comedy is an exercise in examining the relationship of popular art to its historically speciFic setting.” Surveying histories of television sitcoms in general ofFers a unique history of what is understood as national American humor. American humor in general, and Black humor speciFically, began as a “wrested Freedom,” the Freedom to laugh at that which was unjust and cruel in order to create distance From what would otherwise obliterate a sense of selF and community. -

1 Introduction Beginning in the Early 1970S, a Shift Occurred in the World
1 Introduction Beginning in the early 1970s, a shift occurred in the world of television comedy. New network executives came in and decided to change the content that was being put on the air. The popular TV shows of the 1960s were based in fantasy and did not address any relevant issues. Programs like Bewitched, I Dream of Jeannie, Green Acres and Petticoat Junction were some of the highest rated shows of the decade. The reasons for these show’s success are many. One being they appealed to audiences young and old. Television had become cheap enough to be nearly ubiquitous in the U.S. and therefore a family activity. Also, commercial sponsors were and continue to be the loudest voice in determining a program’s content, and wanted to attract the largest audience possible. “And let’s face it, if you’re a salesman and your goal is to sell as many cans of dog food or tubes of toothpaste as you possibly can, the last thing you want to do is offend any potential customers.” 1 After the Communist threat or “red scare” became a lesser issue in the late 1960s, networks felt as though they could depart from traditional, antiquated values and address real societal issues. However, producers and network executives felt as though the best way to portray these issues was through the situation comedy genre. Early sitcoms like The Mary Tyler Moore Show, All in the Family, Maude and Soap all tackled issues that were extremely relevant in the lives of many Americans as well as in the greater American culture. -

In the History of American Primetime Television, Very Few Programs, If Any
“T HOSE WERE THE DAYS …”: ALL IN THE FAMILY AND THE ‘P RIMETIMING ’ OF U.S. DIVERSITY AND COUNTERCULTURE Dennis TREDY Université Paris III – Sorbonne Nouvelle In the history of American primetime television, very few programs, if any, have had as startling and as permanent effect on the television landscape or have broken as many barriers as Norman Lear’s All in the Family . The program, along with the spin-offs and lookalikes spurred by it throughout the early 1970’s, brought long overdue change to the American identity that network television chose to reflect, finally bringing civil strife and intergenerational conflicts regarding race, equal rights for women and minorities, anti-war sentiment and youth culture into America’s living rooms and thereby into the forefront of public discourse. Lear’s go-for-the-jugular approach to dealing with the most divisive and politically incorrect social issues is indeed legendary, as he cleverly used the Trojan horse of laughter to deliver hard truths, and as he understood that America’s deep-seated problems had to be dealt with head-on if they were ever to be overcome—so as to root out the evil, as it were, so that the country could heal. In order to appreciate the true impact that this ground-breaking CBS sitcom had on the television landscape, it is essential to first understand just how “out of touch” the television landscape of the late 1960’s was, the laughably meager steps that had been taken to touch on themes of diversity and counterculture, and the confluence of circumstances that made such a radical change even imaginable, let alone possible. -

Beryl Vertue
The unwitting pioneer of transatlantic format adaptation: Beryl Vertue Article Accepted Version Knox, S. (2019) The unwitting pioneer of transatlantic format adaptation: Beryl Vertue. Historical Journal of Film, Radio and Television, 39 (2). pp. 341-365. ISSN 0143-9685 doi: https://doi.org/10.1080/01439685.2018.1522790 Available at http://centaur.reading.ac.uk/77128/ It is advisable to refer to the publisher’s version if you intend to cite from the work. See Guidance on citing . To link to this article DOI: http://dx.doi.org/10.1080/01439685.2018.1522790 Publisher: Taylor & Francis All outputs in CentAUR are protected by Intellectual Property Rights law, including copyright law. Copyright and IPR is retained by the creators or other copyright holders. Terms and conditions for use of this material are defined in the End User Agreement . www.reading.ac.uk/centaur CentAUR Central Archive at the University of Reading Reading’s research outputs online THE UNWITTING PIONEER OF TRANSATLANTIC FORMAT ADAPTATION: BERYL VERTUE Simone Knox, University of Reading Postal address: University of Reading Department of Film, Theatre & Television Minghella Studios Shinfield Road Reading, Berkshire RG6 6BT. Telephone number: 01183784076 Email address: [email protected] Biographical note: Dr Simone Knox is Lecturer in Film and Television at the University of Reading. Her research interests include the transnationalisation of film and television (including audio-visual translation), aesthetics and medium specificity (including convergence culture, and acting and performance), and representations of minority identities, as well as the lived experience of screen culture. She sits on the board of editors for Critical Studies in Television and her publications include essays in Film Criticism, Journal of Popular Film and Television and New Review of Film and Television Studies, as well as the co-authored blog strand ‘What Actors Do’ for CSTOnline.