Maternal and Neonatal Health in Select Districts of Iraq: Findings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rebooting U.S. Security Cooperation in Iraq
Rebooting U.S. Security Cooperation in Iraq MICHAEL KNIGHTS POLICY FOCUS 137 Rebooting U.S. Security Cooperation in Iraq MICHAEL KNIGHTS THE WASHINGTON INSTITUTE FOR NEAR EAST POLICY www.washingtoninstitute.org The opinions expressed in this Policy Focus are those of the author and not necessarily those of The Washington Institute, its Board of Trustees, or its Board of Advisors. All rights reserved. Printed in the United States of America. No part of this publica- tion may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publisher. © 2015 by The Washington Institute for Near East Policy The Washington Institute for Near East Policy 1828 L Street NW, Suite 1050 Washington, DC 20036 Design: 1000colors Photo: A Kurdish fighter keeps guard while overlooking positions of Islamic State mili- tants near Mosul, northern Iraq, August 2014. (REUTERS/Youssef Boudlal) CONTENTS Acknowledgments | v Acronyms | vi Executive Summary | viii 1 Introduction | 1 2 Federal Government Security Forces in Iraq | 6 3 Security Forces in Iraqi Kurdistan | 26 4 Optimizing U.S. Security Cooperation in Iraq | 39 5 Issues and Options for U.S. Policymakers | 48 About the Author | 74 TABLES 1 Effective Combat Manpower of Iraq Security Forces | 8 2 Assessment of ISF and Kurdish Forces as Security Cooperation Partners | 43 FIGURES 1 ISF Brigade Order of Battle, January 2015 | 10 2 Kurdish Brigade Order of Battle, January 2015 | 28 ACKNOWLEDGMENTS My thanks to a range of colleagues for their encouragement and assistance in the writing of this study. -
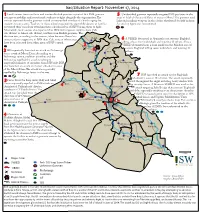
2014-11-17 Situation Report
Iraq Situation Report: November 17, 2014 1 Local sources from southern and western Kirkuk province reported that ISIS gunmen 5 Unidentied gunmen reportedly targeted ISIS positions in the attempt to mobilize and recruit male students to ght alongside the organization. e areas of Islah al-Zerai and Refai of western Mosul. e gunmen used sources reported that the gunmen visited an unspecied number of schools urging the light and medium weapons in the clashes that lasted for half an hour. students to carry arms. Teachers in these schools rejected this step while dozens of families A causality gure was not reported. prevented their sons from attending their schools in fear of ISIS forcing them to ght. Meanwhile, local sources also reported that ISIS shifted power supplies from Zab sub-district to Abassi sub-district, southwestern Kirkuk province. is decision was, according to the sources, taken because Abassi has Dahuk 6 more residents supportive of ISIS than Zab, some of whom may A VBIED detonated in Amiriyah area, western Baghdad, have been relocated from other areas of ISIS control. killing at least four individuals and injuring 13 others. Also, a Mosul2 Dam VBIED detonated near a local market in the Mashtal area of 2 5 eastern Baghdad killing seven individuals and injuring 22 ISIS reportedly launched an attack on Peshmerga Mosul Arbil others. forces south of Mosul Dam. According to a Peshmerga source, coalition airstrikes and the Peshmerga repelled the attack resulting in As Sulaymaniyah unspecied number of casualties from ISIS side. ISIS also launched an attack on Zumar sub-district, west Kirkuk of the Mosul Dam. -

Iraq Protection Cluster
Iraq Protection Cluster: Anbar Returnee Profile - March 2017 24 April 2017 Amiriyat Al- Protection Concerns Ramadi Heet Falluja/Garma Haditha Rutba Khaldiyah High Fallujah Reported Violations of principles relating to return movements (including non-discrimination in the right of return, as well as voluntariness, safety and dignity of return movements) Medium Security incidents resulting in death/injury in return area (including assault, murder, conflict-related casualties) Explosive Remnants of War (ERW)/ Improvised Explosive Device (IED) contamination in return area by District by Low Reported Rights violations by state or non-state military/security actors (including abduction, arbitrary arrest/detention, disproportionate restrictions on freedom of movement) Protection Risk Matrix Risk Protection Concerns relating to inter-communal relations and social cohesion MODM Returnee Figures Returnee Families (Registered and non-registered) District Families Falluja 53,218 Ramadi 82,242 Ramadi 51,293 Falluja/Garma 48,557 Ru'ua Heet 11,321 Heet 19,101 Haditha Haditha 3,936 Rutba 2,356 Ka'im Haditha 2,147 Heet 35,600 Baghdad 18,056 Rutba 1,825 Ana 31,299 Anbar 79,211 22,640 Anbar Displacements Erbil Ramadi 14,331 and Returns Falluja 13,341 Total Families Still Kirkuk 8,729 Displaced 12,472 Sulaymaniyah Total Families Rutba 6,500 Returned 4,440 Other 283 759 Babylon 474 IDP Information Center: 22% of calls received from Anbar were from returnees. The most popular issues flagged: 43% Governmental issues (grants, compensation on damaged properties, ..etc) 29% Cash assistance Data Sources: Disclaimer: 14% Other issues * IOM-DTM as of 30 March 2017 The boundaries and names shown and the designations used on this map * MoDM 18 April 2017 do not imply official endorsement or acceptance by the United Nations. -

Local Policing in Iraq Post-Isil
LOCAL POLICING IN IRAQ POST-ISIL CARVING OUT AN ARENA FOR COMMUNITY SERVICE? Jessica Watkins, Falah Mubarak Bardan, Abdulkareem al- Jarba, Thaer Shaker Mahmoud, Mahdi al-Delaimi, Abdulazez Abbas al-Jassem, Moataz Ismail Khalaf, Dhair Faysal Bidewi LSE Middle East Centre Paper Series | 51 | July 2021 About the Middle East Centre The Middle East Centre builds on LSE’s long engagement with the Middle East and provides a central hub for the wide range of research on the region carried out at LSE. The Middle East Centre aims to enhance un- derstanding and develop rigorous research on the societies, economies, polities and interna- tional relations of the region. The Centre pro- motes both specialised knowledge and public understanding of this crucial area and has out- standing strengths in interdisciplinary research and in regional expertise. As one of the world’s leading social science institutions, LSE com- prises departments covering all branches of the social sciences. The Middle East Centre harnesses this expertise to promote innovative research and training on the region. Middle East Centre Local Policing in Iraq Post-ISIL: Carving Out an Arena for Community Service? Jessica Watkins, Falah Mubarak Bardan, Abdulkareem al-Jarba, Thaer Shaker Mahmoud, Mahdi al-Delaimi, Abdulazez Abbas al- Jassem, Moataz Ismail Khalaf and Dhair Faysal Bidewi LSE Middle East Centre Paper Series | 51 July 2021 About the Authors Abstract Jessica Watkins is a Visiting Fellow at the Since 2003, frequent outbreaks of LSE Middle East Centre, and a Research violence in Iraq have led to a heavily mili- Associate at the German Institute for tarised local police force. -

The Case of the Iraqi Disputed Territories Declaration Submitted By
Title: Education as an Ethnic Defence Strategy: The Case of the Iraqi Disputed Territories Declaration Submitted by Kelsey Jayne Shanks to the University of Exeter as a thesis for the degree of Doctor of Philosophy in Politics, October 2013. This thesis is available for Library use on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. I certify that all material in this thesis which is not my own work has been identified and that no material has previously been submitted and approved for the award of a degree by this or any other University. Kelsey Shanks ................................................................................. 1 Abstract The oil-rich northern districts of Iraq were long considered a reflection of the country with a diversity of ethnic and religious groups; Arabs, Turkmen, Kurds, Assyrians, and Yezidi, living together and portraying Iraq’s demographic makeup. However, the Ba’ath party’s brutal policy of Arabisation in the twentieth century created a false demographic and instigated the escalation of identity politics. Consequently, the region is currently highly contested with the disputed territories consisting of 15 districts stretching across four northern governorates and curving from the Syrian to Iranian borders. The official contest over the regions administration has resulted in a tug-of-war between Baghdad and Erbil that has frequently stalled the Iraqi political system. Subsequently, across the region, minority groups have been pulled into a clash over demographic composition as each disputed districts faces ethnically defined claims. The ethnic basis to territorial claims has amplified the discourse over linguistic presence, cultural representation and minority rights; and the insecure environment, in which sectarian based attacks are frequent, has elevated debates over territorial representation to the height of ethnic survival issues. -

THE BROOKINGS INSTITUTION IRAQ at a CROSSROADS with BARHAM SALIH DEPUTY PRIME MINISTER of IRAQ Washington, D.C. Monday, October
THE BROOKINGS INSTITUTION IRAQ AT A CROSSROADS WITH BARHAM SALIH DEPUTY PRIME MINISTER OF IRAQ Washington, D.C. Monday, October 22, 2007 Introduction and Moderator: MARTIN INDYK Senior Fellow and Director, Saban Center for Middle East Policy The Brookings Institution Featured Speaker: BARHAM SALIH Deputy Prime Minister of Iraq * * * * * 2 P R O C E E D I N G S MR. INDYK: Good morning, ladies and gentlemen. Welcome to The Saban Center for Middle East Policy at the Brookings Institution. I'm Martin Indyk, the Director of the Saban Center, and it's my pleasure to introduce this dear friend, Dr. Barham Salih, to you again. I say again because, of course, Barham Salih is a well-known personality in Washington, having served here with distinction representing the patriotic Union of Kurdistan in the 1990s, and, of course, he's been a frequent visitor since he assumed his current position as Deputy Prime Minister of the Republic of Iraq. He has a very distinguished record as a representative of the PUK, and the Kurdistan regional government. He has served as Deputy Prime Minister, first in the Iraqi interim government starting in 2004, and was then successfully elected to the transitional National Assembly during the January 2005 elections and joined the transitional government as Minister of Planning. He was elected again in the elections of December 2005 to the Council of Representatives, which is the Iraqi Permanent Parliament, and was then called upon to join the Iraqi government in May 2006 as Deputy Prime Minister. Throughout this period he has had special responsibility for economic affairs. -
Who Takes the Blame the Strategic Effects of Collateral Damage
Who Takes the Blame? The Strategic Effects of Collateral Damage Luke N. Condra University of Pittsburgh Jacob N. Shapiro Princeton University Can civilians caught in civil wars reward and punish armed actors for their behavior? If so, do armed actors reap strategic benefits from treating civilians well and pay for treating them poorly? Using precise geo-coded data on violence in Iraq from 2004 through 2009, we show that both sides are punished for the collateral damage they inflict. Coalition killings of civilians predict higher levels of insurgent violence and insurgent killings predict less violence in subsequent periods. This symmetric reaction is tempered by preexisting political preferences; the anti-insurgent reaction is not present in Sunni areas, where the insurgency was most popular, and the anti-Coalition reaction is not present in mixed areas. Our findings have strong policy implications, provide support for the argument that information civilians share with government forces and their allies is a key constraint on insurgent violence, and suggest theories of intrastate violence must account for civilian agency. “When the Americans fire back, they don’t hit the of the interaction between civilians and armed actors in people who are attacking them, only the civilians. civil wars have shown that both outcomes are possible (cf. This is why Iraqis hate the Americans so much. This Stanton 2009; Valentino 2004). Attacks that harm non- is why we love the mujahedeen.”1 —Osama Ali combatants may undermine civilian support or solidify 24-year-old Iraqi it depending on the nature of the violence, the intention- ality attributed to it, and the precision with which it is “If it is accepted that the problem of defeating the applied (Downes 2007; Kalyvas 2006; Kocher, Pepinksy, enemy consists very largely of finding him, it is easy and Kalyvas 2011). -

Peace Message for Iraq Illuminates Erbil Citadel
UNAMI Newsletter United Nations Assistance Mission for Iraq Newsletter - Issue 5 September 2010 IN THIS ISSUE Peace message for Iraq illuminates Erbil Citadel Peace message for Iraq illuminates Erbil Citadel ……………………………. 1 United Nations in Iraq celebrates the International Day of Peace ………… 2 A survivor's answer to violence: help Iraqi youth build peace in Iraq ……….. 3 Championing for peace in Kirkuk, Iraq. 3 A little peace picnic …………………… 4 On the census in Iraq: Speech of DSRSG Jerzy Skuratowicz ………….. 4 The Representative of the Secretary- General on the Human Rights of Internally Displaced Persons visits Iraq …………………………………….. 5 Toward strengthening the monitoring and reporting of grave violations against children in Iraq……………….. 5 Iraq adopts UN plan to transform state The Peace Day slogan put up at the Erbil Citadel. Photo: UNAMI PIO/ Laila Shamji -owned enterprises into corporations ...…………………………. 6 s part of the world wide celebration of urgent preventive works on ten of the European Union helps improve the International Day of Peace which Citadel’s most unstable buildings. UNESCO is schools and quality of education in southern Iraq ………………………….. 6 A falls on 21 September each year, also working with national authorities in their UNAMI raised and illuminated on 19 efforts to enlist the site in the World Heritage United Nations helps tackle illiteracy in September a fluorescent sign of the 2010 List. Iraq ……………………………………… 7 peace day slogan Peace=Future: The Math is Government of Iraq approves a UNAMI collaborated closely with the offices of Easy in Erbil, Kurdistan Region of Iraq. national school feeding programme … 8 the Governor of Erbil and the High Iraq’s first National Health Accounts Scripted and illuminated in the Kurdish Commission for Erbil Citadel Revitalization in survey completed ……………………. -

Iraq SITREP 2015-5-22
Iraq Situation Report: July 07 - 08, 2015 1 On July 6, Iraqi Army (IA) and Counter-Terrorism Service (CTS) reinforcements arrived in 6 On July 6, the DoD reported one airstrike “near Baiji.” On July 7, one SVBIED Barwana sub-district, south of Haditha. On July 7, Prime Minister (PM) Abadi ordered the exploded in the Baiji Souq area in Baiji district, and two SVBIEDs exploded in the Sakak deployment of SWAT reinforcements to Haditha. Also on July 7, Iraqi Security Forces (ISF) and area west of Baiji, killing ten IA and “Popular Mobilization” members and wounding over tribal ghters, reportedly supported by Iraqi and U.S.-led Coalition air support, attacked ISIS in 30. Federal Police (FP) and “Popular Mobilization” forces repelled an attack by ISIS at Barwana and Alus sub-districts, south of Haditha, and destroyed two SVBIEDs in al-Sakran area, al-Fatha, northeast of Baiji, killing 20 ISIS ghters. On July 8, IA and “Popular Mobili- northeast of Haditha, before they reached their targets. Albu Nimr and Albu Mahal tribal ghters zation” reinforcements reportedly arrived in Baiji. Clashes reportedly continue in the Baiji later repelled a counterattack by ISIS against Barwana. IA Aviation and U.S.-led Coalition Souq area of Baiji and in the Sakak area, west of Baiji. IA Aviation and the U.S.-led airstrikes also reportedly destroyed an ISIS convoy heading from Baiji to Barwana. Between July 6 Coalition conducted airstrikes on al-Siniya and al-Sukaria, west of Baiji and on the and 7, the DoD reported eight airstrikes “near Haditha.” On July 8, ISF and tribal ghters repelled petrochemical plant, north of Baiji. -

Weekly Explosive Incidents Flas
iMMAP - Humanitarian Access Response Weekly Explosive Incidents Flash News (23 - 29 APR 2020) 78 14 22 9 0 INCIDENTS PEOPLE KILLED PEOPLE INJURED EXPLOSIONS AIRSTRIKES DIYALA GOVERNORATE NINEWA GOVERNORATE ISIS 23/APR/2020 Security Forces 23/APR/2020 Four mortar shells landed in Abu Karma village in Al-Ibarra subdistrict, northeast of Diyala. Destroyed an ISIS hideout, killing three insurgents and seized 3 kilograms of C4 and other explosive materials, west of Mosul. ISIS 23/APR/2020 Attacked a security checkpoint, killing two Tribal Mobilization Forces members and Popular Mobilization Forces 23/APR/2020 injuring another in Tanira area, north of Muqdadiya district. Halted an ISIS infiltration attempt in Al-Hader district, southwest of Mosul. ISIS 24/APR/2020 Military Intelligence 23/APR/2020 Attacked and killed a Federal Police Forces member while riding his motorcycle in Found an ISIS hideout containing food, clothes, and motorcycle license plates in Umm Muqdadiya district, northeast of Diyala. Idham village, southwest of Mosul. ISIS 24/APR/2020 Federal Police Forces 24/APR/2020 Four mortar shells landed in the Al-Had Al-Ahdar area, injuring a civilian in Al-Ibarra Found a civilian corpse showing torture signs in the Kokjale area, east of Mosul. subdistrict, 14km northeast of Baqubah. ISIS 28/APR/2020 ISIS 25/APR/2020 Injured three civilians in an attack at Zalahfa village in Al-Shoora subdistrict, south of Bombarded the outskirts of Al-Zahra village using mortar shells in Al-Ibarra district. Mosul. ISIS 25/APR/2020 ISIS 29/APR/2020 Injured two Federal Police Forces members using a sniper rifle between Al-Kabaa and Abu Abducted a civilian in his workplace in the Al-Borsa area. -

2016: Accountability for the Victims and the Right to Truth
Enforced disappearances from Anbar governorate 2015-2016: Accountability for victims and the right to truth United Nations Assistance Mission for Iraq Office of the United Nations High Commissioner for Human Rights August 2020 Baghdad, Iraq Cover picture: still from a video of the Iraqi High Commission for Human Rights showing children from Anbar governorate holding pictures and identity documents of missing relatives, Photo credit: Iraqi High Commission for Human Rights – Anbar Governorate Office, June 2020 Contents I Executive summary ................................................................................................................. 5 II Mandate ................................................................................................................................... 6 III Methodology ........................................................................................................................... 7 IV Legal framework ...................................................................................................................... 7 4.1 International human rights law ....................................................................................... 7 4.2 International humanitarian law ...................................................................................... 9 4.3 International criminal law ............................................................................................. 10 4.4 National law .................................................................................................................. -

3 4 3 Iraq Situation Report: January 12-15, 2015
Iraq Situation Report: January 12-15, 2015 1 On January 13, an anonymous security source in Anbar Operation Command stated 6 On January 14, Governor of Diyala Amir al-Majmai called for that ISF and tribal ghters, with U.S. air support, are in ongoing clashes with ISIS in the tribes in the areas of Sansal and Arab Jubur near Muqdadiyah to areas around Rutba district west of Qaim, and have killed 22 ISIS members. Forces volunteer to ght ISIS “to receive weapons.” Majmai explained that “continue advancing towards the entrances of Rutba from the northern and southern directions.” Also, “a senior source from Jazeera and Badia Operations Command such forces will “hold the ground” to prevent damage to these areas ( JBOC)” stated that the operation extends beyond Rutba to clearing Walid sub-district, following operations .He stated that he will have a leadership role in Walid crossing, the Trebil crossing with Jordan, and the Ar-Ar crossing with Saudi these operations. Meanwhile, the local government in Muqdadiyah Arabia. On January 14, joint forces supported by coalition air cover “cordoned” Rutba in stated that it received many requests from residents to clear areas north preparation to storm the district while communication and internet services in Rutba of Muqdadiyah that are being used to launch indirect re attacks on were suspended. Another report indicated that the joint forces “halted” their advance to fortify their positions in areas they cleared near Rutba. e source claimed that the forces the district. Also, ISIS has reportedly evacuated three of its “main cleared the areas of Sagara, Owinnat, and “80 km,” located east of Rutba, and Hussainiyat, headquarters” in the area of Sansal Basin in preparation for the northwest of Rutba, in addition to the areas of “120 km” and “60 km” on the highway and expected launch of military operations to clear ISIS from the area.