Abstractbandbstractband
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guest Editorial 1 Guest Editorial
Indian JJ PhysiolPhysiol PharmacolPharmacol 2012; 2012; 56(1) 56(1) : 1–6 Guest Editorial 1 Guest Editorial IMMUNOLOGY AND NOBEL PRIZE : A LOVE STORY Several breakthroughs revealing the way in which our bodies protect us against microscopic threats of almost any description have been duly acknowledged by the Nobel Prizes in Physiology or Medicine. Interestingly, Nobel Prizes in Physiology or Medicine including the latest one, for the year 2011, has been awarded for twelve times to the field of Immunology. The story began in 1901 with the very first Nobel Prize in Physiology or Medicine - it was awarded to Emil Von Behring for his pioneering work which resulted in the discovery of antitoxins, later termed as antibodies. Working with Shibasaburo Kitasato, Von Behring found that when animals were injected with tiny doses of weakened forms of tetanus or diphtheria bacteria, their blood extracts contained chemicals released in response, which rendered the pathogens’ toxins harmless. Naming these chemical agents ‘antitoxins’, Von Behring and Erich Wernicke showed that transferring antitoxin-containing blood serum into animals infected with the fully virulent versions of diphtheria bacteria cured the recipients of any symptoms, and prevented death. This was found to be true for humans also; and thus Von Behring’s method of treatment – passive serum therapy – became an essential remedy for diphtheria, saving many thousands of lives every year. Shortly after this, the very first explanation about the mechanisms of immune system’s functioning was proposed which paved way for extensive research in immunology till today. Paul Ehrlich had hit upon the key concept of how antibodies seek and neutralize the toxic actions of bacteria, while Ilya Mechnikov had discovered that certain body cells could destroy pathogens by simply engulfing or “eating” them. -

Emil Von Behring (1854–1917) the German Bacteriologist
Emil von Behring (1854–1917) The German bacteriologist and Nobel Prize winner Emil von Behring ranks among the most important medical scientists. Behring was born in Hansdorff, West Prussia, as the son of a teacher in 1854. He grew up in narrow circumstances among eleven brothers and sisters. His desire to study medicine could only be realized by fulfilling the obligation to work as an military doctor for a longer period of time. Between 1874 and 1878 he studied medicine at the Akademie für das militärärztliche Bildungswesen in Berlin. In 1890, after having published his paper Ueber das Zustandekommen der Diphtherie- Immunität und der Tetanus-Immunität bei Thieren, he captured his scientific breakthrough. While having worked as Robert Koch’s scientific assistant at the Berlin Hygienic Institute he had been able to show – together with his Japanese colleague Shibasaburo Kitasato (1852–1931) – via experimentation on animal that it was possible to neutralize pathogenic germs by giving „antitoxins“. Behring demonstrated that the antitoxic qualities of blood are not seated in cells, but in the cell-free serum. Antitoxins recovered of human convalenscents or laboratorty animals, prove themselves as life-saving when being applied to diseased humans. At last – due to Behring’s discovery of the body’s own immune defence and due to his development of serotherapy against diphtheria and tetanus – a remedy existed which was able to combat via antitoxin those infectious diseases which had already broken out. Having developped a serum therapy against diphtheria and tetanus Behring won the first Nobel Prize in Medicine in 1901. Six years before, in 1895, he had become professor of Hygienics within the Faculty of Medicine at the University of Marburg, a position he would hold for the rest of his life. -
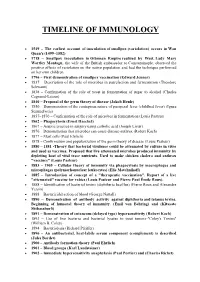
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Jahresbericht 2017
Das Streben nach Wahrheit und Erkenntnis gehört zum Schönsten, dessen der Mensch fähig ist. Albert Einstein, 1943 Einstein Stiftung Berlin 01 Grußbotschaft Berlin hat sich in den letzten Jahren zur Hauptstadt Die Förderung des wissenschaftlichen Nachwuchses der Wissenschaft entwickelt. Aus genau diesem Grund ist uns ein Anliegen und wir haben diesen Beitrag ger- haben wir uns bei Pfizer vor zehn Jahren dazu ent- ne geleistet. Wir danken der Einstein Stiftung sehr für schieden, unsere Deutschlandzentrale nach Berlin zu ihr Engagement und wünschen allen Absolventinnen verlegen. Denn bei wohl kaum einer anderen Branche und Absolventen viel Erfolg! liegen wissenschaftlicher und wirtschaftlicher Erfolg so eng beieinander wie in der Pharmazie. Viele unse- rer Produkte sind auf nobelpreisgekrönte Entdeckun- gen zurückzuführen: vom Penicillin, mit dem Infektio- nen ihren Schrecken verloren, über Impfstoffe, die vor schweren Krankheiten schützen, bis hin zu modernen Immuntherapeutika, die Krebspatienten neue Hoff- nung geben können. Umgekehrt gilt: Ohne die Mög- lichkeiten der großtechnischen Herstellung hätte Fle- mings Penicillin nie den vielen verwundeten Soldaten im Zweiten Weltkrieg helfen können, ohne die Expertise aus der Industrie würden vielversprechende Kandida- ten aus dem Labor oft nicht den mühsamen Weg durch die klinische Prüfung und die Zulassung finden. Viele Nobelpreisträger forschten in Berlin: Robert Koch ent- deckte hier den Tuberkuloseerreger, Emil von Behring das Serum gegen Diphtherie, Paul Ehrlich begründete an der Charité -

Awarded Nobel Prize for Contributions to Immunology
History of Immunology Molecular Immunology (MIR 511) August 27, 2013 Sharon S. Evans, Ph.D. Department of Immunology, RPCI (X3421) [email protected] Required reading: Owens; Immunology(7TH Edition) Chapter 1 – Overview of the Immune System: A Historical Perspective of Immunity Objectives 1. To gain a historical perspective of seminal research that provided underpinnings of immunology discipline. 2. To introduce key concepts of tumor immunology. Assigned Reading . Arthur M. Silverstein, Ilya Metchnikoff, the Phogocytic theory, and how things often work in science. J Leuk Biol 90:409, 2011. Jen-Marc Cavaillon, The historical milestones in the undersanding of leukocyte biology initiated by Elie Metchnikoff. J Leuk Biol 90:413, 2011. Historical Paradigms in General Immunology and Tumor Immunology 500 B.C. 1700s-1800s A.D. 2000 A.D. Recognition of Active Immunity/ Protection from Infectious Agents Molecular Mechanisms of Immunity (Ab, cells, cytokines) Tumor Immunity Survival of Species Depends on Defense Mechanisms • Fight/flight • Barriers - skin • Immune response-complexity depends on organism Vertebrates: •Organized lymphoid organs (spleen, thymus, bone marrow, lymph nodes, Peyer’s patches) •Complex circulatory system (lymphocyte trafficking) Immunity (Latin)-immunis Legal term = free from tax burden General Properties of Immune Response: Protect, defend organism from infectious agents • Innate immunity (NK, PMN, MO, megakaryocytes) • Primitive, higher organism • Adaptive immunity (B, T cells) • Only vertebrates Recognize self -

Proquest Dissertations
RICE UNIVERSITY Gd@C60-(ZME-018) Immunoconjugate Targeting of A375 Melanoma Cells by Christopher Scott Berger A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE Master of Arts Approved Thesis Committee: Lon J. Wilson, Chairman Professor of Chemistry W. Edward Billups Professor of Chemistry ^1 -u Ronald J. Parry Professor of Chemistry HOUSTON, TEXAS MAY 2010 UMI Number: 1486027 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. UMT Dissertation Publishing UMI 1486027 Copyright 2010 by ProQuest LLC. All rights reserved. This edition of the work is protected against unauthorized copying under Title 17, United States Code. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 Abstract Gd@C6o-(ZME-018) Immunoconjugate Targeting of A375 Melanoma Cells by Christopher Scott Berger For the first time, C6o-monoclonal antibody (mAb) immunoconjugates have been determined to internalize into target cells using water-soluble Gd3+-ion-filled fullerenes (Gd@Ceo(OH)x). Separate conjugations of Gd@C6o(OH)x with the antibody ZME-018 and a murine antibody mixture (MulgG) took place in a 1:5 mAb:Gd@C6o ratio. Quanitative analysis of the immunoconjugates was established using inductively-coupled plasma mass spectrometry (ICP-MS) and UV-Vis spectrometry (Gd@C6o+C6o). Enzyme- linked immunosorbent assays (ELISA) show little change in the specific binding of the ZME-018 once conjugated. -

The History of Healthcare Quality: the first 100 Years 1860–1960 ⇑ Brenda Helen Sheingold , Joyce A
Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Nursing Faculty Publications Nursing 2014 The iH story of Healthcare Quality: The irsF t 100 Years 1860-1960 Brenda Helen Sheingold George Washington University Joyce Hahn George Washington University Follow this and additional works at: http://hsrc.himmelfarb.gwu.edu/son_nurs_facpubs Part of the Nursing Commons Recommended Citation Sheingold, B. & Hahn, J. (2014) The iH story of Healthcare Quality: The irF st 100 Years 1860-1960. International Journal of Africa Nursing Sciences. 1(1), 18-22. This Journal Article is brought to you for free and open access by the Nursing at Health Sciences Research Commons. It has been accepted for inclusion in Nursing Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. International Journal of Africa Nursing Sciences 1 (2014) 18–22 Contents lists available at ScienceDirect International Journal of Africa Nursing Sciences journal homepage: www.elsevier.com/locate/ijans The history of healthcare quality: The first 100 years 1860–1960 ⇑ Brenda Helen Sheingold , Joyce A. Hahn The George Washington University, School of Nursing, 2030 M Street, NW, Suite 3021, Washington, DC 22036, United States article info abstract Article history: In the 21st Century, health care systems across the world are focusing policy efforts on improving the Received 17 July 2013 quality of healthcare delivered to their population. In contrast, healthcare quality improvement in earlier Received in revised form 15 April 2014 time periods arose from a series of seemingly unrelated incidents and developments. In this paper, we Accepted 23 May 2014 sequentially review key international historical events that improved health care quality during the years Available online 10 June 2014 1860–1960, including innovation in health care financing, care delivery and workforce diversity. -

Nobel Prize Commemoration in Riga: Media Echo and Objects
Acta medico-historica Rigensia (2018) XI: 92-120 doi:10.25143/amhr.2018.XI.03 Juris Salaks, Nils Hansson Nobel Prize Commemoration in Riga: Media Echo and Objects Abstract This paper is an attempt to investigate the discourses around the Nobel Prize, and it aims at deciphering the commemoration of the award in Riga. The public image of the Nobel Prize in Riga has previously been commented on in a few papers, but has never been studied at length. The first part of the current study contextualises several Nobel links from the city, universi- ties and state printed media, as well as more hidden tracks from the Nobel Prize nominations’ archive. The second part highlights Ilya Mechnikov (Elie Metchnikoff’s, Nobel laureate in physiology or medicine in 1908) collection in Pauls Stradins Museum of the History of Medicine, including a detailed description of his Nobel medal and his ambivalent feelings about this award. Keywords: Nobel Prize, Latvian press, Riga, Baltic States, Ilya Mechnikov (Elie Metchnikoff), Paul Ehrlich, Wilhelm Ostwald, Paul Valden, Ernst von Bergmann, Harald zur Hausen. Several compendia on the history of medicine use the Nobel Prize in physiology or medicine as a lens for reviewing scientific trends in the history of medicine in the last century. The medical historian Erwin Ackerknecht, for instance, argued that the tendencies of the 20th century cutting-edge medicine are illustrated by the names of those who received the Nobel Prize. 1 1 Erwin H. Ackerknecht, A short history of medicine (New York: Johns Hopkins University Press, 1968). 92 Also, more recent textbooks, such as Ortrun Riha’s Grundwissen Geschichte, Theorie und Ethik der Medizin 2, Jacalyn Duffin’s History of Medicine: A Scandalously Short Introduction 3, Tatiana Sorokina’s History of Medicine 4 have (at least in some editions) enclosed lists of Nobel laureates to highlight prominent work throughout the 20th century. -

Burnet Booklet.Indd
Second and Revised Edition, 2007 Introduction Professor Suzanne Cory, Director of The Walter and Eliza Hall Institute of Medical Research Frank Macfarlane Burnet’s theory of clonal selection Hall Institute of Medical Research an international focus on profoundly and forever changed the way that scientists all immunological research and application. Today, immunology over the world understand the working of immunity. In remains one of Australia’s strongest sciences. One third doing so, he brought to Victoria and The Walter and Eliza of the nation’s immunologists work in Victoria and four Australians of the Year have been immunologists. By comparison with today’s overwhelmingly collaborative nature of research and authorship, the circumstances of the creation of Burnet’s paper in 1957 appear quite amazing. While today we are accustomed to more than a dozen researchers acknowledged as contributors to a paper and papers likely to have been drafted many times over many months, by contrast Burnet’s paper was precisely that – Burnet’s alone; and he wrote the paper over the course of a weekend at home. Equally astonishing is the fact that such a revolutionary theory, which caused a seismic shift in thinking, was encapsulated in only a few pages of text. Part of the measure of the greatness of Burnet’s achievement is that today’s immunologists tell us that Burnet’s theories so thoroughly infuse their thinking that it seems impossible to imagine that the world of immunology could ever have been any other way. This universal infusion of Burnet’s theories marks him as one of Australia’s greatest ever scientists. -

Curriculum Vitae Paul Ehrlich (*1854 - †1915) German Medical Doctor – Serology and Immunology
Curriculum Vitae Paul Ehrlich (*1854 - †1915) German medical doctor – serology and immunology 1915 Paul Ehrlich died after a serious illness on 20 August 1915 at Bad Homburg vor der Höhe, Germany- 1912 Honorary citizen of Frankfurt a.M. and his birthplace, Strehlen, Germany 1911 Appointed as “Real Privy Councillor” with the additional title of “Excellency” (the highest civilian honour of the Prussian state) 1909 Discovery of Salvarsan (also called: Dioxy-diamino-arsenobenzol-dihydrochloride or preparation "606“), the first preparation for the treatment of syphilis, in co-operation with his most important co-worker, Sahachiro Hata 1908 Received the Nobel Prize for “Immortal contribution to medical and biological research, particularly to the valency determination of sera preparations”, together with Elia Metschnikow, who discovered phagocytosis 1907 Appointed as privy senior officer of health, honorary doctorate at Oxford 1906 Head of the Georg-Speyer-House for Chemotherapy 1904 Full Honorary Professor of the University of Göttingen and honorary doctorate of the University of Chicago 1903 Award winner of the Great Golden Medal of Science 1899 Head of the “Royal Institute of Experimental Therapy” at Frankfurt am Main 1897 Appointed as Privy Medical Officer of Health Publication of his side-chain theory in an essay “On the determination of the valency of the diphtheria serum” 1896 Appointed as Head of the “Institute for Sera Research and Serum Testing” that had been newly established in Steglitz, near Berlin 1891 Appointed by Robert Koch to the newly established Institute of Infectious Diseases in Berlin (today: Robert Koch Institute). There, he worked on the extraction of diphtheria serum and the determination of its concentration and valency and developed an internationally acknowledged unit of measurement. -

Chapter 3 Medicine in the 13-16Th Centuries Universities, Hospitals
Colophon Notes from the lessons on History of Medicine, taught to the students of the schools of medicine and nursing of the University of Cagliari, by Alessandro Riva, Professor Emeritus of Human Anatomy and of History of Medicine, Founder and Director (1991-2016) of the Museum of Clemente Susini's Anatomical Waxes. 2020 Edition. Reviewed and updated by Prof. Alessandro Riva ([email protected]) in collaboration with Dott. Francesco Loy. First Editorial reviewers: Francesca Testa Riva and Alessandro Riva First Ebook by Attilio Baghino Cover: Francesco Antonio Boi, watercolor by Gigi Camedda, Cagliari, 1978 courtesy of the picture-gallery, Olzai (Nuoro) First on line editions (2000) Editorial reviewer: Gabriele Conti. Webmastering: Andrea Casanova, Beniamino Orrù, Barbara Spina Last on line editions (2020) Editorial reviewer: Francesco Loy, Alessandro Riva Webmastering: Francesco Loy Tecnical support: Stefano Aramo The translation of the 1st Italian version was made by Clive Prestt and revised by Alessandro Riva and Bernard Tandler. Acknowledgments Editorial staff of previous on line versions: Felice Loffredo, Marco Piludu, Attilio Baghino Francesca Spina (less. 1); Lorenzo Fiorin (less. 2), Rita Piana (less. 3); Valentina Becciu (less. 4); Mario D'Atri (less. 5); Manuela Testa (less. 6); Raffaele Orrù (less. 7); Ramona Stara (less. 8), are the medical students, now practising physicians, who made notes of the Prof. Riva’s lessons in the academic year 1997-1998. © Copyright 2020, Università di Cagliari This work is licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/. -

Message from Future Generations*
Message from future generations* ̶Now is the time to establish a direction and a philosophy for science ● Katsuhiko HAYASHI Principal at the School of Science and Technology Journalists and Vice President of the Science Visualization Society of Japan How will future generations living in the 22nd century see people priority was given to the efficiency and desires of the existing living in the current period? What kind of society can we, living in generations and thus lacked the panoramic and permanent view the present, pass on to future generations? of science and technology. There is a saying“ Onko Chishin” in the Analects of Confucius, Although concepts such as“ sustainable development” and meaning“ exploring the past to know the new.” So let’s start by “nation based on the creativity of science and technology” are looking back to science and technology in the 20th century. In correct, these words indicate neither a specific direction nor any 1901, the First Nobel Prize Award Ceremony was held―the most philosophy. When it comes to science and technology for the 21st fitting event for the dawn of the 20th century. These Prizes were century, the pursuit of advanced knowledge is absolutely essen- established in accordance with the last will and testament of tial, but that is not enough. With consideration of“ future genera- Alfred Bernhard Nobel, a chemist, engineer and businessman. tions” as the keyword during such processes, this author would He condemned himself for his invention of dynamite, which had like to desire a paradigm shift to be realized toward the direction begun to be used as a tool of war at the same time, and, for the of: (1) making an international contribution through develop- welfare of mankind, left a will requesting the establishment of ment of the world’s greatest technology and industries within Nobel Prizes for outstanding achievements.