WES Gene Package Aneurysm.Xlsx
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reframing Psychiatry for Precision Medicine
Reframing Psychiatry for Precision Medicine Elizabeth B Torres 1,2,3* 1 Rutgers University Department of Psychology; [email protected] 2 Rutgers University Center for Cognitive Science (RUCCS) 3 Rutgers University Computer Science, Center for Biomedicine Imaging and Modelling (CBIM) * Correspondence: [email protected]; Tel.: (011) +858-445-8909 (E.B.T) Supplementary Material Sample Psychological criteria that sidelines sensory motor issues in autism: The ADOS-2 manual [1, 2], under the “Guidelines for Selecting a Module” section states (emphasis added): “Note that the ADOS-2 was developed for and standardized using populations of children and adults without significant sensory and motor impairments. Standardized use of any ADOS-2 module presumes that the individual can walk independently and is free of visual or hearing impairments that could potentially interfere with use of the materials or participation in specific tasks.” Sample Psychiatric criteria from the DSM-5 [3] that does not include sensory-motor issues: A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive, see text): 1. Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions. 2. Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication. -

The Advantage of Genome-Wide Microarrays Over Targeted Approaches
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/70828 Please be advised that this information was generated on 2021-09-24 and may be subject to change. COPY NUMBER VARIATION AND MENTAL RETARDATION opmaak koolen.indd 1 10-09-2008 10:11:31 Copy number variation and mental retardation The studies presented in this thesis were performed at the Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. The research was supported by a grant from the Netherlands Organization for Health Research and Development (ZonMw). Publication of this thesis was financially supported by the Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. ISBN/EAN 978-90-6464-290-6 © 2008 D.A. Koolen All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, by print or otherwise, without permission in writing from the author. Cover photo: Printed by: Ponsen & Looijen B.V., Wageningen opmaak koolen.indd 2 10-09-2008 10:11:31 Copy number variation and mental retardation Een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad doctor aan de Radboud Universiteit Nijmegen op gezag van de rector magnificus prof. mr. S.C.J.J. Kortmann, volgens besluit van het College van Decanen in het openbaar te verdedigen op donderdag 6 november 2008 om 15.30 uur precies door David Aljosja Koolen geboren op 22 juni 1976 te ‘s-Gravenhage opmaak koolen.indd 3 10-09-2008 10:11:32 Promotor: Prof. -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

MED12 Related Disorders FTNW
MED12 related disorders rarechromo.org What are the MED12 related disorders? MED12 related disorders are a group of disorders that primarily affect boys. Most boys with MED12 related disorders have intellectual disability/ developmental delay, behavioural problems and low muscle tone. MED12 related disorders occur when the MED12 gene has lost its normal function. Genes are instructions which have important roles in our growth and development. They are made of DNA and are incorporated into organised structures called chromosomes. Chromosomes therefore contain our genetic information. Chromosomes are located in our cells, the building blocks of our bodies. The MED12 gene is located on the X chromosome. The X chromosome is one of the sex chromosomes that determine a person’s gender. Men have one X chromosome and one Y chromosome, while women have two X chromosomes. Because the MED12 gene is located on the X chromosome, men have only one copy of the gene, while women have two copies. A change in the MED12 gene can cause symptoms in men. Women with a change in the MED12 gene usually have no symptoms. They carry a second copy of the gene that does function normally. Women may show mild features such as learning difficulties. The MED12 related disorders are FG syndrome , Lujan syndrome and the X- linked recessive form of Ohdo syndrome . Although these syndromes differ, they also have the overlapping features listed on page 2. The way that these conditions are inherited is called ‘X-linked’ or ‘X-linked’ recessive. In 2007 it was discovered that changes in the MED12 gene were responsible for the symptoms and features in several boys with FG syndrome. -

Prenatalscreen® Standard Technical Report
About PrenatalScreen® Prenatal Test PrenatalScreen® Prenatal Test is a genetic test that analyses fetal DNA, obtained from CVS or amniotic fluid following an invasive prenatal diagnosis, to screen for monogenic disorders in the fetus. Using the latest technologies, including Next Generation Sequencing (NGS), PrenatalScreen® Prenatal Test screen 744 genes for mutations causing over 1.000 severe genetic disorders in the fetus. PrenatalScreen® Prenatal Test allows for a comprehensive care and enables patients to make more informed reproductive decisions. Offering PrenatalScreen® Prenatal Test to a patient during pregnancy allows her to gain more knowledge about the potential to pass along a condition to the fetus. Aim of the test PrenatalScreen® Prenatal Test analyses DNA extracted from fetal cells in the amniotic fluid, collected through amniocentesis, or in the chorionic villi through villocentesis (CVS). The aim of this diagnositc test is to assess severe genetic diseases in the fetus, including the most common diseases in the European population. Genes listed in Table 1 were selected according to the incidence in the population of the disease caused by mutations in such genes, the severity of the clinical phenotype at birth and the importance of the related pathogenetic picture, in accordance with the indications of the American College of Medical Genetics (ACMG)(Grody et al., Genet Med 2013:15:482–483). PrenatalScreen®: Indication for testing PrenatalScreen® Prenatal Test is intended for patients who meet any of the following criteria: • Personal/familial anamnesis of hereditary genetic diseases; • For expectant mothers wishing to reduce the risk of a genetic diseases in the fetus; • For natural or in vitro fertilization (IVF)-derived pregnancies: • For couples using heterologus IVF procedures (egg/sperm donors). -

Craniosynostosis Precision Panel Overview Indications Clinical Utility
Craniosynostosis Precision Panel Overview Craniosynostosis is defined as the premature fusion of one or more cranial sutures, often resulting in abnormal head shape. It is a developmental craniofacial anomaly resulting from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). As well, craniosynostosis can be simple when only one suture fuses prematurely or complex/compound when there is a premature fusion of multiple sutures. Complex craniosynostosis are usually associated with other body deformities. The main morbidity risk is the elevated intracranial pressure and subsequent brain damage. When left untreated, craniosynostosis can cause serious complications such as developmental delay, facial abnormality, sensory, respiratory and neurological dysfunction, eye anomalies and psychosocial disturbances. In approximately 85% of the cases, this disease is isolated and nonsyndromic. Syndromic craniosynostosis usually present with multiorgan complications. The Igenomix Craniosynostosis Precision Panel can be used to make a directed and accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Craniosynostosis Precision Panel is indicated for those patients with a clinical diagnosis or suspicion with or without the following manifestations: ‐ Microcephaly ‐ Scaphocephaly (elongated head) ‐ Anterior plagiocephaly ‐ Brachycephaly ‐ Torticollis ‐ Frontal bossing Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. - Early initiation of treatment in the form surgical procedures to relieve fused sutures, midface advancement, limited phase of orthodontic treatment and combined 1 orthodontics/orthognathic surgery treatment. -

Characterisation of the MID1/Α4 Multiprotein Complex
Characterisation of the MID1/α4 multiprotein complex INAUGURAL DISSERTATION to obtain doctor rerum naturalium (Dr. rer. nat.) submitted to the Department of Biology, Chemistry and Pharmacy of Freie Universität Berlin by Beatriz Aranda Orgillés Born on 07 November 1976 in Zaragoza, Spain Berlin, April 2006 1. Reviewer: Professor Dr. Susann Schweiger 2. Reviewer: Professor Dr. Volker A. Erdmann Date of defence: To Dirk, Gabriel, Mª Jesús and Ana Table of Contents Table of Contents TABLE OF CONTENTS............................................................................................................1 1 INTRODUCTION...............................................................................................................4 1.1 VENTRAL MIDLINE DEVELOPMENT .................................................................................4 1.1.1 Craniofacial development .....................................................................................7 1.1.2 Heart development ................................................................................................8 1.1.3 Ephrins as NCC pathfinders ................................................................................9 1.1.4 Midline development and disease .......................................................................10 1.2 X-LINKED OPITZ BBB/G SYNDROME (OS) AND MID1................................................11 1.2.1 The RBCC protein MID1.....................................................................................12 1.2.2 The MID1 function ..............................................................................................15 -

Marfan Syndrome Precision Panel Overview Indications Clinical Utility
Marfan Syndrome Precision Panel Overview Marfan Syndrome (MFS) is a spectrum of disorders caused by a genetic defect of the connective tissue and it is inherited in an autosomal dominant pattern. Since the connective tissue is the tissue that helps body growth as well as serving as a scaffold for cells and organs, Marfan Syndrome is a pleiotropic syndrome affecting mainly musculoskeletal, cardiac and ocular systems. The most severe of these manifestations include aortic root dilation and dissection, which are responsible for early patient demise. Pregnancy is a time of increased cardiovascular risk for women with Marfan syndrome, so an early diagnosis is key in pregnancy management. The Igenomix Marfan Syndrome Precision Panel can be used to make an accurate and directed diagnosis as well as a differential diagnosis of connective tissue disorders due to their overlapping phenotypic features ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Marfan Syndrome Precision Panel is indicated for those patients with a clinical suspicion or diagnosis with or without the following manifestations: - Subluxation of lenses - Cardiovascular findings: mitral valve prolapse, aortic regurgitation, mitral regurgitation, aortic dilation, dissection or aneurysm - Tall and thin stature - Long fingers and toes - Pectus carinatum or excavatum - Scoliosis - Hypermobile joints - Severe hindfoot valgus Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. Understanding global and molecular functions of fibrillin containing microfibrils for the development of a comprehensive theory of pathogenesis. -

Marfan Syndrome
Marfan Syndrome Marfan syndrome (MFS) is a connective tissue disorder that exhibits a high degree of clinical variability. Clinical symptoms typically involve the cardiovascular, ocular, and skeletal systems. Early diagnosis is crucial for treatment of skeletal, orthopedic, and Tests to Consider cardiovascular abnormalities. The diagnosis of MFS can be made or suspected based on established clinical criteria (see below). MFS is caused by pathogenic variants in the FBN1 Marfan Syndrome (FBN1) Sequencing and gene; however, there is signicant overlap of the clinical features with syndromes caused by Deletion/Duplication 2005584 pathogenic variants in other genes. Method: Polymerase Chain Reaction/Sequencing/Multiplex Ligation-dependent Probe Amplication Preferred test to conrm diagnosis when MFS is Disease Overview strongly suspected by consensus criteria Marfan Syndrome, FBN1 Sequencing Prevalence 2005589 Method: Polymerase Chain Reaction/Sequencing 1/5,000-10,000 Acceptable test to conrm diagnosis for individuals with clinical phenotype of MFS Symptoms Related Tests A clinical diagnosis of MFS in an individual without a family history of MFS (when Shprintzen-Goldberg syndrome [SGS], Loeys-Dietz syndrome [LDS], and Ehlers-Danlos Aortopathy Panel, Sequencing and Deletion/Duplication 2006540 syndrome type IV [EDS IV] have been excluded) is based on the presence of any of the Method: Massively Parallel Sequencing/Exonic following: Oligonucleotide-based CGH Microarray Aortic root dilatation or dissection and ectopia lentis Aortic root dilatation -

PGD) Considerations on PGD
QiQuestions for the German Council’ s Hearing on Preimplantation Genetic Diagnos is (PGD) Considerations on PGD Prof Dr P Devroey Application Application of PGD (Belgium) z Centre for Medical Genetics (()n: 7) z Centre for Reproductive Medicine (regulated by law) z Psychologist z Ethics Committee J Institutional J Ad Hoc (psychologist, biologist, geneticist, lawyer, paramedical) List List of genetic diseases (PGD) z According a rational approach (prenatal diagnosis) z If an embryo is carrying a given disease z Embryypo is not replaced z ≈ 100 indications z GiGenetic normal embryos are repldlaced according to their morphology Rating : Decision process in transparent PGS vs PGD PGS versus PGD z Preimplantation Genetic Screening (PGS) J Mosaicism J Chromosomal rearrangement Preimplantation aneuploidy screening: a research tool for now Devroey, Lancet 2007 Biopsy of cleavage-stage embryo PGS study < 36 years of age Control PGS No of transfers 89 85 Embryos / transfer mean ± SD 1.0 ± 0.0 1.0 ± 0.0 No of positive HCG 52 47 Positive HCG/OPU 53.1 % 47.0 % NS Positive HCG/ET 58.4 % 55.3 % NS No ongoing pregnancies (> 12 w) 37 37 Ongggpg/oing preg/OPU 37.7 % 37.0 % NS Delivery rate/ET 41.6 % 43.5 % NS Embryos cryopreserved 2.2 ± 2.6 1.4 ± 2.2 P<0.01 Staessen HR 2008 Rating : PGS is research Sequence of embryo replacement decision • Genetic examination • Morphological evaluation • If genetically and morphological normal one embryo is replaced • Supplementary day 5 blastocyst or vitrifyyp for possible later use Rating : decision process is simple -

Whole Exome Sequencing Gene Package Skeletal Dysplasia, Version 2.1, 31-1-2020
Whole Exome Sequencing Gene package Skeletal Dysplasia, Version 2.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCC9 Atrial fibrillation, familial, 12, 614050 601439 65 100 100 95 Cardiomyopathy, dilated, 1O, 608569 Hypertrichotic osteochondrodysplasia, 239850 ACAN Short stature and advanced bone age, with or without early-onset osteoarthritis -
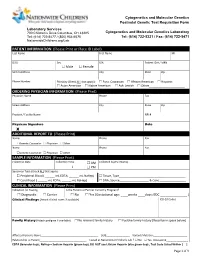
PATIENT INFORMATION (Please Print Or Place ID Label) Last Name First Name MI
Cytogenetics and Molecular Genetics Postnatal Genetic Test Requisition Form Laboratory Services 700 Children’s Drive Columbus, OH 43205 Cytogenetics and Molecular Genetics Laboratory Tel: (614) 722-5477 / (800) 934-6575 Tel: (614) 722-5321 / Fax: (614) 722-5471 NationwideChildrens.org/Lab PATIENT INFORMATION (Please Print or Place ID Label) Last Name First Name MI DOB Sex SSN Patient ID # / MRN Male Female Street Address City State Zip Phone Number Ethnicity (Check ALL that apply): Euro. Caucasian African American Hispanic Asian American Native American Ash. Jewish Other______________________ ORDERING PHYSICIAN INFORMATION (Please Print) Physician Name Phone Fax Street Address City State Zip Practice / Facility Name NPI # Physican Signature Date X ADDITIONAL REPORT TO (Please Print) Name Phone Fax Genetic Counselor Physician Other Name Phone Fax Genetic Counselor Physician Other SAMPLE INFORMATION (Please Print) Collection Date Collection Time AM Collected by (Full Name) : PM Specimen Type (Check ALL that apply): Peripheral Blood ( ______ mL EDTA; ______ mL NaHep) Tissue, Type_________________________________________ Cord Blood ( ______ mL EDTA; ______ mL NaHep) DNA, Source__________________ & Conc.________________ CLINICAL INFORMATION (Please Print) Indication for Testing Is the Patient or Partner Currently Pregnant? Diagnostic Carrier No Yes (Gestational age: ____weeks ____days; EDC _______________ ) Clinical Findings (Attach clinical notes if available) ICD-10 Codes Family History (Attach pedigree if available)