Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Isolated Acrania in the Presence of Amniotic Band Syndrome
100 Jul 2017 Vol 10 No.3 North American Journal of Medicine and Science Case Report Isolated Acrania in the Presence of Amniotic Band Syndrome Lei Li, MD, PhD; Sandra Cerda, MD; David Kindelberger, MD; Jing Yang, MD, PhD; Carmen Sarita-Reyes, MD* Department of Pathology and Laboratory Medicine, Boston Medical Center, Boston, MA Acrania is an extremely rare congenital developmental anomaly. It is often confused with another disease entity, anencephaly. Even though these two developmental defects often occur simultaneously, they are believed to have different pathogenic mechanisms. We report the case of a 22-year-old woman with an unremarkable first trimester pregnancy who delivered a demised male fetus at 16 weeks gestation. External and microscopic examination of the fetus revealed normal development in all internal organs. The brain was covered by leptomeninges only, with an absence of skull and overlying skin. Additionally, both the fetus and placenta showed evidence of amniotic band syndrome. A diagnosis of isolated acrania in the presence of amniotic band syndrome was made. The exact etiology of acrania is not well understood. Two popular theories suggest that amniotic bands or a migration failure of the ectodermal mesenchyme may play a role in the pathogenesis. We believe that isolated acrania may represent a group of developmental anomalies which share a common ultimate outcome: absence of the neurocranium with relatively minor effects on brain development. [N A J Med Sci. 2017;10(3):100-102. DOI: 10.7156/najms.2017.1003100] Key Words: acrania, anencephaly, acalvaria, amniotic band syndrome INTRODUCTION Acrania is an extremely rare lethal embryonic developmental current smoker. -

Acalvaria: Case Report and Review of Literature of a Rare
DOI: 10.7860/JCDR/2018/35736.11530 Case Report Acalvaria: Case Report and Review of Literature of a Rare Paediatrics Section Congenital Malformation DEEKSHA ANAND SINGLA1, ANAND SINGLA2 ABSTRACT Acalvaria, defined as absent skull bones, is an extremely rare congenital anomaly with only a handful of cases reported in literature. Hypocalvaria is its hypoplastic variant where the skull bones are incompletely formed. Due to such a rare incidence, it has been given the status of an orphan disease. In this report we present the case of a female neonate with acalvaria born in our institute. The neonate survived a short and stormy course of 12 days as she also had associated co-morbidities. The condition per se has been described as having high mortality rate. Very few living cases, less than ten have been reported till date. Keywords: Absent skull bones, Hypocalvaria, Orphan disease CASE REPORT admitted in view of bad obstetric history. An emergency cesarean The baby (female) was born to a 25-year-old female by non section had to be undertaken as she developed fetal distress. consanguineous marriage through spontaneous conception. The The index female neonate was born by caesarean section at 34 birth order of the baby was fifth and the only surviving sibling was a weeks of gestation. APGAR Score at one and five minutes was nine five-year-old female. The first baby was a male, born 10 years back each. The heart rate was 142 beats per minute, respiratory rate through normal vaginal delivery who died at 1.5 months of age, was 66 breaths per minute with mild subcostal and intercostals the cause of death was unknown to the parents. -

Imaging Surgical Epilepsy in Children
Childs Nerv Syst (2006) 22:786–809 DOI 10.1007/s00381-006-0132-5 SPECIAL ANNUAL ISSUE Imaging surgical epilepsy in children Charles Raybaud & Manohar Shroff & James T. Rutka & Sylvester H. Chuang Received: 1 February 2006 / Published online: 13 June 2006 # Springer-Verlag 2006 Abstract of the diverse pathologies concerned with epilepsy surgery in Introduction Epilepsy surgery rests heavily upon magnetic the pediatric context is provided with illustrative images. resonance imaging (MRI). Technical developments have brought significantly improved efficacy of MR imaging in Keywords MR imaging . Epilepsy. Ganglioglioma . DNT. detecting and assessing surgical epileptogenic lesions, PXA . FCD . Hypothalamic hamartoma . while more clinical experience has brought better definition Meningioangiomatosis of the pathological groups. Discussion MRI is fairly efficient in identifying develop- mental, epilepsy-associated tumors such as ganglioglioma Introduction (with its variants gangliocytoma and desmoplastic infantile ganglioglioma), the complex, simple and nonspecific forms Epilepsy surgery in children addresses severe refractory of dysembryoplastic neuroepithelial tumor, and the rare epilepsy mainly, which threatens the child’s development, pleomorphic xanthoastrocytoma. The efficacy of MR when a constant epileptogenic focus can be identified from imaging is not as good for the diagnosis of focal cortical the clinical and the electroencephalogram (EEG) data and be dysplasia (FCD), as it does not necessarily correlate with removed. Imaging must demonstrate -
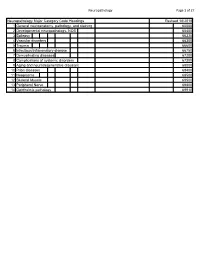
Neuropathology Category Code List
Neuropathology Page 1 of 27 Neuropathology Major Category Code Headings Revised 10/2018 1 General neuroanatomy, pathology, and staining 65000 2 Developmental neuropathology, NOS 65400 3 Epilepsy 66230 4 Vascular disorders 66300 5 Trauma 66600 6 Infectious/inflammatory disease 66750 7 Demyelinating diseases 67200 8 Complications of systemic disorders 67300 9 Aging and neurodegenerative diseases 68000 10 Prion diseases 68400 11 Neoplasms 68500 12 Skeletal Muscle 69500 13 Peripheral Nerve 69800 14 Ophthalmic pathology 69910 Neuropathology Page 2 of 27 Neuropathology 1 General neuroanatomy, pathology, and staining 65000 A Neuroanatomy, NOS 65010 1 Neocortex 65011 2 White matter 65012 3 Entorhinal cortex/hippocampus 65013 4 Deep (basal) nuclei 65014 5 Brain stem 65015 6 Cerebellum 65016 7 Spinal cord 65017 8 Pituitary 65018 9 Pineal 65019 10 Tracts 65020 11 Vascular supply 65021 12 Notochord 65022 B Cell types 65030 1 Neurons 65031 2 Astrocytes 65032 3 Oligodendroglia 65033 4 Ependyma 65034 5 Microglia and mononuclear cells 65035 6 Choroid plexus 65036 7 Meninges 65037 8 Blood vessels 65038 C Cerebrospinal fluid 65045 D Pathologic responses in neurons and axons 65050 1 Axonal degeneration/spheroid/reaction 65051 2 Central chromatolysis 65052 3 Tract degeneration 65053 4 Swollen/ballooned neurons 65054 5 Trans-synaptic neuronal degeneration 65055 6 Olivary hypertrophy 65056 7 Acute ischemic (hypoxic) cell change 65057 8 Apoptosis 65058 9 Protein aggregation 65059 10 Protein degradation/ubiquitin pathway 65060 E Neuronal nuclear inclusions 65100 -

Instelling Naam Expertise Centrum Cluster Van / Specifieke Aandoening Toelichting Erkenning
Instelling Naam Expertise Centrum Cluster van / Specifieke aandoening Toelichting erkenning AMC Amsterdam Lysosome Center Gaucher disease ("Sphinx") Fabry disease Niemann-Pick disease type A Niemann-Pick disease type B Niemann-Pick disease type C Mucopolysaccharidosis type 1 Mucopolysaccharidosis type 3 Mucopolysaccharidosis type 4 Lysosomal Disease Cholesteryl ester storage disease AMC Dutch Centre for Peroxisomal Peroxisome biogenesis disorder-Zellweger syndrome spectrum disorders Disorder of peroxisomal alpha- - beta- and omega-oxidation Rhizomelic chondrodysplasia punctata Non-syndromic pontocerebellar hypoplasia AMC Expertise center Vascular medicine Homozygous familial hypercholesterolemia Familial lipoprotein lipase deficiency Tangier disease AMC Centre for Genetic Metabolic Disorder of galactose metabolism Diseases Amsterdam Disorder of phenylalanine metabolism AMC Centre for Neuromuscular Diseases Neuromuscular disease Motor neuron disease; amyotrophic lateral sclerosis, primary sclerosis and progressive muscular atrophy Idiopathic inflammatory myopathy, incl dermatomyositis, polymyositis, necrotizing autoimmune myopathy and inclusion body myositis Poliomyelitis Hereditary motor and sensory neuropathy Chronic inflammatory demyelinating polyneuropathy, incl. Guillain_Barre syndrome, CIDP, MMN AMC Centre for rare thyroid diseases Congenital hypothyroidism AMC Centre for gastroenteropancreatic Gastroenteropancreatic endocrine tumor neuroendocrine tumors AMC Centre for rare hypothalamic and Rare hypothalamic or pituitary disease pituitary -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Diffusion Weighted Imaging in Pediatric Neuroradiology Massachusetts General Hospital, Boston, MA • Harvard Medical School, Boston, MA
Pallavi Sagar, M.D.; P. Ellen Grant, M.D. Diffusion Weighted Imaging in Pediatric Neuroradiology Massachusetts General Hospital, Boston, MA • Harvard Medical School, Boston, MA I. CEREBROVASCULAR DISEASE IV. TOXIC AND METABOLIC DISORDERS V. DEMYELINATING DISORDERS 1) Arterial Ischemic Stroke (AIS) 3) Global Hypoxia and Hypoperfusion 1) Methotrexate Neurotoxicity 1) Multiple Sclerosis (MS) INTRODUCTION Pediatric AIS is less common and almost 50% of the pediatric AIS are Perinatal Hypoxic Ischemic Brain Injury Intrathecal or intravenous methotrexate can cross blood brain barrier and cause diffuse or multifocal Figure 9. Methotrexate toxicity. Axial (a) T2 and (b) DWI. There is MS is an inflammatory demyelinating process, Diffusion-weighted magnetic resonance idiopathic. Pediatric strokes can be classified as perinatal (between 28 weeks white matter changes typically in the periventricular region. Alteration in myelin metabolism faint T2 hyperintensity in the left posterior centrum semiovale. which can be reversible due to reparative imaging (DWI) provides image contrast DWI is more sensitive in demonstrating increased signal in this of gestation and 28 days of postnatal life) or childhood (between 30 days and Hypoxic ischemic brain injury results from a combination of global cerebral hypoxia and hypoperfusion. Two patterns have causing axonal swelling and intramyelinic edema has been proposed. In acute encephalopathy region and an additional lesion on the right side presumably remyelination or become irreversible with that is dependent on the molecular motion 18 year of life) ( Figure 1) . been described. Partial asphyxia or peripheral pattern with bilateral white matter injury and a profound or central pattern with transient and reversible lesions with decreased diffusion can be observed. -
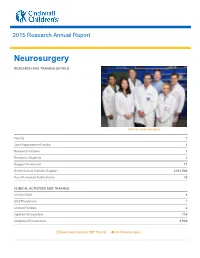
Neurosurgery
2015 Research Annual Report Neurosurgery RESEARCH AND TRAINING DETAILS Click to view members Faculty 7 Joint Appointment Faculty 4 Research Fellows 1 Research Students 2 Support Personnel 11 Direct Annual Industry Support $292,544 Peer Reviewed Publications 20 CLINICAL ACTIVITIES AND TRAINING Clinical Staff 8 Staff Physicians 7 Clinical Fellows 2 Inpatient Encounters 716 Outpatient Encounters 3,908 Download Report in PDF Format Visit Neurosurgery Research Highlights Research Highlights Diverse, Collaborative Clinical and Research Activities The surgical treatment of intractable epilepsy in children, and finding new ways to improve outcomes, remains our division’s primary focus. Division Chief Francesco Mangano, DO, FACS, FACOS, is coprincipal investigator with Weihong Yuan, PhD, Department of Radiology, on a study of advanced MR imaging techniques in the field of hydrocephalus. Work from this multiinstitutional study was published internationally. Collaborating with physicians in medical neurooncology and radiation oncology, Charles Stevenson, MD, leads the division’s brain tumor program. As a member institution of the Pediatric Brain Tumor Consortium (PBTC), Cincinnati Children’s continues to innovate in clinical trials related to brain cancer. In one recent trial sponsored by the National Cancer Institute and PBTC, a special virus designed to kill tumor cells but not affect normal cells was injected into malignant brain tumors that defy chemotherapy and radiation therapy. Cincinnati Children’s is the only pediatric hospital in the U.S. approved for this treatment. Stevenson, with colleagues in the Divisions of Pediatric Physical Medicine and Rehabilitation and Physical Therapy, launched a multidisciplinary surgical spasticity clinic which focuses on early identification of patients with cerebral palsy and spinal cord injury. -

Os Odontoideum As a Cause of Cervical Cord Injury in a Patient with Refractory Epilepsy
Case Report Clinics in Surgery Published: 09 Feb, 2021 Os Odontoideum as a Cause of Cervical Cord Injury in a Patient with Refractory Epilepsy Shohei Kusabiraki1, Eiji Nakagawa1*, Takashi Saito1, Yutaro Takayama2, Keiya Iijima2, Masaki Iwasaki2, Ayano Matsui3 and Tetsuya Abe4 1Department of Child Neurology, National Center Hospital, NCNP, Japan 2Department of Neurosurgery, National Center Hospital, Japan 3Department of Orthopedics, National Center Hospital, Japan 4Department of Orthopedic Surgery, University of Tsukuba, Japan Abstract Os odontoideum is an anomaly of the second cervical vertebrae in which the odontoid process is separated from the body of the axis. Traumatic injury or congenital fusion failure is thought to be the etiology. The clinical symptoms are variable from cervical pain, torticollis, and myelopathy and vertebrobasilar ischemia. Os odontoideum can cause instability of the neck, and neck injuries can cause life-threatening complications. In this report, we present the case of a 15-year-old girl with refractory epilepsy who developed quadriparesis after a fall and hit to the forehead while traveling. Although the symptoms improved, weakness in her right upper limb persisted at 2 months after the fall. Imaging studies revealed Os odontoideum. Based on her medical history, the recent head trauma due to epileptic seizures accompanied by atlantoaxial instability was considered to result in cervical compression and spinal damage. She was at a high risk of sudden death due to recurrent seizures and cervical injury; therefore, -

UC San Francisco Previously Published Works
UCSF UC San Francisco Previously Published Works Title A pictorial review of the pathophysiology and classification of the magnetic resonance imaging patterns of perinatal term hypoxic ischemic brain injury - What the radiologist needs to know…. Permalink https://escholarship.org/uc/item/0s5968ds Journal SA journal of radiology, 24(1) ISSN 1027-202X Authors Misser, Shalendra K Barkovich, Anthony J Lotz, Jan W et al. Publication Date 2020 DOI 10.4102/sajr.v24i1.1915 Peer reviewed eScholarship.org Powered by the California Digital Library University of California SA Journal of Radiology ISSN: (Online) 2078-6778, (Print) 1027-202X Page 1 of 17 Pictorial Review A pictorial review of the pathophysiology and classification of the magnetic resonance imaging patterns of perinatal term hypoxic ischemic brain injury – What the radiologist needs to know… Authors: This article provides a correlation of the pathophysiology and magnetic resonance imaging 1,2 Shalendra K. Misser (MRI) patterns identified on imaging of children with hypoxic ischemic brain injury (HIBI). Anthony J. Barkovich3 Jan W. Lotz4 The purpose of this pictorial review is to empower the reading radiologist with a simplified Moherndran Archary5 classification of the patterns of cerebral injury matched to images of patients demonstrating each subtype. A background narrative literature review was undertaken of the regional, Affiliations: continental and international databases looking at specific patterns of cerebral injury related to 1Department of Radiology, Faculty of Health Sciences perinatal HIBI. In addition, a database of MRI studies accumulated over a decade (including a Medicine, College of Health total of 314 studies) was analysed and subclassified into the various patterns of cerebral injury. -

Birth Defects Surveillance a Manual for Programme Managers
BIRTH DEFECTS SURVEILLANCE A MANUAL FOR PROGRAMME MANAGERS Birth defects surveillance: a manual for programme managers i WHO I CDC I ICBDSR WHO I CDC I ICBDSR ii Birth defects surveillance: a manual for programme managers BIRTH DEFECTS SURVEILLANCE A MANUAL FOR PROGRAMME MANAGERS Birth defects surveillance: a manual for programme managers i WHO I CDC I ICBDSR WHO Library Cataloguing-in-Publication Data Birth defects surveillance: a manual for programme managers. 1.Congenital abnormalities – epidemiology. 2.Congenital abnormalities – prevention and control. 3.Neural tube defects. 4.Public health surveillance. 5.Developing countries. I.World Health Organization. II.Centers for Disease Control and Prevention (U.S.). III.International Clearinghouse for Birth Defects Monitoring Systems. ISBN 978 92 4 154872 4 NLM classification: QS 675 © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non- commercial distribution– should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -
The Role of Inhibitory Interneurons in a Model Od Developmental Epilepsy
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2007 The Role of Inhibitory Interneurons in a Model od Developmental Epilepsy Patrick James Wolfgang Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Nervous System Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/1145 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. © Patrick James Wolfgang 2007 All Rights Reserved THE ROLE OF INHIBITORY INTERNEURONS IN A MODEL OF DEVELOPMENTAL EPILEPSY A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science in Anatomy and Neurobiology at Virginia Commonwealth University. by PATRICK JAMES WOLFGANG BA Environmental Science, University of Virginia, 2005 Director: KIMBERLE JACOBS ASSISTANT PROFESSOR ANATOMY AND NEUROBIOLOGY Virginia Commonwealth University Richmond, Virginia August, 2007 ii Acknowledgement First, I would like to thank my parents for their support over the last 25 years. I would also like to thank Dr. Jacobs for her support and guidance during the year. I would also like to extend a sincere thanks to Amanda Lynn George (AKA Mandy 5 or the MD/PhDbot) for keeping me sane as the year progressed. I expect to see your name quite a bit in future publications. I would also like to thank everyone else who has supported me over the years: Michael, Katie, Matthew, Matt, Rob, Hatcher, Tommy, The other Tommy, Patrick, Lauren, Teo, Cara, Shep, Alex, Jamie, Malcolm, Kelly, Shep, Moo, Markowitz, Matt, Jordan, Tina, Kim, Anya, Melissa, Lynn, Sue, all of my teachers, Bam Bam, Grace, the whole Mendez family, the Longos, the Estes, Ms.