Chapter 3 Medicine in the 13-16Th Centuries Universities, Hospitals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Prezentace Aplikace Powerpoint
KapitolyKapitoly zz neurofyziologieneurofyziologie smyslsmyslůů NeurofyziologieNeurofyziologie Ambice:Ambice: PochopenPochopeníí psychikypsychiky ččlovlověěkaka aa jejjejííchch poruch.poruch. BouBouřřlivýlivý rozvoj:rozvoj: MolekulMolekuláárnrníí neurovneurověědydy NeurofarmakologieNeurofarmakologie ZobrazovacZobrazovacíí metodymetody Nobel prices related to neuroscience 1901 Wilhelm Conrad Röntgen (Germany) "in recognition of the extraordinary services he has rendered by the discovery of the remarkable rays subsequently named after him" 1904 Ivan Petrovich Pavlov (Russia) "in recognition of his work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged" 1906 Camillo Golgi (Italy) and Santiago Ramón y Cajal (Spain) "in recognition of their work on the structure of the nervous system" 1909 Emil Theodor Kocher (Switzerland) "for his work on the physiology, pathology and surgery of the thyroid gland" 1914 Robert Bárány (Vienna) "for his work on the physiology and pathology of the vestibular apparatus" 1920 Chemistry: Walther Hermann Nernst (Germany) "in recognition of his work in thermochemistry" 1932 Sir Charles Scott Sherrington (Great Britain) and Edgar Douglas Adrian (Great Britain) "for their discoveries regarding the functions of neurons" 1935 Hans Spemann (Germany) "for his discovery of the organizer effect in embryonic development" 1936 Sir Henry Hallett Dale (Great Britain) and Otto Loewi (Great Britain) "for their discoveries relating to chemical transmission of -

書 名 等 発行年 出版社 受賞年 備考 N1 Ueber Das Zustandekommen Der
書 名 等 発行年 出版社 受賞年 備考 Ueber das Zustandekommen der Diphtherie-immunitat und der Tetanus-Immunitat bei thieren / Emil Adolf N1 1890 Georg thieme 1901 von Behring N2 Diphtherie und tetanus immunitaet / Emil Adolf von Behring und Kitasato 19-- [Akitomo Matsuki] 1901 Malarial fever its cause, prevention and treatment containing full details for the use of travellers, University press of N3 1902 1902 sportsmen, soldiers, and residents in malarious places / by Ronald Ross liverpool Ueber die Anwendung von concentrirten chemischen Lichtstrahlen in der Medicin / von Prof. Dr. Niels N4 1899 F.C.W.Vogel 1903 Ryberg Finsen Mit 4 Abbildungen und 2 Tafeln Twenty-five years of objective study of the higher nervous activity (behaviour) of animals / Ivan N5 Petrovitch Pavlov ; translated and edited by W. Horsley Gantt ; with the collaboration of G. Volborth ; and c1928 International Publishing 1904 an introduction by Walter B. Cannon Conditioned reflexes : an investigation of the physiological activity of the cerebral cortex / by Ivan Oxford University N6 1927 1904 Petrovitch Pavlov ; translated and edited by G.V. Anrep Press N7 Die Ätiologie und die Bekämpfung der Tuberkulose / Robert Koch ; eingeleitet von M. Kirchner 1912 J.A.Barth 1905 N8 Neue Darstellung vom histologischen Bau des Centralnervensystems / von Santiago Ramón y Cajal 1893 Veit 1906 Traité des fiévres palustres : avec la description des microbes du paludisme / par Charles Louis Alphonse N9 1884 Octave Doin 1907 Laveran N10 Embryologie des Scorpions / von Ilya Ilyich Mechnikov 1870 Wilhelm Engelmann 1908 Immunität bei Infektionskrankheiten / Ilya Ilyich Mechnikov ; einzig autorisierte übersetzung von Julius N11 1902 Gustav Fischer 1908 Meyer Die experimentelle Chemotherapie der Spirillosen : Syphilis, Rückfallfieber, Hühnerspirillose, Frambösie / N12 1910 J.Springer 1908 von Paul Ehrlich und S. -

09 Piqueras.Qxp
PERSPECTIVES INTERNATIONAL MICROBIOLOGY (2007) 10:217-226 DOI: 10.2436/20.1501.01.30 ISSN: 1139-6709 www.im.microbios.org Microbiology: a dangerous profession? Mercè Piqueras President, Catalan Association for Science Communication (ACCC), Barcelona, Spain The history of science contains many cases of researchers eases in Minorca from the year 1744 to 1749 to which is pre- who have died because of their professional activity. In the fixed, a short account of the climate, productions, inhabi- field of microbiology, some have died or have come close to tants, and endemical distempers of that island (T. Cadell, D. death from infection by agents that were the subject of their Wilson and G. Nicol, London, 1751), which he dedicated to research (Table 1). Infections that had a lethal outcome were the Society of Surgeons of His Majesty’s Royal Navy. usually accidental. Sometimes, however, researchers inocu- Minorcan historian of science Josep M. Vidal Hernández has lated themselves with the pathogen or did not take preventive described and carefully analyzed Cleghorn’s work in measures against the potential pathogen because they wanted Minorca and his report [43]. According to Vidal, what to prove their hypotheses—or disprove someone else’s— Cleghorn describes is “tertian” fever, which was the name regarding the origin of the infection. Here is an overview of given at the time to fever caused by malaria parasites with a several episodes in the history of microbiology since the mid periodicity of 48 hours. In fact, Cleghorn used quinine to nineteenth century involving researchers or workers in fields treat tertian fever (i.e, malaria), which was not eradicated related to microbiology who have become infected. -

Nobel Prizes
W W de Herder Heroes in endocrinology: 1–11 3:R94 Review Nobel Prizes Open Access Heroes in endocrinology: Nobel Prizes Correspondence Wouter W de Herder should be addressed to W W de Herder Section of Endocrinology, Department of Internal Medicine, Erasmus MC, ’s Gravendijkwal 230, 3015 CE Rotterdam, Email The Netherlands [email protected] Abstract The Nobel Prize in Physiology or Medicine was first awarded in 1901. Since then, the Nobel Key Words Prizes in Physiology or Medicine, Chemistry and Physics have been awarded to at least 33 " diabetes distinguished researchers who were directly or indirectly involved in research into the field " pituitary of endocrinology. This paper reflects on the life histories, careers and achievements of 11 of " thyroid them: Frederick G Banting, Roger Guillemin, Philip S Hench, Bernardo A Houssay, Edward " adrenal C Kendall, E Theodor Kocher, John J R Macleod, Tadeus Reichstein, Andrew V Schally, Earl " neuroendocrinology W Sutherland, Jr and Rosalyn Yalow. All were eminent scientists, distinguished lecturers and winners of many prizes and awards. Endocrine Connections (2014) 3, R94–R104 Introduction Endocrine Connections Among all the prizes awarded for life achievements in In 1901, the first prize was awarded to the German medical research, the Nobel Prize in Physiology or physiologist Emil A von Behring (3, 4). This award heralded Medicine is considered the most prestigious. the first recognition of extraordinary advances in medicine The Swedish chemist and engineer, Alfred Bernhard that has become the legacy of Nobel’s prescient idea to Nobel (1833–1896), is well known as the inventor of recognise global excellence. -

Tierversuche in Der Forschung Senatskommission Für Tierexperimentelle Forschung Der Deutschen Forschungsgemeinschaft Tierversuche in Der Forschung 3 2
Senatskommission für tierexperimentelle Forschung der Deutschen Forschungsgemeinschaft Tierversuche in der Forschung Senatskommission für tierexperimentelle Forschung der Deutschen Forschungsgemeinschaft Tierversuche in der Forschung 2 3 Inhalt Vorwort �� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 4 Tierversuche und Tierschutz: Ethische Abwägungen Einführung �� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 6 Die Entwicklung des Tierschutzgedankens in Deutschland �� � � � � � � � � � � � � 39 Ethische Aspekte von Tierversuchen und das Solidaritätsprinzip� � � � � � � � 40 Tierversuche: Definition und Zahlen Die Übertragbarkeit aus ethisch-rechtlicher Sicht� � � � � � � � � � � � � � � � � � � � � � 45 Was ist ein Tierversuch? �� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 9 Das 3 R-Prinzip �� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 48 Wie viele Tiere werden verwendet? �� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 9 Alternativen zum Tierversuch� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 51 Wofür werden Tiere in der Forschung benötigt? �� � � � � � � � � � � � � � � � � � � � � � 11 Grenzen von Alternativmethoden� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 54 Welche Tierarten werden eingesetzt? �� -

Tierversuche in Der Forschung Senatskommission Für Tierexperimentelle Forschung Der Deutschen Forschungsgemeinschaft Tierversuche in Der Forschung 2 3
Senatskommission für tierexperimentelle Forschung der Deutschen Forschungsgemeinschaft Tierversuche in der Forschung Senatskommission für tierexperimentelle Forschung der Deutschen Forschungsgemeinschaft Tierversuche in der Forschung 2 3 Inhalt Vorwort . 4 Tierversuche und Tierschutz: Ethische Abwägungen Einführung . 6 Die Entwicklung des Tierschutzgedankens in Deutschland . 39 Ethische Aspekte von Tierversuchen und das Solidaritätsprinzip. 40 Tierversuche: Definition und Zahlen Die Übertragbarkeit aus ethisch-rechtlicher Sicht. 45 Was ist ein Tierversuch? . 9 Das 3 R-Prinzip . 48 Wie viele Tiere werden verwendet? . 9 Alternativen zum Tierversuch. 51 Wofür werden Tiere in der Forschung benötigt? . 11 Grenzen von Alternativmethoden. 54 Welche Tierarten werden eingesetzt? . 11 Die Basler Deklaration . 56 Europaweite Entwicklung . 14 Tierversuche in Deutschland: Vom Antrag bis zur Durchführung Tierexperimentelle Praxis: Einsatzbereiche für Versuchstiere Europäische Regelungen für Tierversuche . 59 Grundlagenforschung. 17 Tierversuche unter Genehmigungsvorbehalt . 60 Medizinische Forschung. 18 Rechtliche Grundlagen . 60 Nobelpreiswürdig: Herausragende wissenschaftliche Erkenntnisse . 20 Genehmigungsverfahren . 63 Diagnostik . 22 Durchführung von Tierversuchen . 64 Transplantationsmedizin . 25 Qualifizierte Überwachung. 68 Zell- und Gewebeersatz beim Menschen. 26 Belastungen für die Tiere . 69 Stammzellforschung . 27 Die Tierschutz-Verbandsklage . 71 Genomforschung . 28 Neurowissenschaften . 31 Anhang Veterinärmedizinische Forschung . 33 Tierversuche -

Issue 4 (December, 2019)
Geological Society of Africa Newsletter Volume 9 - Issue 4 (December, 2019) Since the Nobel prize was established, 27 African and African-born persons and African organizations got it. YES Africa can do it !!! Stories inside the issue Africa and Nobel prize CAG28 is approaching Toward a better communication Edited by Tamer Abu-Alam Editor of the GSAf Newsletter In the issue GSAF MATTERS 1 KNOW AFRICA (COVER STORY) 10 GEOLOGY COMIC 11 GEOLOGICAL EXPRESSIONS 11 AFRICAN GEOPARK AND GEOHERITAGE 13 AFRICA'S NOBEL PRIZE WINNERS: A LIST 14 NEWS 23 LITERATURE 30 OPPORTUNITIES 38 CONTACT THE COUNCIL 42 Geological Society of Africa – Newsletter Volume 9 – Issue 4 December 2019 © Geological Society of Africa http://gsafr.org Temporary contact: [email protected] GSAf MATTERS Toward a better and a faster communication among the African community of Geosciences By Tamer Abu-Alam (GSAf newsletter editor and information officer) Information and news should be communicated in a faster way than a newsletter. For example, a deadline to apply for a scholarship can be easily missed if it is not posted to the community at a proper time. As a result, and for better and faster communication among the geological society of Africa, the GSAf will use a Gmail group ([email protected]) to facilitate the communication between society members. Some advice and rules: Since any member can post and all the members will receive your message, please do not overload the society by un-related news. Post only important news that wants immediate action from members. Improper messages can lead its owner to be blocked from posting. -

Guest Editorial 1 Guest Editorial
Indian JJ PhysiolPhysiol PharmacolPharmacol 2012; 2012; 56(1) 56(1) : 1–6 Guest Editorial 1 Guest Editorial IMMUNOLOGY AND NOBEL PRIZE : A LOVE STORY Several breakthroughs revealing the way in which our bodies protect us against microscopic threats of almost any description have been duly acknowledged by the Nobel Prizes in Physiology or Medicine. Interestingly, Nobel Prizes in Physiology or Medicine including the latest one, for the year 2011, has been awarded for twelve times to the field of Immunology. The story began in 1901 with the very first Nobel Prize in Physiology or Medicine - it was awarded to Emil Von Behring for his pioneering work which resulted in the discovery of antitoxins, later termed as antibodies. Working with Shibasaburo Kitasato, Von Behring found that when animals were injected with tiny doses of weakened forms of tetanus or diphtheria bacteria, their blood extracts contained chemicals released in response, which rendered the pathogens’ toxins harmless. Naming these chemical agents ‘antitoxins’, Von Behring and Erich Wernicke showed that transferring antitoxin-containing blood serum into animals infected with the fully virulent versions of diphtheria bacteria cured the recipients of any symptoms, and prevented death. This was found to be true for humans also; and thus Von Behring’s method of treatment – passive serum therapy – became an essential remedy for diphtheria, saving many thousands of lives every year. Shortly after this, the very first explanation about the mechanisms of immune system’s functioning was proposed which paved way for extensive research in immunology till today. Paul Ehrlich had hit upon the key concept of how antibodies seek and neutralize the toxic actions of bacteria, while Ilya Mechnikov had discovered that certain body cells could destroy pathogens by simply engulfing or “eating” them. -

Emil Von Behring (1854–1917) the German Bacteriologist
Emil von Behring (1854–1917) The German bacteriologist and Nobel Prize winner Emil von Behring ranks among the most important medical scientists. Behring was born in Hansdorff, West Prussia, as the son of a teacher in 1854. He grew up in narrow circumstances among eleven brothers and sisters. His desire to study medicine could only be realized by fulfilling the obligation to work as an military doctor for a longer period of time. Between 1874 and 1878 he studied medicine at the Akademie für das militärärztliche Bildungswesen in Berlin. In 1890, after having published his paper Ueber das Zustandekommen der Diphtherie- Immunität und der Tetanus-Immunität bei Thieren, he captured his scientific breakthrough. While having worked as Robert Koch’s scientific assistant at the Berlin Hygienic Institute he had been able to show – together with his Japanese colleague Shibasaburo Kitasato (1852–1931) – via experimentation on animal that it was possible to neutralize pathogenic germs by giving „antitoxins“. Behring demonstrated that the antitoxic qualities of blood are not seated in cells, but in the cell-free serum. Antitoxins recovered of human convalenscents or laboratorty animals, prove themselves as life-saving when being applied to diseased humans. At last – due to Behring’s discovery of the body’s own immune defence and due to his development of serotherapy against diphtheria and tetanus – a remedy existed which was able to combat via antitoxin those infectious diseases which had already broken out. Having developped a serum therapy against diphtheria and tetanus Behring won the first Nobel Prize in Medicine in 1901. Six years before, in 1895, he had become professor of Hygienics within the Faculty of Medicine at the University of Marburg, a position he would hold for the rest of his life. -

The Impact of NMR and MRI
WELLCOME WITNESSES TO TWENTIETH CENTURY MEDICINE _____________________________________________________________________________ MAKING THE HUMAN BODY TRANSPARENT: THE IMPACT OF NUCLEAR MAGNETIC RESONANCE AND MAGNETIC RESONANCE IMAGING _________________________________________________ RESEARCH IN GENERAL PRACTICE __________________________________ DRUGS IN PSYCHIATRIC PRACTICE ______________________ THE MRC COMMON COLD UNIT ____________________________________ WITNESS SEMINAR TRANSCRIPTS EDITED BY: E M TANSEY D A CHRISTIE L A REYNOLDS Volume Two – September 1998 ©The Trustee of the Wellcome Trust, London, 1998 First published by the Wellcome Trust, 1998 Occasional Publication no. 6, 1998 The Wellcome Trust is a registered charity, no. 210183. ISBN 978 186983 539 1 All volumes are freely available online at www.history.qmul.ac.uk/research/modbiomed/wellcome_witnesses/ Please cite as : Tansey E M, Christie D A, Reynolds L A. (eds) (1998) Wellcome Witnesses to Twentieth Century Medicine, vol. 2. London: Wellcome Trust. Key Front cover photographs, L to R from the top: Professor Sir Godfrey Hounsfield, speaking (NMR) Professor Robert Steiner, Professor Sir Martin Wood, Professor Sir Rex Richards (NMR) Dr Alan Broadhurst, Dr David Healy (Psy) Dr James Lovelock, Mrs Betty Porterfield (CCU) Professor Alec Jenner (Psy) Professor David Hannay (GPs) Dr Donna Chaproniere (CCU) Professor Merton Sandler (Psy) Professor George Radda (NMR) Mr Keith (Tom) Thompson (CCU) Back cover photographs, L to R, from the top: Professor Hannah Steinberg, Professor -
Timeline of Immunology
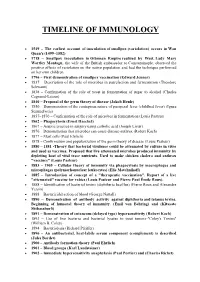
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Research Organizations and Major Discoveries in Twentieth-Century Science: a Case Study of Excellence in Biomedical Research
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Hollingsworth, Joseph Rogers Working Paper Research organizations and major discoveries in twentieth-century science: A case study of excellence in biomedical research WZB Discussion Paper, No. P 02-003 Provided in Cooperation with: WZB Berlin Social Science Center Suggested Citation: Hollingsworth, Joseph Rogers (2002) : Research organizations and major discoveries in twentieth-century science: A case study of excellence in biomedical research, WZB Discussion Paper, No. P 02-003, Wissenschaftszentrum Berlin für Sozialforschung (WZB), Berlin This Version is available at: http://hdl.handle.net/10419/50229 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von diesen Nutzungsbedingungen die in der dort Content Licence (especially Creative Commons Licences), you genannten Lizenz gewährten Nutzungsrechte. may exercise further usage rights as specified in the indicated licence. www.econstor.eu P 02 – 003 RESEARCH ORGANIZATIONS AND MAJOR DISCOVERIES IN TWENTIETH-CENTURY SCIENCE: A CASE STUDY OF EXCELLENCE IN BIOMEDICAL RESEARCH J.