Acute and Chronic Inflammation Yasmin Thanavala, Ph.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Influence of Infection and Inflammation on Biomarkers of Nutritional Status
A2.4 INFLUENCE OF INFECTION AND INFLAMMATION ON BIOMARKERS OF NUTRITIONAL STATUS A2.4 Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron David I. Thurnham1 and George P. McCabe2 1 Northern Ireland Centre for Food and Health, University of Ulster, Coleraine, United Kingdom of Great Britain and Northern Ireland 2 Statistics Department, Purdue University, West Lafayette, Indiana, United States of America Corresponding author: David I. Thurnham; [email protected] Suggested citation: Thurnham DI, McCabe GP. Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron. In: World Health Organization. Report: Priorities in the assessment of vitamin A and iron status in populations, Panama City, Panama, 15–17 September 2010. Geneva, World Health Organization, 2012. Abstract n Many plasma nutrients are influenced by infection or tissue damage. These effects may be passive and the result of changes in blood volume and capillary permeability. They may also be the direct effect of metabolic alterations that depress or increase the concentration of a nutrient or metabolite in the plasma. Where the nutrient or metabolite is a nutritional biomarker as in the case of plasma retinol, a depression in retinol concentrations will result in an overestimate of vitamin A deficiency. In contrast, where the biomarker is increased due to infection as in the case of plasma ferritin concentrations, inflammation will result in an underestimate of iron deficiency. Infection and tissue damage can be recognized by their clinical effects on the body but, unfortunately, subclinical infection or inflammation can only be recognized by measur- ing inflammation biomarkers in the blood. -
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

The Gut Microbiota and Inflammation
International Journal of Environmental Research and Public Health Review The Gut Microbiota and Inflammation: An Overview 1, 2 1, 1, , Zahraa Al Bander *, Marloes Dekker Nitert , Aya Mousa y and Negar Naderpoor * y 1 Monash Centre for Health Research and Implementation, School of Public Health and Preventive Medicine, Monash University, Melbourne 3168, Australia; [email protected] 2 School of Chemistry and Molecular Biosciences, The University of Queensland, Brisbane 4072, Australia; [email protected] * Correspondence: [email protected] (Z.A.B.); [email protected] (N.N.); Tel.: +61-38-572-2896 (N.N.) These authors contributed equally to this work. y Received: 10 September 2020; Accepted: 15 October 2020; Published: 19 October 2020 Abstract: The gut microbiota encompasses a diverse community of bacteria that carry out various functions influencing the overall health of the host. These comprise nutrient metabolism, immune system regulation and natural defence against infection. The presence of certain bacteria is associated with inflammatory molecules that may bring about inflammation in various body tissues. Inflammation underlies many chronic multisystem conditions including obesity, atherosclerosis, type 2 diabetes mellitus and inflammatory bowel disease. Inflammation may be triggered by structural components of the bacteria which can result in a cascade of inflammatory pathways involving interleukins and other cytokines. Similarly, by-products of metabolic processes in bacteria, including some short-chain fatty acids, can play a role in inhibiting inflammatory processes. In this review, we aimed to provide an overview of the relationship between the gut microbiota and inflammatory molecules and to highlight relevant knowledge gaps in this field. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Energy Healing
57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 61 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. CHAPTER 3 Energy Healing Our remedies oft in ourselves do lie. —WILLIAM SHAKESPEARE LEARNING OBJECTIVES 1. Describe the types of energy. 2. Explain the universal energy field (UEF). 3. Explain the human energy field (HEF). 4. Describe the seven auric layers. 5. Describe the seven chakras. 6. Define the concept of energy healing. 7. Describe various types of energy healing. INTRODUCTION For centuries, traditional healers worldwide have practiced methods of energy healing, viewing the body as a complex energy system with energy flowing through or over its surface (Rakel, 2007). Until recently, the Western world largely ignored the Eastern interpretation of humans as energy beings. However, times have changed dramatically and an exciting and promising new branch of academic inquiry and clinical research is opening in the area of energy healing (Oschman, 2000; Trivieri & Anderson, 2002). Scientists and energy therapists around the world have made discoveries that will forever alter our picture of human energetics. The National Institutes of Health (NIH) is conducting research in areas such as energy healing and prayer, and major U.S. academic institutions are conducting large clinical trials in these areas. Approaches in exploring the concepts of life force and healing energy that previously appeared to compete or conflict have now been found to support each other. Conner and Koithan (2006) note 61 57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 62 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. 62 CHAPTER 3 • ENERGY HEALING that “with increased recognition and federal funding for energetic healing, there is a growing body of research that supports the use of energetic healing interventions with patients” (p. -

Purinergic Signalling in Skin
PURINERGIC SIGNALLING IN SKIN AINA VH GREIG MA FRCS Autonomic Neuroscience Institute Royal Free and University College School of Medicine Rowland Hill Street Hampstead London NW3 2PF in the Department of Anatomy and Developmental Biology University College London Gower Street London WCIE 6BT 2002 Thesis Submitted for the Degree of Doctor of Philosophy University of London ProQuest Number: U643205 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest U643205 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 ABSTRACT Purinergic receptors, which bind ATP, are expressed on human cutaneous kératinocytes. Previous work in rat epidermis suggested functional roles of purinergic receptors in the regulation of proliferation, differentiation and apoptosis, for example P2X5 receptors were expressed on kératinocytes undergoing proliferation and differentiation, while P2X? receptors were associated with apoptosis. In this thesis, the aim was to investigate the expression of purinergic receptors in human normal and pathological skin, where the balance between these processes is changed. A study was made of the expression of purinergic receptor subtypes in human adult and fetal skin. -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases
microorganisms Review Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases Juan Alberto Lira-Lucio 1 , Ramcés Falfán-Valencia 1 , Alejandra Ramírez-Venegas 2, Ivette Buendía-Roldán 3 , Jorge Rojas-Serrano 4 , Mayra Mejía 4 and Gloria Pérez-Rubio 1,* 1 HLA Laboratory, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.A.L.-L.); [email protected] (R.F.-V.) 2 Tobacco Smoking and COPD Research Department, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 3 Translational Research Laboratory on Aging and Pulmonary Fibrosis, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 4 Interstitial Lung Disease and Rheumatology Unit, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.R.-S.); [email protected] (M.M.) * Correspondence: [email protected]; Tel.: +52-55-5487-1700 (ext. 5152) Received: 11 June 2020; Accepted: 7 July 2020; Published: 16 July 2020 Abstract: The lung microbiome composition has critical implications in the regulation of innate and adaptive immune responses. Next-generation sequencing techniques have revolutionized the understanding of pulmonary physiology and pathology. Currently, it is clear that the lung is not a sterile place; therefore, the investigation of the participation of the pulmonary microbiome in the presentation, severity, and prognosis of multiple pathologies, such as asthma, chronic obstructive pulmonary disease, and interstitial lung diseases, contributes to a better understanding of the pathophysiology. Dysregulation of microbiota components in the microbiome–host interaction is associated with multiple lung pathologies, severity, and prognosis, making microbiome study a useful tool for the identification of potential therapeutic strategies. -

Cells, Tissues and Organs of the Immune System
Immune Cells and Organs Bonnie Hylander, Ph.D. Aug 29, 2014 Dept of Immunology [email protected] Immune system Purpose/function? • First line of defense= epithelial integrity= skin, mucosal surfaces • Defense against pathogens – Inside cells= kill the infected cell (Viruses) – Systemic= kill- Bacteria, Fungi, Parasites • Two phases of response – Handle the acute infection, keep it from spreading – Prevent future infections We didn’t know…. • What triggers innate immunity- • What mediates communication between innate and adaptive immunity- Bruce A. Beutler Jules A. Hoffmann Ralph M. Steinman Jules A. Hoffmann Bruce A. Beutler Ralph M. Steinman 1996 (fruit flies) 1998 (mice) 1973 Discovered receptor proteins that can Discovered dendritic recognize bacteria and other microorganisms cells “the conductors of as they enter the body, and activate the first the immune system”. line of defense in the immune system, known DC’s activate T-cells as innate immunity. The Immune System “Although the lymphoid system consists of various separate tissues and organs, it functions as a single entity. This is mainly because its principal cellular constituents, lymphocytes, are intrinsically mobile and continuously recirculate in large number between the blood and the lymph by way of the secondary lymphoid tissues… where antigens and antigen-presenting cells are selectively localized.” -Masayuki, Nat Rev Immuno. May 2004 Not all who wander are lost….. Tolkien Lord of the Rings …..some are searching Overview of the Immune System Immune System • Cells – Innate response- several cell types – Adaptive (specific) response- lymphocytes • Organs – Primary where lymphocytes develop/mature – Secondary where mature lymphocytes and antigen presenting cells interact to initiate a specific immune response • Circulatory system- blood • Lymphatic system- lymph Cells= Leukocytes= white blood cells Plasma- with anticoagulant Granulocytes Serum- after coagulation 1. -
Wound Care: the Basics
Wound Care: The Basics Suzann Williams-Rosenthal, RN, MSN, WOC, GNP Norma Branham, RN, MSN, WOC, GNP University of Virginia May, 2010 What Type of Wound is it? How long has it been there? Acute-generally heal in a couple weeks, but can become chronic: Surgical Trauma Chronic -do not heal by normal repair process-takes weeks to months: Vascular-venous stasis, arterial ulcers Pressure ulcers Diabetic foot ulcers (neuropathic) Chronic Wounds Pressure Ulcer Staging Where is it? Where is it located? Use anatomical location-heel, ankle, sacrum, coccyx, etc. Measurements-in centimeters Length X Width X Depth • Length = greatest length (head to toe) • Width = greatest width (side to side) • Depth = measure by marking the depth with a Q- Tip and then hold to a ruler Wound Characteristics: Describe by percentage of each type of tissue: Granulation tissue: • red, cobblestone appearance (healing, filling in) Necrotic: • Slough-yellow, tan dead tissue (devitalized) • Eschar-black/brown necrotic tissue, can be hard or soft Evaluating additional tissue damage: Undermining Separation of tissue from the surface under the edge of the wound • Describe by clock face with patients head at 12 (“undermining is 1 cm from 12 to 4 o’clock”) Tunneling Channel that runs from the wound edge through to other tissue • “tunneling at 9 o’clock, measuring 3 cm long” Wound Drainage and Odor Exudate Fluid from wound • Document the amount, type and odor • Light, moderate, heavy • Drainage can be clear, sanguineous (bloody), serosanguineous (blood-tinged), -
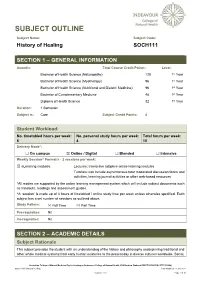
SOCH111 History of Healing Last Modified: 17-Jun-2021
SUBJECT OUTLINE Subject Name: Subject Code: History of Healing SOCH111 SECTION 1 – GENERAL INFORMATION Award/s: Total Course Credit Points: Level: Bachelor of Health Science (Naturopathy) 128 1st Year Bachelor of Health Science (Myotherapy) 96 1st Year Bachelor of Health Science (Nutritional and Dietetic Medicine) 96 1st Year Bachelor of Complementary Medicine 48 1st Year Diploma of Health Science 32 1st Year Duration: 1 Semester Subject is: Core Subject Credit Points: 4 Student Workload: No. timetabled hours per week: No. personal study hours per week: Total hours per week: 6 4 10 Delivery Mode*: ☐ On campus ☒ Online / Digital ☐ Blended ☐ Intensive Weekly Session^ Format/s - 2 sessions per week: ☒ eLearning modules: Lectures: Interactive adaptive online learning modules Tutorials: can include asynchronous tutor moderated discussion forum and activities, learning journal activities or other web-based resources *All modes are supported by the online learning management system which will include subject documents such as handouts, readings and assessment guides. ^A ‘session’ is made up of 3 hours of timetabled / online study time per week unless otherwise specified. Each subject has a set number of sessions as outlined above. Study Pattern: ☒ Full Time ☒ Part Time Pre-requisites: Nil Co-requisites: Nil SECTION 2 – ACADEMIC DETAILS Subject Rationale This subject provides the student with an understanding of the history and philosophy underpinning traditional and other whole medical systems from early human existence to the present day in diverse cultures worldwide. Social, Australian College of Natural Medicine Pty Ltd trading as Endeavour College of Natural Health, FIAFitnation (National CRICOS #00231G, RTO #31489) SOCH111 History of Healing Last modified: 17-Jun-2021 Version: 27.0 Page 1 of 10 cultural and political developments are considered in the evolution of healing and medicine, as well as the parallel developments in anatomy, physiology and other sciences. -

Hormones and the Immune Response
Ann Rheum Dis: first published as 10.1136/ard.48.1.1 on 1 January 1989. Downloaded from Annals of the Rheumatic Diseases, 1989; 48, 1-6 Review Hormones and the immune response Recent advances suggest that the immune system cells, are present on mouse spleen cells3 and human does not function in isolation but is influenced by peripheral blood mononuclear cells.4 Receptors, other physiological systems such as the endocrine identical to those in the central nervous system, for and neuroendocrine systems. This review discusses methionine enkephalin are present on splenocytes aspects of immune function altered by neuroendo- and T lymphocytes.3 In contrast, leucine enkephalin crine peptides, sex hormones, and vitamin D and j3-endorphin receptors on T lymphocyte differ metabolites. from those in the central nervous system as binding cannot be inhibited by opiate antagonists.5 6 In the Neuroendocrine effects case of ,3-endorphin the bindings occur through its carboxy terminal, whereas opiates bind their A system of bidirectional communication between receptor through the amino terminus. This raises the immune and neuroendocrine system exists, in an interesting possibility that a peptide such as which the two systems share a common set of f6-endorphin could form a bridge between two hormones and receptors.'2 Not only do immune lymphocyte subtypes by binding to one through its for peptides, to the and cells possess receptors neuroendocrine amino terminus opiate receptor through copyright. they are also capable of synthesising them and of its carboxy terminus to the non-opiate receptor on responding to them. Products of immune cells affect another lymphocyte.4 the central nervous system, which possesses recep- Other neuroendocrine peptide receptors present tors for cytokines and can also synthesise them on leucocztes include those for neurotensin,7 sub- (Fig.