Preincisional Analgesia with Intravenous Or Subcutaneous
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
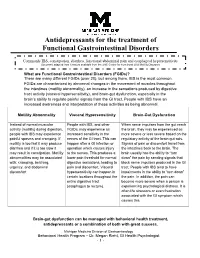
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -

The Cardiovascular Actions of Mu and Kappa Opioid Agonists In
THE CARDIOVASCULAR ACTIONS OF MU AND KAPPA OPIOID AGONISTS IN VIVO AND IN VITRO. By Abimbola T. Omoniyi, BSc (Hons) A thesis submitted in accordance with the requirements of the University of Surrey for the Degree of Doctor of Philosophy. Department of Pharmacology, September 1998. Cornell University Medical College, New York, NY 10021, ProQuest Number: 27733163 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 27733163 Published by ProQuest LLC (2019). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106 - 1346 ACKNOWLEDGEMENTS I would like to thank God through whom all things are made possible. Many thanks to Dr. Hazel Szeto for funding this thesis. Heartfelt gratitude to Dr. Dunli Wu for his support, encouragement and for keeping me sane. I thoroughly enjoyed the funny stories, the relentless Viagra jokes and endless tales of the Chinese revolution! Thanks to Dr. Yi Soong for all her support and generous assistance and all that food! Thanks to Dr. Ian Kitchen and Dr. Susanna Hourani for making this a successful collaborative degree. Thanks to my family for all their support and belief in me. -

Table 6.12 Deaths from Poisoning, by Sex and Cause, Scotland, 2004
Table 6.12 Deaths from poisoning, by sex and cause, Scotland, 2004 ICD Cause of death Both Males Females ICD Cause of death Both Males Females Codes and substance sexes Codes and substance sexes ACCIDENTS INTENTIONAL SELF-HARM X40 Accidental poisoning by and exposure X60 Intentional self-poisoning by -49 to noxious substances 57 40 17 -69 and exposure to 166 92 74 X40 Nonopioid analgesics, antipyretics X60 Nonopioid analgesics, antipyretics and antirheumatics and antirheumatics Ibuprofen 1 1 - Meptazinol, Alcohol 1 1 - Paracetamol 1 - 1 Meptazinol, Dihydrocodeine, Amitriptyline, Tramadol, Alcohol 1 1 - Imipramine, Alcohol 1 1 - Paracetamol 15 6 9 X41 Antiepileptic, sedative-hypnotic, Paracetamol, Codeine, Alcohol 1 1 - antiparkinsonism and Paracetamol, Diazepam 1 - 1 psychotropic drugs, Paracetamol, Oxazepam 1 1 - not elsewhere classified Tramadol 3 - 3 Clozapine, Diazepam, Alcohol 1 - 1 X61 Antiepileptic, sedative-hypnotic, antiparkinsonism and X42 Narcotics and psychodysleptics psychotropic drugs, (hallucinogens), not elsewhere not elsewhere classified classified Amitriptyline 8 3 5 Cocaine, Amphetamine 1 - 1 Amitriptyline, Alcohol 1 1 - Codeine, Tylex, Paracetamol, Alcohol 1 - 1 Amitriptyline, Dihydrocodeine 1 - 1 Dihydrocodeine, Diazepam 1 - 1 Amitriptyline, Paracetamol 1 1 - Ecstasy 1 1 - Carbamazepine 2 - 2 Heroin 4 3 1 Carbamazepine, Paroxetine, Paracetamol 1 1 - Heroin, Cocaine 1 1 - Chlordiazepoxide, Co-proxamol 1 - 1 Heroin, Methadone, Alcohol 1 1 - Chlorpromazine, Alcohol 2 2 - Heroin, Morphine 1 1 - Citalopram, Alcohol 1 - -

Effects of Medication-Assisted Treatment (MAT) on Functional Outcomes Among Patients with Opioid Use Disorder (OUD)
NATIONAL DEFENSE RESEARCH INSTITUTE Effects of Medication- Assisted Treatment (MAT) for Opioid Use Disorder on Functional Outcomes A Systematic Review Margaret A. Maglione, Laura Raaen, Christine Chen, Gulrez Shah Azhar, Nima Shahidinia, Mimi Shen, Ervant J. Maksabedian Hernandez, Roberta M. Shanman, Susanne Hempel Prepared for the Office of the Secretary of Defense Approved for public release; distribution unlimited For more information on this publication, visit www.rand.org/t/RR2108 Published by the RAND Corporation, Santa Monica, Calif. © Copyright 2018 RAND Corporation R® is a registered trademark. Limited Print and Electronic Distribution Rights This document and trademark(s) contained herein are protected by law. This representation of RAND intellectual property is provided for noncommercial use only. Unauthorized posting of this publication online is prohibited. Permission is given to duplicate this document for personal use only, as long as it is unaltered and complete. Permission is required from RAND to reproduce, or reuse in another form, any of its research documents for commercial use. For information on reprint and linking permissions, please visit www.rand.org/pubs/permissions. The RAND Corporation is a research organization that develops solutions to public policy challenges to help make communities throughout the world safer and more secure, healthier and more prosperous. RAND is nonprofit, nonpartisan, and committed to the public interest. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. Support RAND Make a tax-deductible charitable contribution at www.rand.org/giving/contribute www.rand.org Preface Over the past two decades, the U.S. Department of Defense (DoD) has invested unparalleled resources into developing effective treatments for military-related psychological health conditions. -
Guidelines for Prescribing Controlled Substances for Pain
GUIDELINES FOR PRESCRIBI NG CONTROLLED SUBSTANCE S FOR PAIN MEDICAL BOARD OF CALIFORNIA NOVEMBER 2014 Edmund G. Brown Jr., Governor David Serrano Sewell, J.D., President, Medical Board of California Kimberly Kirchmeyer, Executive Director, Medical Board of California Guidelines for Prescribing Controlled Substances for Pain Table of Contents PREAMBLE ..................................................................................................................... 1 UNDERSTANDING PAIN ................................................................................................ 2 Pain ............................................................................................................................. 2 Acute and Chronic Pain ............................................................................................... 3 Nociceptive and Neuropathic Pain ............................................................................... 3 Cancer and Non-Cancer Pain ...................................................................................... 3 Tolerance, Dependence and Addiction ........................................................................ 4 Pain as an Illness......................................................................................................... 4 SPECIAL PATIENT POPULATIONS............................................................................... 4 Acute Pain ................................................................................................................... 4 Emergency -

Double-Blind Crossover Trial of Oral Meptazinol, Pentazocine and Placebo in the Treatment of Pain in the Elderly V
Postgrad Med J: first published as 10.1136/pgmj.56.657.474 on 1 July 1980. Downloaded from Postgraduate Medical Journal (July 1980) 56, 474-477 Double-blind crossover trial of oral meptazinol, pentazocine and placebo in the treatment of pain in the elderly V. PEARCE P. J. ROBSON M.B. B.S., M.R.C.P. M.B. B.S., M.R.C.P. Chesterton Hospital, Cambridge and Wyeth Laboratories, Maidenhead, Berkshire Summary unit, pentazocine 25 mg orally, and placebo. The 2 In a randomized, double-blind crossover trial in 30 active drugs were given in deliberately small doses elderly patients suffering from moderate to severe as it is well recognized that age is highly correlated pain, the analgesic efficacy, tendency to produce with the pain relief obtained from a given dose of mental confusion and side effect profile of meptazinol analgesic (Beliville et al., 1971) and that the elderly 100 mg orally were compared with those of pentazo- are more susceptible to drugs in general (Leading cine 25 mg orally and placebo. Article, 1977). Both the active drugs produced significantly better analgesia than placebo but meptazinol also provided Materials and methods significantly better pain relief than pentazocine, This was a randomized double-blind crossover whilst at the same time causing less mental confusion. trial in 30 patients over the age of 70 years who had Side effects were unremarkable. given informed consent to participate and whocopyright. Meptazinol appears to be a better general purpose would in any case have required a potent oral anal- oral analgesic in this group of patients than penta- gesic. -

Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gutlbrain Interaction): a Rome Foundation Working Team Report Douglas A
Gastroenterology 2018;154:1140–1171 SPECIAL REPORT Neuromodulators for Functional Gastrointestinal Disorders (Disorders of GutLBrain Interaction): A Rome Foundation Working Team Report Douglas A. Drossman,1,2 Jan Tack,3 Alexander C. Ford,4,5 Eva Szigethy,6 Hans Törnblom,7 and Lukas Van Oudenhove8 1Center for Functional Gastrointestinal and Motility Disorders, University of North Carolina, Chapel Hill, North Carolina; 2Center for Education and Practice of Biopsychosocial Care and Drossman Gastroenterology, Chapel Hill, North Carolina; 3Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium; 4Leeds Institute of Biomedical and Clinical Sciences, University of Leeds, Leeds, United Kingdom; 5Leeds Gastroenterology Institute, St James’s University Hospital, Leeds, United Kingdom; 6Departments of Psychiatry and Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania; 7Departments of Internal Medicine and Clinical Nutrition, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; and 8Laboratory for BrainÀGut Axis Studies, Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium BACKGROUND & AIMS: Central neuromodulators (antide- summary information and guidelines for the use of central pressants, antipsychotics, and other central nervous neuromodulators in the treatment of chronic gastrointestinal systemÀtargeted medications) are increasingly used for treat- symptoms and FGIDs. Further studies are needed to confirm ment -
Guidelines for Pre Scribing Controlled Subs Tances for Pain
GUIDELINES FOR PRE SCRIBING CONTROLLED SUBS TANCES FOR PAIN MEDICAL BOARD OF CALIFORNIA NOVEMBER 2014 Edmund G. Brown Jr., Governor David Serrano Sewell, J.D., President, Medical Board of California Kimberly Kirchmeyer, Executive Director, Medical Board of California Guidelines for Prescribing Controlled Substances for Pain Table of Contents PREAMBLE ..................................................................................................................... 1 UNDERSTANDING PAIN ................................................................................................ 2 Pain 2............................................................................................................................. Acute and Chronic Pain3 ............................................................................................... Nociceptive and Neuropathic Pain 3............................................................................... Cancer and Non-Cancer Pain ...................................................................................... 3 Tolerance, Dependence and Addiction 4........................................................................ Pain as an Illness.........................................................................................................4 SPECIAL PATIENT POPULATIONS...............................................................................4 Acute Pain 4................................................................................................................... Emergency Departments -

Abdominal Visceral Pain: Clinical Aspect*
Rev Dor. São Paulo, 2013 out-dez;14(4):311-4 ARTIGO DE REVISÃO Abdominal visceral pain: clinical aspects* Dor visceral abdominal: aspectos clínicos Telma Mariotto Zakka1, Manoel Jacobsen Teixeira1, Lin Tchia Yeng1 *Recebido do Centro Interdisciplinar de Dor do Hospital de Clínicas da Faculdade de Medicina / Universidade de São Paulo. São Paulo, SP, Brasil. ABSTRACT CONTEÚDO: Como as doenças viscerais podem determinar dores de vários tipos e, habitualmente, desafiam os médicos no seu diagnós- BACKGROUND AND OBJECTIVES: Abdomen is the most fre- tico e tratamento, os autores descreveram de forma prática, as carac- quent site for acute or chronic painful syndromes, for referred pain terísticas dolorosas e as associações com as doenças mais incidentes. from distant structures or for pain caused by systemic injuries. Ab- CONCLUSÃO: O tratamento interdisciplinar com a associação das dominal visceral pain is induced by hollow viscera or parenchymal medidas farmacológicas aos procedimentos de medicina física e rea- viscera walls stretching or by peritoneal stretching. Complex diag- bilitação e ao acompanhamento psicológico diminui o sofrimento e nosis and treatment have motivated this study. Patients with chronic as incapacidades e melhora a qualidade de vida. abdominal pain are usually undertreated and underdiagnosed. The Descritores: Dor abdominal, Dor miofascial, Dor visceral, Trata- interdisciplinary treatment aims at minimizing patients’ distress, re- mento interdisciplinar. lieving pain and improving their quality of life. CONTENTS: Since visceral diseases may determine pain of different INTRODUÇÃO types and, usually, challenge physicians with regard to their diagnosis and treatment, the authors have described in a practical way painful A dor visceral pode decorrer por tensão ou estiramento da parede characteristics and associations with more common diseases. -

Clinical Evidence on Visceral Pain. Systematic Review Evidência Clínica Sobre Dor Visceral
Rev Dor. São Paulo, 2017 jan-mar;18(1):65-71 REVIEW ARTICLE Clinical evidence on visceral pain. Systematic review Evidência clínica sobre dor visceral. Revisão sistemática Durval Campos Kraychete1, José Tadeu Tesseroli de Siqueira2, João Batista Garcia3, Rioko Kimiko Sakata4, Ângela Maria Sousa5, Daniel Ciampi de Andrade6, Telma Regina Mariotto Zakka7, Manoel Jacobsen Teixeira7 and Diretoria da Sociedade Brasileira para o Estudo da Dor de 2015 DOI 10.5935/1806-0013.20170014 ABSTRACT RESUMO BACKGROUND AND OBJECTIVES: Visceral pain is in- JUSTIFICATIVA E OBJETIVOS: A dor visceral é causada por duced by abnormalities of organs such as stomach, kidneys, anormalidades de órgãos como o estômago, rim, bexiga, vesícula bladder, gallbladder, intestines and others and includes disten- biliar, intestinos ou outros e inclui distensão, isquemia, inflama- sion, ischemia, inflammation and mesenteric traction. It is re- ção e tração do mesentério. É responsável por incapacidade física sponsible for physical and psychic incapacity, absenteeism and e psíquica, absenteísmo do trabalho e má qualidade de vida. O poor quality of life. This study aimed at discussing major aspects objetivo deste estudo foi discutir os principais aspectos da dor of visceral pain with regard to prevalence, etiology and diagnosis. visceral relacionados a prevalência, etiologia e diagnóstico. CONTENTS: According to Evidence-Based Medicine concepts, CONTEÚDO: Foram revisados segundo os preceitos da Medic- visceral pain etiology, diagnosis and prognosis were reviewed in ina Baseada em Evidência os enfoques etiológicos, diagnóstico LILACS, EMBASE and Pubmed databases. Therapeutic stud- e prognóstico da dor visceral nas bases de indexações biomédi- ies were not selected. The following terms were used as search cas, LILACS, EMBASE e Pubmed. -

Assessment of Ethanol-Induced Toxicity on Ipsc-Derived Human
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.12.237461; this version posted August 12, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Assessment of ethanol-induced toxicity on iPSC-derived human dopaminergic neurons using a novel high-throughput mitochondrial neuronal health (MNH) assay Authors and affiliations: Annika Zink1,2,3, Josefin Conrad2, Narasimha Swami Telugu2, Sebastian Diecke2, Andreas Heinz1, Erich Wanker2, Josef Priller1,4*, Alessandro Prigione2,3* 1Department of Neuropsychiatry, Charité - Universitätsmedizin Berlin, Germany 2Max Delbrück Center for Molecular Medicine (MDC), Berlin, Germany 3Department of General Pediatrics, Neonatology, and Pediatric Cardiology, Heinrich Heine University, Duesseldorf, Germany 4University of Edinburgh and UK DRI, Edinburgh, UK *Co-Last Authors Contact information: *Prof. Dr. Josef Priller, Department of Neuropsychiatry, Charité - Universitätsmedizin Berlin, 10117 Berlin, Germany. Phone: +49 30 450517209, Email: [email protected] *Prof. Dr. Alessandro Prigione, Department of General Pediatrics, Neonatology and Pediatric Cardiology, Heinrich Heine University, Duesseldorf, Germany, Phone: +49 211 81 18705, Email: [email protected] Keywords: iPSCs, neurons, mitochondria, ethanol, high-content screening, neuronal toxicity Running title: High-throughput mitochondrial neuronal health assay 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.12.237461;