Cerebrovascular Amyloid Angiopathy in Bioengineered Vessels Is
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
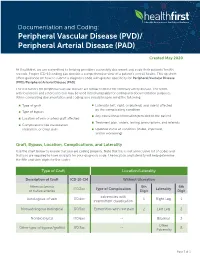
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Peripheral Artery Disease (Pad)
PERIPHERAL ARTERY DISEASE (PAD) Provider’s guide to diagnose and code PAD Peripheral Artery Disease (ICD-10 code I73.9) is estimated The American Cardiology and American Heart Association to affect 12 to 20% of Americans age 65 and older with as 2013 revised guidelines recommend the following many as 75% of that group being asymptomatic (Rogers et al, interpretation for noncompression values for ABI 2011). Of note, for the purposes of this clinical flyer the term (Anderson, 2013). peripheral vascular disease (PVD) is used synonymously with PAD. Table 2: Interpretation of ABI Values Who and how to screen for PAD Value Interpretation The updated 2013 American College of Cardiology and > 1.30 Non-compressible American Heart Association guidelines for the management of 1.00 – 1.29 Normal patients with PAD, recommends screening patients at risk for lower extremity PAD (Anderson et al, 2013). 0.91 – 0.99 Borderline The guidelines recommend reviewing vascular signs and 0.41 - 0.90 Mild to moderate PAD symptoms (e.g., walking impairment, claudication, ischemic 0.00 – 0.40 Severe PAD rest pain and/or presence of non-healing wounds) and physical examination (e.g., evaluation of pulses and inspection The diagnostic accuracy of the ABI can be hindered under the of lower extremities). The Trans-Atlantic Inter-Society following conditions: (Ruff, 2003) Consensus Document on Management of PAD and U.S. Preventative Task Force on screening for PAD identify similar › Patient anxiety and/or discomfort screening criteria that address patient’s age, smoking history, › Poor positioning of patient or restless patient co-morbid conditions and physical exam findings (Moyer, 2013 & Norgren et al, 2007). -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -

Cell Communication and Signaling Biomed Central
Cell Communication and Signaling BioMed Central Review Open Access Extravasation of leukocytes in comparison to tumor cells Carina Strell and Frank Entschladen* Address: Institute of Immunology, Witten/Herdecke University, Stockumer Str. 10, 58448 Witten, Germany Email: Carina Strell - [email protected]; Frank Entschladen* - [email protected] * Corresponding author Published: 4 December 2008 Received: 18 November 2008 Accepted: 4 December 2008 Cell Communication and Signaling 2008, 6:10 doi:10.1186/1478-811X-6-10 This article is available from: http://www.biosignaling.com/content/6/1/10 © 2008 Strell and Entschladen; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract The multi-step process of the emigration of cells from the blood stream through the vascular endothelium into the tissue has been termed extravasation. The extravasation of leukocytes is fairly well characterized down to the molecular level, and has been reviewed in several aspects. Comparatively little is known about the extravasation of tumor cells, which is part of the hematogenic metastasis formation. Although the steps of the process are basically the same in leukocytes and tumor cells, i.e. rolling, adhesion, transmigration (diapedesis), the molecules that are involved are different. A further important difference is that leukocyte interaction with the endothelium changes the endothelial integrity only temporarily, whereas tumor cell interaction leads to an irreversible damage of the endothelial architecture. Moreover, tumor cells utilize leukocytes for their extravasation as linkers to the endothelium. -
Lysosomal Membrane Glycoproteins Bind Cholesterol and Contribute to Lysosomal Cholesterol Export
1 Lysosomal membrane glycoproteins bind cholesterol and 2 contribute to lysosomal cholesterol export 3 4 Jian Li and Suzanne R. Pfeffer* 5 Department of Biochemistry, Stanford University School of Medicine 6 Stanford, CA USA 94305-5307 7 8 *Correspondence to: [email protected]. 9 10 Abstract: LAMP1 and LAMP2 proteins are highly abundant, ubiquitous, mammalian proteins 11 that line the lysosome limiting membrane, and protect it from lysosomal hydrolase action. 12 LAMP2 deficiency causes Danon’s disease, an X-linked hypertrophic cardiomyopathy. LAMP2 13 is needed for chaperone-mediated autophagy, and its expression improves tissue function in 14 models of aging. We show here that LAMP1 and LAMP2 bind cholesterol in a manner that 15 buries the cholesterol 3β-hydroxyl group; they also bind tightly to NPC1 and NPC2 proteins that 16 export cholesterol from lysosomes. Quantitation of cellular LAMP2 and NPC1 protein levels 17 suggest that LAMP proteins represent a significant cholesterol binding site at the lysosome 18 limiting membrane, and may signal cholesterol availability. Functional rescue experiments show 19 that the ability of LAMP2 to facilitate cholesterol export from lysosomes relies on its ability to 20 bind cholesterol directly. 21 22 23 Introduction 24 Eukaryotic lysosomes are acidic, membrane-bound organelles that contain proteases, lipases and 25 nucleases and degrade cellular components to regenerate catabolic precursors for cellular use (1- 26 3). Lysosomes are crucial for the degradation of substrates from the cytoplasm, as well as 27 membrane bound compartments derived from the secretory, endocytic, autophagic and 28 phagocytic pathways. The limiting membrane of lysosomes is lined with so-called lysosomal 29 membrane glycoproteins (LAMPs) that are comprised of a short cytoplasmic domain, a single 30 transmembrane span, and a highly, N- and O-glycosylated lumenal domain (4-6). -

Sensitization to the Lysosomal Cell Death Pathway by Oncogene- Induced Down-Regulation of Lysosome-Associated Membrane Proteins 1 and 2
Research Article Sensitization to the Lysosomal Cell Death Pathway by Oncogene- Induced Down-regulation of Lysosome-Associated Membrane Proteins 1 and 2 Nicole Fehrenbacher,1 Lone Bastholm,2 Thomas Kirkegaard-Sørensen,1 Bo Rafn,1 Trine Bøttzauw,1 Christina Nielsen,1 Ekkehard Weber,3 Senji Shirasawa,4 Tuula Kallunki,1 and Marja Ja¨a¨ttela¨1 1Apoptosis Department and Centre for Genotoxic Stress Response, Institute for Cancer Biology, Danish Cancer Society; 2Institute of Molecular Pathology, Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark; 3Institute of Physiological Chemistry, Medical Faculty, Martin-Luther-University Halle-Wittenberg, Halle, Germany; and 4Department of Cell Biology, School of Medicine, Fukuoka University, Fukuoka, Japan Abstract molecules of the cell to breakdown products available for Expression and activity of lysosomal cysteine cathepsins metabolic reuse (3, 4). Cathepsin proteases are among the best- correlate with the metastatic capacity and aggressiveness of studied lysosomal hydrolases. They are maximally active at the tumors. Here, we show that transformation of murine acidic pH of lysosomes (pH 4–5). However, many of them can be Y527F embryonic fibroblasts with v-H-ras or c-src changes the active at the neutral pH outside lysosomes, albeit with a decreased distribution, density, and ultrastructure of the lysosomes, efficacy and/or altered specificity (5). For example, transformation and tumor environment enhance the expression of lysosomal decreases the levels of lysosome-associated membrane pro- teins (LAMP-1 and LAMP-2) in an extracellular signal- cysteine cathepsins and increase their secretion into the extracel- regulated kinase (ERK)- and cathepsin-dependent manner, lular space (6). Once outside the tumor cells, cathepsins stimulate and sensitizes the cells to lysosomal cell death pathways angiogenesis, tumor growth, and invasion in murine cancer induced by various anticancer drugs (i.e., cisplatin, etoposide, models, thereby enhancing cancer progression (7, 8). -

Intracerebral Hemorrhage
Circulation Journal ORIGINAL ARTICLE Circ J 2019; 83: 441 – 446 doi: 10.1253/circj.CJ-18-0938 Stroke Safety of Anticoagulant Therapy Including Direct Oral Anticoagulants in Patients With Acute Spontaneous Intracerebral Hemorrhage Yuki Sakamoto, MD; Chikako Nito, MD, PhD; Yasuhiro Nishiyama, MD, PhD; Satoshi Suda, MD, PhD; Noriko Matsumoto, MD, PhD; Junya Aoki, MD, PhD; Takashi Shimoyama, MD, PhD; Takuya Kanamaru, MD, PhD; Kentaro Suzuki, MD; Takuya Nishimura, MD; Masahiro Mishina, MD, PhD; Kazumi Kimura, MD, PhD Background: Because the efficacy and safety of anticoagulant therapy in patients with acute intracerebral hemorrhage (ICH) are not fully known, present study aimed to elucidate the current status and the safety of anticoagulant therapy, mainly direct oral anticoagulants (DOACs), for acute ICH and anticoagulant-indicated patients. Methods and Results: From September 2014 through March 2017, consecutive patients with acute (<7 days from onset), sponta- neous ICH were retrospectively enrolled from a prospective registry. Whether to start anticoagulation was at the attending physicians’ discretion, and thromboembolic or hemorrhagic events during hospitalization were analyzed. A total of 236 patients (80 women [34%]; median age 69 [interquartile range 61–79] years; National Institutes of Health stroke scale score 7 [3–16]) were enrolled. Of them, 47 patients (20%) had an indication for anticoagulant therapy (33 had atrial fibrillation, 14 developed deep vein thrombosis), and 41 of 47 patients (87%) were actually treated with anticoagulant therapy (DOACs were used in 34 patients) after a median of 7 days from ICH onset. There was neither hematoma expansion nor excessive hemorrhagic complications during hospitalization after starting anticoagulant therapy. -

Origin of the Microangiopathic Changes in Diabetes
ORIGIN OF THE MICROANGIOPATHIC CHANGES IN DIABETES A. H. BARNETT Birmingham SUMMARY its glycosidally linked disaccharide units. Such alterations The mechanism of development of microangiopathy is lead to abnormal packing of the peptide chains producing incompletely understood, but relates to a number of excessive leakiness of the membrane. The exact mech ultrastructural, biochemical and haemostatic processes. anisms of thickening and leakiness of basement mem These include capillary basement membrane thickening, brane and their relevance to diabetic complications are not non-enzymatic glycosylation, possibly increased free rad entirely clear, but appear to involve several biochemical ical activity, increased flux through the polyol pathway mechanisms. and haemostatic abnormalities. The central feature Non-enzymatic Glycosylation appears to be hyperglycaemia, which is causally related to the above processes and culminates in tissue ischaemia. In the presence of persistent hyperglycaemia glucose This article will briefly describe these processes and will chemically attaches to proteins non-enzymatically to form discuss possible pathogenic interactions which may lead a stable product (keto amine or Amadori product) of which to the development of the pathological lesion. glycosylated haemoglobin is the best-known example. In long-lived tissue proteins such as collagen the ketoamine Microangiopathy is a specific disorder of the small blood then undergoes a series of reactions resulting in the vessels which causes much morbidity and mortality in dia development of advanced glycosylation end products betic patients. Diabetic retinopathy is the commonest (AGE) (Fig. 1).5 AGE are resistant to degradation and con cause of blindness in the working population of the United tinue to accumulate indefinitely on long-lived proteins. -
Anti-Thrombotics in Stroke When to Start and When to Stop
Anti-Thrombotics In Stroke when to start and when to stop Ania Busza MD PhD Assistant Professor of Neurology University of Rochester School of Medicine and Dentistry No Relevent Disclosures • Research funding from NIH/NICHD (K12 award) • Materials provided for research from MC10, Inc This person was He has afib but was Outlinedischarged 1 week discharged only on ago with a subdural. aspirin – when Should they be back My patient is should I restart his on aspirin? currently on warfarin anticoagulation ? but wants to get pregnant. Is that Common questions that arise post-Stroke safe? Why is everyone The report says talking about putting “likely amyloid TIA patients on angiopathy” – what BOTH aspirin and do I do about their plavix for a few antithrombotics? weeks? Outline ? • Physiology – types of clots and the logic behind the different choices for antithrombotic therapy • Timing: When should antithrombotics be started… – after an ischemic stroke? ? ? – after a hemorrhagic stroke? • Safety: What to consider in selecting antithrombotic therapy – in pregnancy – in patients with cerebral amyloid angiopathy ? • DAPT: When is duo-antiplatelet treatment indicated? Physiology of Clots thrombosis - an obstruction of blood flow due to a localized occlusive process within one more more blood vessels. Physiology of Clots RED THROMBI WHITE THROMBI RED THROMBI • Erythrocytes + Fibrin • tend to develop in low flow situations: – dilated cardiac atria / afib – regions of ventricular hypokinesia (ventricular aneurysms, low EF, or MI) – leg/pelvic veins -

The Increasing Impact of Cerebral Amyloid Angiopathy: Essential New
JNNP Online First, published on August 26, 2017 as 10.1136/jnnp-2016-314697 Cerebrovascular disease J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2016-314697 on 26 August 2017. Downloaded from REVIEW The increasing impact of cerebral amyloid angiopathy: essential new insights for clinical practice Gargi Banerjee,1 Roxana Carare,2 Charlotte Cordonnier,3 Steven M Greenberg,4 Julie A Schneider,5 Eric E Smith,6 Mark van Buchem,7 Jeroen van der Grond,7 Marcel M Verbeek,8,9 David J Werring1 For numbered affiliations see ABSTRact Furthermore, CAA gained new relevance with the end of article. Cerebral amyloid angiopathy (CAA) has never been advent of anti-Aβ immunotherapies for the treat- more relevant. The last 5 years have seen a rapid ment of Alzheimer’s disease (AD), as a sizeable Correspondence to increase in publications and research in the field, with proportion of those treated went on to develop Dr David J Werring, The National Hospital for Neurology and the development of new biomarkers for the disease, imaging features of CAA-related inflammation as 5 Neurosurgery, UCL Institute thanks to advances in MRI, amyloid positron emission an unintended consequence. This, together with of Neurology, Queen Square, tomography and cerebrospinal fluid biomarker analysis. advances in our understanding of the impact of London WC1N 3BG, UK; d. The inadvertent development of CAA-like pathology CAA on cognition, in the context of ICH, ageing werring@ ucl. ac. uk in patients treated with amyloid-beta immunotherapy and AD, has broadened the clinical spectrum Received 1 March 2017 for Alzheimer’s disease has highlighted the importance of disease to which the contribution of CAA is Revised 26 April 2017 of establishing how and why CAA develops; without recognised. -

Dipeptidase Aminodipeptidase, Quiescent Cell Proline of a Novel
Vesicular Localization and Characterization of a Novel Post-Proline-Cleaving Aminodipeptidase, Quiescent Cell Proline Dipeptidase This information is current as of September 26, 2021. Murali Chiravuri, Fernando Agarraberes, Suzanne L. Mathieu, Henry Lee and Brigitte T. Huber J Immunol 2000; 165:5695-5702; ; doi: 10.4049/jimmunol.165.10.5695 http://www.jimmunol.org/content/165/10/5695 Downloaded from References This article cites 28 articles, 18 of which you can access for free at: http://www.jimmunol.org/content/165/10/5695.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Vesicular Localization and Characterization of a Novel Post-Proline-Cleaving Aminodipeptidase, Quiescent Cell Proline Dipeptidase1 Murali Chiravuri,* Fernando Agarraberes,† Suzanne L. Mathieu,* Henry Lee,* and Brigitte T. Huber2* A large number of chemokines, cytokines, and signal peptides share a highly conserved X-Pro motif on the N-terminus. -

From Brain to Heart: Possible Role of Amyloid-Β in Ischemic Heart Disease and Ischemia-Reperfusion Injury
International Journal of Molecular Sciences Review From Brain to Heart: Possible Role of Amyloid-β in Ischemic Heart Disease and Ischemia-Reperfusion Injury Giulia Gagno 1, Federico Ferro 1, Alessandra Lucia Fluca 1, Milijana Janjusevic 1, Maddalena Rossi 1, Gianfranco Sinagra 1, Antonio Paolo Beltrami 2 , Rita Moretti 3 and Aneta Aleksova 1,* 1 Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina (ASUGI) and University of Trieste, 34100 Trieste, Italy; [email protected] (G.G.); ff[email protected] (F.F.); alessandrafl[email protected] (A.L.F.); [email protected] (M.J.); [email protected] (M.R.); [email protected] (G.S.) 2 Department of Medicine (DAME), University of Udine, 33100 Udine, Italy; [email protected] 3 Department of Internal Medicine and Neurology, Neurological Clinic, 34100 Trieste, Italy; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +39-340-550-7762 Received: 3 December 2020; Accepted: 14 December 2020; Published: 17 December 2020 Abstract: Ischemic heart disease (IHD) is among the leading causes of death in developed countries. Its pathological origin is traced back to coronary atherosclerosis, a lipid-driven immuno-inflammatory disease of the arteries that leads to multifocal plaque development. The primary clinical manifestation of IHD is acute myocardial infarction (AMI),) whose prognosis is ameliorated with optimal timing of revascularization. Paradoxically, myocardium re-perfusion can be detrimental because of ischemia-reperfusion injury (IRI), an oxidative-driven process that damages other organs. Amyloid-β (Aβ) plays a physiological role in the central nervous system (CNS). Alterations in its synthesis, concentration and clearance have been connected to several pathologies, such as Alzheimer’s disease (AD) and cerebral amyloid angiopathy (CAA).