Screening and Brief Intervention to Reduce Occupational
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

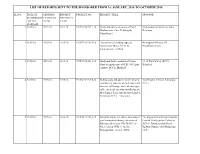
LIST of REPORTS SENT to the SPONSORER from 1ST JANUARY, 2016 to 14Th JULY, 2021
LIST OF REPORTS SENT TO THE SPONSORER FROM 1ST JANUARY, 2016 TO 14th JULY, 2021 SL.NO. DATE OF SENDING PROJECT PROJECT NO. PROJECT TITLE SPONSOR SUBMISSION FINANCIAL FINANCIAL TO THE YEAR YEAR SPONSOR 1 08.01.16 2015-16 2013-14 CNP/3714/2013-14 Study and advice on safety of Patal Archaeological Survey of India, Bhubaneswar Cave Pithoragarh, Dehradun Uttarakhand 2 08.02.16 2015-16 2015-16 CNP/4312/2015-16 Assessment of winding ropes of Narwapahar Mines,UCIL, Narwapahar Mines, UCIL by Singhbhum (East) nondestructive method 3 19.02.16 2015-16 2011-12 CNP/2928/2011-12 Study and failure analysis of 32mm 10/12 Pits Colliery, BCCL, diameter guide rope of K.B. 10/12 pits Dhanbad colliery, BCCL, Dhanbad”. 4 23.03.16 2015-16 2015-16 CNP/4212/2015-16 In-Situ study and advice on the present Asia Resorts Limited, Parwanoo condition of four nos of track ropes and (H.P.) two nos. Of haulage ropes of passenger cable car aerial ropeway installation of M/s Timber Trail, Asia Resorts Limited, Parwanoo (H.P.) – Two visits 5 23.03.16 2015-16 2014-15 CNP/4121/2014-15 Scientific study and advice for status of The Singareni Collieries Company goaf atmosphere during extraction of Limited, Kothagudam Collieries- blasting gallery panel No.BG-J(3) in 507101, Bhadrachalam Road No.3 seam at GDK 11 Incline, Railway Station, Dist-Khammam Ramagundam Area -I, SCCL (A.P.) 6 28.03.16 2015-16 2015-16 CNP/4345/2015-16 Investigation into drop and spark Block II Area, BCCL, Nawagarh, sensitivity of Nonel tubes and VOD, Dhanbad Sensitivity and density parameters of cast boosters involved in the accidental initiation at Amalgamated Block-II OCP 7 05.05.16 2016-17 2010-11 CNP/2859/2010-11 Studies on failure of 25mm diameter Bastacolla Area-IX, BCCL, 6X8 FS construction winding rope of Dhanbad victory 2 pit (south side) Bastacolla Area,”. -

EASTERN COALFIELDS LIMITED (A Subsidiary of Coal India Limited) Office of the General Manager SATGRAM AREA P.O.:-Devchandnagar Dist
EASTERN COALFIELDS LIMITED (A Subsidiary of Coal India Limited) Office of the General Manager SATGRAM AREA P.O.:-Devchandnagar Dist. Burdwan (W.B.) SHORT TENDER NOTICE Ref. No. SAT/ Admn/Hiring-Vehicle/2015/1335 Dated: 12.03.2015 Sealed tenders in Two parts in prescribed form are invited from eligible commercial Light Vehicle Owners having their valid Vehicle Registration Book with commercial Registration Numbers for the following works at Nimcha Colliery under Satgram Area for two years for the period 01.04.2015 to 31.03.2017. Details of engagement of the Vehicles are as under:- Sl.No Specification of Place of No. of Vehicle Estimated E.Money@1% Cost of Vehicle Engagement requirement Cost(SOR) document 01 Light Vehicle, Nimcha 01 RS.3,40,603/- Rs.3,406/- Rs.114.50 BOLERO-Non Colliery A/C under Satgram Area Salient points pertaining to this Tender are furnished below:- 01. Type of Tender :-Tender are invited in Two part system, namely Part-I and Part-II tender. While Part-I tender is meant for Pre-Qualification, Part-II tender will contain price bid only. Part-II tender of only tenderers will be qualified on the basis of credentials submitted in Part-I tender. 02. Period of Contract: -Engagement of standard Vehicles on hire basis by inviting discount bids on SOR from the bidders and concluding contract for 2(Two) years with provision for one year extension at each time up to 2 years on rates, terms, and conditions as per SOR. 03. S.O.R for full deployment of the above two vehicles. -

[email protected] Contact Person Sarda Ruhil
0 June "" List of Laboratories Accredited in Accordance with the Standard ISO/IEC 17025:2017 S. No. Name of the Laboratory & Full address Certificate No Discipline Issue Date Validity Date Validity Extended Upto 1 Quality Control Laboratory, Ordnance Factory, PS‐6 TC‐7549 Chemical 04‐07‐2018 03‐07‐2020 03‐07‐2021 (C3 Area), Tiruchirappalli,TAMIL NADU,INDIA, Mechanical Tiruchirappalli, Tamil Nadu‐620016 Mob: 9942607136 Email: [email protected] Contact Person: G. ASHOK KUMAR 2 Parishil Laboratories Private Limited TC‐7519 Chemical 04‐07‐2018 03‐07‐2020 03‐07‐2021 3rd Floor, Jivabhai Chambers, OPP BATA SHOWROOM,Ahmedabad Gujarat 380009 Ph: 9099980155 Email Id: [email protected] Contact Person MNANDIK TRIVEDI 3 Apex enviro laboratory TC‐7531 Chemical 04‐07‐2018 03‐07‐2020 03‐07‐2021 3, Dhebar Colony, Pratap NagarUdaipur‐ 313001,RAJASTHAN,INDIA UDAIPUR RAJASTHAN 313002 Ph: 9785227837 Email Id: [email protected] Contact Person AMIT SAXENA 4 Centre for Environment and Food technology Pvt. TC‐6145 Biological 04‐07‐2018 03‐07‐2020 03‐07‐2021 Ltd. Chemical 1ST AND 2ND FLOOR , 17 DLF INDUSTRIAL AREA, Delhi New Delhi 110015 Ph: 011‐43216603/45012722, 8178392913 Email Id: [email protected] Contact Person: Madhavi Verma 5 PROCOMM LABORATORIES,NATIONAL BULK TC‐7528 Chemical 04‐07‐2018 03‐07‐2020 03‐07‐2021 HANDLING CORPORATION PRIVATE LIMITED 6/10 Brodipet, D.No. 5‐96‐01Guntur‐522002,ANDHRA PRADESH,INDIA GUNTUR ANDHRA PRADESH 522002 Ph: 7032826723 Email Id: [email protected] Contact Person Y RAJASEKHARAREDDY 6 National Collateral Management Services Limited‐ TC‐7518 Biological 04‐07‐2018 03‐07‐2020 03‐07‐2021 Commgrade, Testing Services, Area Laboratory Chemical Regent Garment & Apparel Park, Block No. -
The Role of Mining Hydrological Investigation with Emphasis on Geophysical Approach to Ascertain Coal Barrier Thickness in Part of Raniganj Coalfield - India
IMWA Proceedings 1998 | © International Mine Water Association 2012 | www.IMWA.info THE ROLE OF MINING HYDROLOGICAL INVESTIGATION WITH EMPHASIS ON GEOPHYSICAL APPROACH TO ASCERTAIN COAL BARRIER THICKNESS IN PART OF RANIGANJ COALFIELD - INDIA. P. K. GUPTA & T. N. SINGH CENTRAL MINING RESEARCH INSTITUTE BARWA ROAD, DHANBAD. 826001 ABSTRACT Underground Mines are the natural non renewable resource base, which sustain the prosperity of region and optimize local resource balance. The conservation and safety of underground mines from minewater inrush point of view, requires concentrated and coordinated efforts toward comprehensive knowledge of mining hydrology. The conceptual mine hydrological modeling is a successful venture and needs to be developed further for minewater flow characterization and minewater prediction rate on regional basis. The introduction of suitable legislation for coal barrier thickness is mandatory for successful underground coal mining operation in river valley. An attempt has been made to determine the critical coal barrier thickness at shallow depth, along partially approachable and largely unapproachable area using geophysical approach under the overall frame of mining hydrologicaly investigation. The study area belongs to the part of Raniganj coalfield, where the coal mining had been introduced in India since 1 ]th century. The study has delineated the critical coal barrier thickness with accuracy +I- 1m in conjunction with horizontal bore hole drilling with regulatory valve system at approachable area, as well as extended to 2unapproachable area. The study leads for provision of optimum minewater column to control over mine fire encroachment at one end, besides to prevent mine water inrush through old water logged portion at under side. -

Meeting of the Standing Committee on Safety in Coal Mines
1 | P a g e 45th MEETING OF THE STANDING COMMITTEE ON SAFETY IN COAL MINES Index Sl. Page Agenda Items No. Nos. 1. In Memoriam 3-6 Agenda Item No.-I 2. Confirmation of the minutes of the 44th meeting of Standing Committee 7-12 on Safety in Coal Mines held on 12.02.2020 Agenda Item No.-II 3. Action Taken Report on the recommendations of the 44th meeting of 13-48 Standing Committee on Safety in Coal Mines held on 12.02.2020 Agenda Item No.-III 4. Details of fatal and serious accidents in between 44th meeting and 45th 49-50 meeting Agenda Item No.-IV 5. 51-62 Details of fatal and serious accidents for last three years and current year Agenda Item No.-V 6. Analysis of major accidents that occurred during last one year and status of 63-64 inquiry & action taken Agenda Item No.-VI 7. 65-76 Risk Assessment & Management Agenda Item No.-VII 8. 77-82 Requirement of statutory manpower and steps taken to fill up the shortage Agenda Item No.-VIII 9. 83-87 Safety Budget and its utilization Agenda Item No.-IX 10. 88-91 Occupational Health Hazards and Health Risk 2 | P a g e In Memoriam STANDING COMMITTEE ON SAFETY IN COAL MINES DEEPLY MOURNS ON THE SAD DEMISE OF THE FOLLOWING BELOVED WORKERS MARTYR OF COAL/LIGNITE COMPANIES AND PAY HOMAGE TO ALL THOSE WHO SACRIFICED THEIR PRECIOUS LIVES FOR THE CAUSE OF THE NATION DURING THE PERIOD BETWEEN THE 44TH(12.02.2020) AND THE 45TH (05.01.2021) MEETINGS OF THE STANDING COMMITTEE ON SAFETY IN COAL MINES 1. -

ANSWERED ON:03.03.2010 ILLEGAL MINING in ASANSOL AREA Chowdhury Shri Bansagopal;Haque Shri Sk
GOVERNMENT OF INDIA COAL LOK SABHA UNSTARRED QUESTION NO:947 ANSWERED ON:03.03.2010 ILLEGAL MINING IN ASANSOL AREA Chowdhury Shri Bansagopal;Haque Shri Sk. Saidul Will the Minister of COAL be pleased to state: (a) whether attention of the Government has been drawn to the on-going-large-scale illegal mining in Asansol-Raniganj- Jharia coal belt areas; (b) if so, the details thereof and the reasons therefor; (c) whether the Government has taken any preventive steps to stop illegal mining with the help from the State Government; (d) if so, the details thereof; and (e) if not, the reasons therefor ? Answer MINISTER OF STATE (IC) IN THE MINISTRY OF COAL AND MINISTER OF STATE (IC) IN THE MINISTRY O F STATISTICS & PROGRAMME IMPLEMENTATION (SHRI SRIPRAKASH JAISWAL) (a)& (b) : Yes, Sir. As per the information received from Coal India Ltd. (CIL), the details of illegal coal mining in Asansol-Raniganj- Jharia coal belt are as under: i) The areas of illegal coal mining activities within the leasehold of Eastern Coalfields Ltd. (ECL), but where the surface rights belong to others, are Sripur area, Sodepur area, Salanpur area, Satgram area, Kenda area, Kunustoria area, Bankola area and Kajora area. ii) In Jharia coal belt, areas of illegal mining activities are Barora, Govindpur, Katras, Sijua, Kusunda, Kustore, Bastacolla, Lodna, E.J. area, W.J. area and C.V. area. The following reasons are attributable to the menace of illegal coal mining: a) Socio-Economic−unemployment, poverty; b) Administrative−innumerable small pockets spread over vast coalfield area; c) Geological − easy access to coal with very low cover; d) Economic − demand from end-users, willing to pay good price; e) Legal action against offenders-time consuming; and f) Landlessness/marginal land holding. -
Eastern Coalfields Limited (A Subsidiary of Coal India Ltd.)
HALF YEARLY ENVIRONMENT CLEARANCE COMPLIANCE REPORT OF CLUSTER 9 J-11015/38/2011-IA.II(M) FOR THE PERIOD OF OCTOBER 2019 TO MARCH 2020 Eastern Coalfields Limited (A subsidiary of Coal India Ltd.) Satgram Area-Six Monthly EC Compliance Report Eastern Coalfields Limited - Cluster 9 (Oct 19 to Mar 20) Condition no. The maximum production from the mine at any given time shall not exceed the i) limit as prescribed in the EC. Compliance Complied Mine Peak EC Production in MT Production Capacity (Oct 19-Mar 20) in MT (FY (MTPA) 19-20) Ratibati UG 0.04 Production suspended Production suspended Chapuikhas UG& OCP 0.06 0.012085 0.025793 Amritnagar UG 0.60 0.046714 0.097646 Tirat-Kuardih UG & OCP 0.15 Production Production Suspended Suspended Nimcha UG & Amkola 1.43 0.176994 0.335825 /Nimcha OC Patch Ghusick-Musila UG & 1.93 Production Production OC Suspended Suspended Kalipahari UG and OC 0.40 0.045526 0.60081 Jemehari UG 0.04 Production Production Suspended Suspended JK Nagar UG & OC 0.42 0.090793 0.18241 Damara UG 0.05 Production Production Suspended Suspended Mahabir UG& Egara OC 0.38 0.015292 0.021855 Narainkuri OCP (60Ha) 2.50 0 0.058449 Total 8.00 0.387404 1.3722788 Condition no. The validity of the EC is for the life of the mine or as specified in the EIA ii) Notification, 2006, whichever is earlier. Compliance Agreed Condition no. The quality of water should conform to the prescribed standards before iii) discharged into nallahs. Compliance Regular monitoring of Quality of Water is carried out by CMPDIL and found to conform to standards prescribed by CPCB. -

A Demographic Survey and Socio- Economic Study for the Project Affected People
DRAFT REPORT 288888222222225 A Demographic Survey and Socio- economic Study for the Project Affected People (PAP) and NON- PAP People of New Kenda OCP, WEST Burdwan District SUBMITTED BY: Dr. Amitabh Pandey Dr. Parul Rishi Dr. Bal Krishna Upadhyay Dr. Ujjal Sarma SUBMITTED TO: EASTERN COALFIELDS LIMITED, KENDA AREA WEST BURDWAN DISTRICT Indian Institute of Forest Management, P.O. Box 357, Nehru Nagar Bhopal (MP) 462003 1 AKNOWLEDGEMENTS Our team would like to express its sincere gratitude towards the General Manager Kenda area Mr. S.K. Singh, for providing us an opportunity to work with their prestigious institution and also for providing us with all the necessary help, support and guidance for the consultancy project. we would like to express our sincere thanks to the Director, IIFM for his kind support throughout the project. We would like to thank Mr. Uday Shankar Choubey (Agent, Kenda Area), Mr. Indranath Chatterjee (Manager, Kenda Area), Mr. Ashish Kumar (Assistant Manager, Environment officer, Kenda Area) and Mr. Monoj Bhattacharjee for supporting me throughout the field visits and facilitating smooth and productive field work. We are highly indebted to the people of Kenda village for their cooperation and support throughout the study. Amitabh Pandey Parul Rishi B K Upadhyay U K Sarma 2 TABLE OF CONTENTS Contents LIST OF ABBREVIATONS4 ................................................................................................................. 4 EXECUTIVE SUMMARY5 .................................................................................................................. -
20.11.2018 REPORT for WEBSITE.Xlsx
LIST OF REPORTS SENT TO THE SPONSORER FROM 1st JANUARY, 2016 TO OCTOBER'2018 SL.NO. DATE OF SENDING PROJECT PROJECT NO. PROJECT TITLE SPONSOR SUBMISSION FINANCIAL FINANCIAL TO THE YEAR YEAR SPONSOR 1 08.01.16 2015-16 2013-14 CNP/3714/2013-14 Study and advice on safety of Patal Archaeological Survey of India, Bhubaneswar Cave Pithoragarh, Dehradun Uttarakhand 2 08.02.16 2015-16 2015-16 CNP/4312/2015-16 Assessment of winding ropes of Narwapahar Mines,UCIL, Narwapahar Mines, UCIL by Singhbhum (East) nondestructive method 3 19.02.16 2015-16 2011-12 CNP/2928/2011-12 Study and failure analysis of 32mm 10/12 Pits Colliery, BCCL, diameter guide rope of K.B. 10/12 pits Dhanbad colliery, BCCL, Dhanbad”. 4 23.03.16 2015-16 2015-16 CNP/4212/2015-16 In-Situ study and advice on the present Asia Resorts Limited, Parwanoo condition of four nos of track ropes and (H.P.) two nos. Of haulage ropes of passenger cable car aerial ropeway installation of M/s Timber Trail, Asia Resorts Limited, Parwanoo (H.P.) – Two visits 5 23.03.16 2015-16 2014-15 CNP/4121/2014-15 Scientific study and advice for status of The Singareni Collieries Company goaf atmosphere during extraction of Limited, Kothagudam Collieries- blasting gallery panel No.BG-J(3) in 507101, Bhadrachalam Road No.3 seam at GDK 11 Incline, Railway Station, Dist-Khammam Ramagundam Area -I, SCCL (A.P.) 6 28.03.16 2015-16 2015-16 CNP/4345/2015-16 Investigation into drop and spark Block II Area, BCCL, Nawagarh, sensitivity of Nonel tubes and VOD, Dhanbad Sensitivity and density parameters of cast boosters involved in the accidental initiation at Amalgamated Block-II OCP 7 05.05.16 2016-17 2010-11 CNP/2859/2010-11 Studies on failure of 25mm diameter Bastacolla Area-IX, BCCL, 6X8 FS construction winding rope of Dhanbad victory 2 pit (south side) Bastacolla Area,”. -

Annual Report & Accounts 2019-20
Eastern Coalfields Limited (A subsidiary of Coal India Limited) ANNUAL REPORT & ACCOUNTS 2019-20 EASTERN COALFIELDS LIMITED (A subsidiary of Coal India Limited) www.easterncoal.nic.in Mission To produce and market the planned quantity of coal and coal products efficiently and economically in an eco-friendly manner with due regard to safety, conservation and quality. Vision To emerge as a global player in the primary energy sector committed to provide energy security to the country by attaining environmentally & socially sustainable growth through best practices from mine to market. CONTENTS Sl.No. Contents Page No. 1. Management ............................................................................................ 04 2. Bankers/Auditors .................................................................................... 06 3. Notice of Annual General Meeting ........................................................... 08 4. Chairman’s Statement ............................................................................. 11 5. Operational Statistics/Financial Position ................................................. 15 6. Profile of Directors ................................................................................... 33 7. Boards’ Report ......................................................................................... 37 8. Comments of the Comptroller and Auditor General of India .................... 128 9. Auditors Report and Management’s Reply ............................................... 130 10. Balance Sheet -

Of 3 OFFICEORDER Consequent Upon the Recommendation of the Departmental Selection Committee, the Competent Au
Page 1 of 3 ईट셍न कोलफील्ड्स लललिटेड EASTERN COALFIELDS LIMITED कोल इंडिया का एक अंग (A Subsidiary of Coal India Limited) अध्यक्ष- सह प्रबन्धक निर्देशक का कायाालय, Office of the Chairman-Cum-Managing Director, सं啍टोरिया, पो-दर्दशेिगढ़, जिला-वधामाि, Sanctoria, PO: Dishergarh, Dist. Burdwan. West Bengal - 713333. पजचिम बंगाल-713333 Office of the General Manager (P&IR). महाप्रबंधक(का/औ.स.) का कायाालय CIN-U10101WB1975GOI030295. CIN-U10101WB1975GOI030295. Telefax- 0341-2523586. फ़ै啍स- 0341-2523586. Website: www.easterncoal.gov.in Website: www.easterncoal.gov.in Ref. NO. ECL/CMD/Rectt/SRD/Clerk-17/32/240 Date: 29th May, 2017. O F F I C E O R D E R Consequent upon the recommendation of the Departmental Selection Committee, the Competent Authority has accorded approval for selection of the following employees as “Clerk” Grade-III from amongst the SC/ST eligible departmental candidates of ECL who applied against the notification no: ECL/CMD/Rectt/SRD/Clerk-17/32/2102 dated 07.02.2017 under special drive. On being selected, they are hereby posted in the Areas/Units/Estb. as given against their names: List of SC category candidates Sl. Previous Father’s U. Man ROLL New place of N Name place of Unit Name Caste Name No. NO posting o posting Samiran Lt. Sukumar 1 192231 Jhanjra MIC SC 50521 Jhanjra Area Mondal Monday Lt-Dilip Raju Narsamuda 2 Kumar 190649 Sodepur SC 50612 Sodepur Area Paswan Colliery Paswan Raghunath Lt. Fela Ram 3 132604 Satgram Nimcha SC 50591 ECL,Hq. -
Annual Report & Accounts 2018-19
CENTRAL MINE PLANNING & DESIGN INSTITUTE LIMITED Annual Report & Accounts 2018-19 CENTRAL MINE PLANNING & DESIGN INSTITUTE LIMITED (A SUBSIDIARY OF COAL INDIA LIMITED) A Mini Ratna Company (Cat-I) AN ISO 9001:2015 CERTIFIED GONDWANA PLACE, KANKE ROAD RANCHI - 834 031 CIN: U14292 JH1975 GOI 001223 Website: www.cmpdi.co.in 135 Vision To be the global market leader in an expanding earth resource sector and allied professional activities. Mission To provide total consultancy in coal and mineral exploration, mining, engineering and allied fields as the premier consultant in India and also in the international arena. Management Policy of CMPDIL With a mission of exploration of coal and other mineral resources and providing consultancy in mine planning, design, associated engineering and management systems, CMPDIL, as a premier consultant, strives to be the market leader in the expanding earth resource sector and other professional activities. We are committed to: 1. Continually improve the quality of our consultancy and other support services with due consideration of the environment, information security and energy performance; 2. Protect the environment by minimizing the adverse impact of our activities on it by consistently reducing, reusing and recycling a part of the waste generated; 3. Provide the resources for achieving the objectives and targets of the quality, environment, energy and information security management systems; 4. Protect our information assets from threats and interruptions to maintain business continuity and continually improve information security performance; 5. Comply with the legal and all other applicable requirements. GENERAL NOTE FOR SHAREHOLDERS OF COAL INDIA LIMITED The Annual Accounts of CMPDI would be kept for inspection and also would be available at the Headquarter for providing information to any Shareholder of Coal India Limited on demand.