A Review of the Type-1 Fibrillinopathies: Pathophysiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Marfan Syndrome Precision Panel Overview Indications Clinical Utility
Marfan Syndrome Precision Panel Overview Marfan Syndrome (MFS) is a spectrum of disorders caused by a genetic defect of the connective tissue and it is inherited in an autosomal dominant pattern. Since the connective tissue is the tissue that helps body growth as well as serving as a scaffold for cells and organs, Marfan Syndrome is a pleiotropic syndrome affecting mainly musculoskeletal, cardiac and ocular systems. The most severe of these manifestations include aortic root dilation and dissection, which are responsible for early patient demise. Pregnancy is a time of increased cardiovascular risk for women with Marfan syndrome, so an early diagnosis is key in pregnancy management. The Igenomix Marfan Syndrome Precision Panel can be used to make an accurate and directed diagnosis as well as a differential diagnosis of connective tissue disorders due to their overlapping phenotypic features ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Marfan Syndrome Precision Panel is indicated for those patients with a clinical suspicion or diagnosis with or without the following manifestations: - Subluxation of lenses - Cardiovascular findings: mitral valve prolapse, aortic regurgitation, mitral regurgitation, aortic dilation, dissection or aneurysm - Tall and thin stature - Long fingers and toes - Pectus carinatum or excavatum - Scoliosis - Hypermobile joints - Severe hindfoot valgus Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. Understanding global and molecular functions of fibrillin containing microfibrils for the development of a comprehensive theory of pathogenesis. -

Marfan Syndrome
Marfan Syndrome Marfan syndrome (MFS) is a connective tissue disorder that exhibits a high degree of clinical variability. Clinical symptoms typically involve the cardiovascular, ocular, and skeletal systems. Early diagnosis is crucial for treatment of skeletal, orthopedic, and Tests to Consider cardiovascular abnormalities. The diagnosis of MFS can be made or suspected based on established clinical criteria (see below). MFS is caused by pathogenic variants in the FBN1 Marfan Syndrome (FBN1) Sequencing and gene; however, there is signicant overlap of the clinical features with syndromes caused by Deletion/Duplication 2005584 pathogenic variants in other genes. Method: Polymerase Chain Reaction/Sequencing/Multiplex Ligation-dependent Probe Amplication Preferred test to conrm diagnosis when MFS is Disease Overview strongly suspected by consensus criteria Marfan Syndrome, FBN1 Sequencing Prevalence 2005589 Method: Polymerase Chain Reaction/Sequencing 1/5,000-10,000 Acceptable test to conrm diagnosis for individuals with clinical phenotype of MFS Symptoms Related Tests A clinical diagnosis of MFS in an individual without a family history of MFS (when Shprintzen-Goldberg syndrome [SGS], Loeys-Dietz syndrome [LDS], and Ehlers-Danlos Aortopathy Panel, Sequencing and Deletion/Duplication 2006540 syndrome type IV [EDS IV] have been excluded) is based on the presence of any of the Method: Massively Parallel Sequencing/Exonic following: Oligonucleotide-based CGH Microarray Aortic root dilatation or dissection and ectopia lentis Aortic root dilatation -
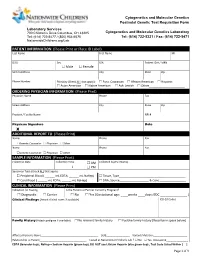
PATIENT INFORMATION (Please Print Or Place ID Label) Last Name First Name MI
Cytogenetics and Molecular Genetics Postnatal Genetic Test Requisition Form Laboratory Services 700 Children’s Drive Columbus, OH 43205 Cytogenetics and Molecular Genetics Laboratory Tel: (614) 722-5477 / (800) 934-6575 Tel: (614) 722-5321 / Fax: (614) 722-5471 NationwideChildrens.org/Lab PATIENT INFORMATION (Please Print or Place ID Label) Last Name First Name MI DOB Sex SSN Patient ID # / MRN Male Female Street Address City State Zip Phone Number Ethnicity (Check ALL that apply): Euro. Caucasian African American Hispanic Asian American Native American Ash. Jewish Other______________________ ORDERING PHYSICIAN INFORMATION (Please Print) Physician Name Phone Fax Street Address City State Zip Practice / Facility Name NPI # Physican Signature Date X ADDITIONAL REPORT TO (Please Print) Name Phone Fax Genetic Counselor Physician Other Name Phone Fax Genetic Counselor Physician Other SAMPLE INFORMATION (Please Print) Collection Date Collection Time AM Collected by (Full Name) : PM Specimen Type (Check ALL that apply): Peripheral Blood ( ______ mL EDTA; ______ mL NaHep) Tissue, Type_________________________________________ Cord Blood ( ______ mL EDTA; ______ mL NaHep) DNA, Source__________________ & Conc.________________ CLINICAL INFORMATION (Please Print) Indication for Testing Is the Patient or Partner Currently Pregnant? Diagnostic Carrier No Yes (Gestational age: ____weeks ____days; EDC _______________ ) Clinical Findings (Attach clinical notes if available) ICD-10 Codes Family History (Attach pedigree if available) -

86A1bedb377096cf412d7e5f593
Contents Gray..................................................................................... Section: Introduction and Diagnosis 1 Introduction to Skin Biology ̈ 1 2 Dermatologic Diagnosis ̈ 16 3 Other Diagnostic Methods ̈ 39 .....................................................................................Blue Section: Dermatologic Diseases 4 Viral Diseases ̈ 53 5 Bacterial Diseases ̈ 73 6 Fungal Diseases ̈ 106 7 Other Infectious Diseases ̈ 122 8 Sexually Transmitted Diseases ̈ 134 9 HIV Infection and AIDS ̈ 155 10 Allergic Diseases ̈ 166 11 Drug Reactions ̈ 179 12 Dermatitis ̈ 190 13 Collagen–Vascular Disorders ̈ 203 14 Autoimmune Bullous Diseases ̈ 229 15 Purpura and Vasculitis ̈ 245 16 Papulosquamous Disorders ̈ 262 17 Granulomatous and Necrobiotic Disorders ̈ 290 18 Dermatoses Caused by Physical and Chemical Agents ̈ 295 19 Metabolic Diseases ̈ 310 20 Pruritus and Prurigo ̈ 328 21 Genodermatoses ̈ 332 22 Disorders of Pigmentation ̈ 371 23 Melanocytic Tumors ̈ 384 24 Cysts and Epidermal Tumors ̈ 407 25 Adnexal Tumors ̈ 424 26 Soft Tissue Tumors ̈ 438 27 Other Cutaneous Tumors ̈ 465 28 Cutaneous Lymphomas and Leukemia ̈ 471 29 Paraneoplastic Disorders ̈ 485 30 Diseases of the Lips and Oral Mucosa ̈ 489 31 Diseases of the Hairs and Scalp ̈ 495 32 Diseases of the Nails ̈ 518 33 Disorders of Sweat Glands ̈ 528 34 Diseases of Sebaceous Glands ̈ 530 35 Diseases of Subcutaneous Fat ̈ 538 36 Anogenital Diseases ̈ 543 37 Phlebology ̈ 552 38 Occupational Dermatoses ̈ 565 39 Skin Diseases in Different Age Groups ̈ 569 40 Psychodermatology -

Scleroderma Mimics - Clinical Features and Management
Mimics of systemic sclerosis and inflammatory muscle disease Scleroderma mimics - clinical features and management Catherine H Orteu1 Voon H. Ong2 Christopher P. Denton2 1Department of Dermatology, Royal Free London NHS Foundation Trust, Pond Street, London NW3 2QG 2Centre for Rheumatology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF Correspondence Professor Christopher Denton Centre for Rheumatology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF [email protected] 1 Mimics of systemic sclerosis and inflammatory muscle disease Scleroderma is often used as a synonym for systemic sclerosis but is perhaps better seen as a collective term covering a range of autoimmune inflammatory conditions in which skin thickening or sclerosis is a hallmark feature. Consensus has emerged that includes localised and systemic forms of scleroderma in a classification that is highlighted in Figure 1. This is sometimes termed the scleroderma spectrum and provides a very useful operational framework for management of the conditions. The term morphoea has recently been applied more consistently to the localised forms of scleroderma and this helps to avoid confusion with patients and clinical staff. There are several other conditions which may be pathogenetically or clinically related to scleroderma that represent diagnostic mimics, and these “pseudo-sclerodermas” are the main focus of this chapter. Establishing the underlying cause and correct diagnosis in a patient with diffuse skin thickening is important because disease impact, prognosis and management vary widely between systemic sclerosis, morphoea and the scleroderma mimics. Practical approach When skin thickening or tightness is observed this should prompt further clinical and laboratory assessment and the tools available generally permit a reliable differentiation between scleroderma and each of the scleroderma mimics. -

Mallory Prelims 27/1/05 1:16 Pm Page I
Mallory Prelims 27/1/05 1:16 pm Page i Illustrated Manual of Pediatric Dermatology Mallory Prelims 27/1/05 1:16 pm Page ii Mallory Prelims 27/1/05 1:16 pm Page iii Illustrated Manual of Pediatric Dermatology Diagnosis and Management Susan Bayliss Mallory MD Professor of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine Director, Pediatric Dermatology St. Louis Children’s Hospital St. Louis, Missouri, USA Alanna Bree MD St. Louis University Director, Pediatric Dermatology Cardinal Glennon Children’s Hospital St. Louis, Missouri, USA Peggy Chern MD Department of Internal Medicine/Division of Dermatology and Department of Pediatrics Washington University School of Medicine St. Louis, Missouri, USA Mallory Prelims 27/1/05 1:16 pm Page iv © 2005 Taylor & Francis, an imprint of the Taylor & Francis Group First published in the United Kingdom in 2005 by Taylor & Francis, an imprint of the Taylor & Francis Group, 2 Park Square, Milton Park Abingdon, Oxon OX14 4RN, UK Tel: +44 (0) 20 7017 6000 Fax: +44 (0) 20 7017 6699 Website: www.tandf.co.uk All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of the publisher or in accordance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any licence permitting limited copying issued by the Copyright Licensing Agency, 90 Tottenham Court Road, London W1P 0LP. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention. -

Skeletal Manifestations of Marfan Syndrome Associated to Heterozygous R2726W FBN1 Variant: Sibling Case Report and Literature Review Octavio D
Reyes-Hernández et al. BMC Musculoskeletal Disorders (2016) 17:79 DOI 10.1186/s12891-016-0935-9 CASE REPORT Open Access Skeletal manifestations of Marfan syndrome associated to heterozygous R2726W FBN1 variant: sibling case report and literature review Octavio D. Reyes-Hernández1†, Carmen Palacios-Reyes1†, Sonia Chávez-Ocaña1, Enoc M. Cortés-Malagón1, Patricia Garcia Alonso-Themann2, Víctor Ramos-Cano3, Julián Ramírez-Bello4 and Mónica Sierra-Martínez1* Abstract Background: FBN1 (15q21.1) encodes fibrillin-1, a large glycoprotein which is a major component of microfibrils that are widely distributed in structural elements of elastic and non-elastic tissues. FBN1 variants are responsible for the related connective tissue disorders, grouped under the generic term of type-1 fibrillinopathies, which include Marfan syndrome (MFS), MASS syndrome (Mitral valve prolapse, Aortic enlargement, Skin and Skeletal findings, Acromicric dysplasia, Familial ectopia lentis, Geleophysic dysplasia 2, Stiff skin syndrome, and dominant Weill-Marchesani syndrome. Case presentation: Two siblings presented with isolated skeletal manifestations of MFS, including severe pectus excavatum, elongated face, scoliosis in one case, and absence of other clinical features according to Ghent criteria diagnosis, were screened for detection of variants in whole FBN1 gene (65 exons). Both individuals were heterozygous for the R2726W variant. This variant has been previously reported in association with some skeletal features of Marfan syndrome in the absence of both tall stature and non-skeletal features. These features are consistent with the presentation of the siblings reported here. Conclusion: The presented cases confirm that the R2726W FBN1 variant is associated with skeletal features of MFS in the absence of cardiac or ocular findings. -

Molecular Genetics of the Fibrillinopathies Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jondeau, Catherine Boileau
Molecular Genetics of the Fibrillinopathies Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jondeau, Catherine Boileau To cite this version: Mélodie Aubart, Louise Benarroch, Pauline Arnaud, Gwenaelle Collod-Beroud, Guillaume Jon- deau, et al.. Molecular Genetics of the Fibrillinopathies. eLS, John Wiley & Sons, 2016, 10.1002/9780470015902.a0025314. hal-01682320 HAL Id: hal-01682320 https://hal-amu.archives-ouvertes.fr/hal-01682320 Submitted on 12 Jan 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Molecular Genetics of Advanced article Article Contents the Fibrillinopathies • Introduction ⋆ • Fibrillins Mélodie Aubart , Laboratory for Vascular Translational Science, INSERM • FBN1 Mutation-Associated Disorders U1148, Paris, France • FBN2-Mutation-Associated Disorders: Congenital Contractural Arachnodactyly (CCA) or Beals Louise Benarroch, Laboratory for Vascular Translational Science, INSERM Syndromes U1148, Paris, France • Animal Models • Pauline Arnaud, Laboratory for Vascular Translational Science, INSERM -

A Case of Myhre Syndrome Mimicking Juvenile Scleroderma Barbara Jensen1*, Rebecca James2, Ying Hong1, Ebun Omoyinmi1, Clarissa Pilkington3, Neil J
Jensen et al. Pediatric Rheumatology (2020) 18:72 https://doi.org/10.1186/s12969-020-00466-1 CASE REPORT Open Access A case of Myhre syndrome mimicking juvenile scleroderma Barbara Jensen1*, Rebecca James2, Ying Hong1, Ebun Omoyinmi1, Clarissa Pilkington3, Neil J. Sebire4, Kevin J. Howell5, Paul A. Brogan1,3 and Despina Eleftheriou1,3,6 Abstract Background: Myhre syndrome is a genetic disorder caused by gain of function mutations in the SMAD Family Member 4 (SMAD4) gene, resulting in progressive, proliferative skin and organ fibrosis. Skin thickening and joint contractures are often the main presenting features of the disease and may be mistaken for juvenile scleroderma. Case presentation: We report a case of a 13 year-old female presenting with widespread skin thickening and joint contractures from infancy. She was diagnosed with diffuse cutaneous systemic sclerosis, and treatment with corticosteroids and subcutaneous methotrexate recommended. There was however disease progression prompting genetic testing. This identified a rare heterozygous pathogenic variant c.1499 T > C (p.Ile500Thr) in the SMAD4 gene, suggesting a diagnosis of Myhre syndrome. Securing a molecular diagnosis in this case allowed the cessation of immunosuppression, thus reducing the burden of unnecessary and potentially harmful treatment, and allowing genetic counselling. Conclusion: Myhre Syndrome is a rare genetic mimic of scleroderma that should be considered alongside several other monogenic diseases presenting with pathological fibrosis from early in life. We highlight this case to provide an overview of these genetic mimics of scleroderma, and highlight the molecular pathways that can lead to pathological fibrosis. This may provide clues to the pathogenesis of sporadic juvenile scleroderma, and could suggest novel therapeutic targets. -

FBN1 Gene Fibrillin 1
FBN1 gene fibrillin 1 Normal Function The FBN1 gene provides instructions for making a large protein called fibrillin-1. This protein is transported out of cells into the extracellular matrix, which is an intricate lattice of proteins and other molecules that forms in the spaces between cells. In this matrix, molecules of fibrillin-1 attach (bind) to each other and to other proteins to form threadlike filaments called microfibrils. Microfibrils form elastic fibers, which enable the skin, ligaments, and blood vessels to stretch. Microfibrils also provide support to more rigid tissues such as bones and the tissues that support the nerves, muscles, and lenses of the eyes. Microfibrils store a protein called transforming growth factor beta (TGF-b ), a critical growth factor. TGF-b affects development by helping to control the growth and division ( proliferation) of cells, the process by which cells mature to carry out specific functions ( differentiation), cell movement (motility), and the self-destruction of cells (apoptosis). Microfibrils help regulate the availability of TGF-b , which is turned off (inactivated) when stored in microfibrils and turned on (activated) when released. Health Conditions Related to Genetic Changes Acromicric dysplasia At least nine FBN1 gene mutations have been identified in people with acromicric dysplasia. This condition is characterized by severely short stature, short limbs, stiff joints, and distinctive facial features. FBN1 gene mutations that cause acromicric dysplasia are located in an area of the gene called exons 41 and 42, and change single protein building blocks (amino acids) in a region of the fibrillin-1 protein called TGF-b binding-protein-like domain 5. -

Medical & Clinical Case Reports
Alina Draga Belengeanu et.al., Ann Case Rep 2018, Volume 3 DOI: 10.29011/2574-7754-C1-006 2nd Global Congress on Medical & Clinical Case Reports November 19–20, 2018 Dubai, UAE New born with progeroid facial features lipodystrophy and marfanoid features - Romanian case 1Alina Draga Belengeanu, 2Daniela Eugenia Popescu, 3Cristina Popescu, 3Silvia Vuculescu and 3Valerica Belengeanu 1"Victor Babes" University of Medicine and Pharmacy, Romania 2Premiere Clinical Hospital Timişoara, Romania 3West University "Vasile Goldis", Arad, Romania Fibrillinopathies are a large heterogeneous group of genetic disorders with distinct effects on differential allelic expression of mutations in the fibrillin-1 gene (FBN1). Different mutations in the gene have been associated with a variety of conditions including Marfan syndrome, MASS syndrome, isolated ectopia lentis syndrome, thoracic aortic aneurysms, WeilleMarchesani syndrome, geleophysic and acromicric dysplasia, and stiff skin syndrome, and Marfan-progeroid-lipodystrophy syndrome. Up to now, seven cases have been reported in the literature, all with a specific gene mutation, type mutation is a truncating mutation in the penultimate exon, i.e., exon 64, in the gene FBN1. Here, we report on a newborn with senile facial appearance with distinctive facial features, with additional manifestations of Marfan syndrome and severe congenital lipodystrophy. The newborn is first child and was born at 39 weeks of gestation to non-consanguineous Caucasian young parents, apparently healthy. The birth weight was 2,600 -

The Ocular Phenotype of Stiff-Skin Syndrome
Eye (2016) 30, 156–159 © 2016 Macmillan Publishers Limited All rights reserved 0950-222X/16 www.nature.com/eye 1 1 2 CASE SERIES The ocular phenotype S Chamney , B Cartmill , O Earley , 3 4 of stiff-skin syndrome V McConnell and CE Willoughby Abstract unaffected son from the sibship. Diagnosis was fi Purpose Stiff skin syndrome (SSS; con rmed at the molecular level using direct MIM#184900) is a rare autosomal dominantly sequencing; all affected family members had a inherited Mendelian disorder characterised by heterozygous FBN1 pathogenic gene mutation 4 thickened and stone-hard indurations of the (c.4710G C; p.Trp1570Cys). Ophthalmic and skin, mild hypertrichosis, and limitation of joint orthoptic examinations were subsequently mobility with flexion contractures. It is completed. autosomal dominant with high penetrance and results from mutations in the fibrillin 1 (FBN1; MIM*134797) gene. Here we present the Case 1: Proband (54-year-old female) associated ocular phenotype in a two generation 1 nonconsanguineous Northern Irish family. This patient wore glasses from the age of 5 years Department of Methods Ophthalmology, Royal The affected patients underwent and had been diagnosed with right amblyopia, Victoria Hospital, Belfast, UK complete ophthalmic and orthoptic which was treated with occlusion therapy. assessment and genetic testing. Aged 51 years, she was diagnosed with bilateral 2 Results Department of All three patients had posterior subcapsular cataracts and had Ophthalmology, Mater ophthalmoplegia of varying degrees. Direct uncomplicated phacoemulsification and Hospital, Belfast, UK FBN1 sequencing of the gene detected a intraocular lens implantation. The left eye was heterozygous pathogenic mutation 3Northern Ireland Regional unexpectedly myopic post-operatively and was (c.4710G4C; p.Trp1570Cys) in all affected Genetics Department, corrected by a LASIK (Laser Assisted in situ Belfast City Hospital, Belfast patients.